Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Junyang Luo, Mingan Li, Junwei Chen*, Jiesheng Qian and Zaibo Jiang*
Received: July 01, 2018; Published: July 12, 2018
*Corresponding author: Zaibo Jiang, Department of Interventional Radiology, the Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
Junwei Chen, Department of Interventional Radiology, the Third Affiliated Hospital of Sun Yat-Sen University, Guangzhou, China
DOI: 10.26717/BJSTR.2018.06.001393
Ectopic varices (EcVs) are defined as large portosystemic venous collaterals located at sites other than the gastric and esophageal regions. A patient with a bleeding EcVs may present with anemia, shock, hematemesis, melena or hematochezia. Although bleeding EcVs are rare, they should be paid special attention because of their association with high mortality rates. However, optimal treatment for bleeding EcVs remains controversial because of the lack of standardized guidelines and randomized controlled studies. Herein, we report a case of bleeding EcV who was successfully treated with transjugular intrahepatic portosystemic shunt (TIPS) combined with variceal embolization.
Keywords: Portal Hypertension, Ectopic Varices, Endovascular Therapy, Transjugular Intrahepatic Portosystemic Shunt, Embolization
Abbrevations: ECVs:Ectopic Varices,TIPS: Transjugular Intrahepatic Portosystemic Shunt, CT: Computed Tomography
EcVs are defined as large pressurized portosystemic collateral veins in locations other than the gastroesophageal region. As a rare cause of gastrointestinal hemorrhage, EcVs bleeding account for up to 5% of all variceal bleeding and can be difficult to find and control because of the complex etiology and highly variable sites of EcVs. Variable therapeutic approaches, including surgery, endoscopic procedures, and endovascular therapy, have been used to address this condition. Here we report a case of a man with a bleeding EcV who was successfully treated with TIPS combined with variceal embolization.
A 43-year-old male visited an emergency room with massive melena and hematochezia. He had a past medical history of chronic hepatitis B and liver cirrhosis for approximately 6 years and was diagnosed with β-thalassemia for more than 10 years. He had no history of a prior operation. Upon admission, his heart rate was 95 beats/min and blood pressure were 105/55mmHg. Clinical examination revealed an anemic face, palpable spleen and slight jaundice, but he had no asterixis or ascites. Laboratory findings showed a hemoglobin level of 6.0g/dl, a platelet level of 35000/μL, prothrombin time of 21.6 second, a serum albumin level of 2.6g/dl, a total bilirubin level of 2.8mg/dL, a positive hepatitis B surface antigen and a negative hepatitis C antibody. Hepatic function was classified as Child–Pugh Grade B. An emergency upper gastrointestinal endoscopy showed esophageal and gastric fundal varices, but no active source of bleeding was found.
Figure 1A: CT image demonstrates large duodenal varices (white arrow). Esophageal and gastric fundal varices were treated by band ligation and glue injection (black arrow).

Because the varices were thought to be at risk of rupture, band ligation and glue injection were performed. However, a colonoscopy showed fresh blood throughout the colon and no identifiable bleeding point. The persistent hematochezia prompted us to perform abdominal contrast-enhanced abdominal computed tomography (CT) on the patient, which revealed the obliteration of esophageal and gastric fundal varices. Duodenal varices were observed, which were fed by the superior mesenteric vein and communicated to the left renal vein without evidence of extravasation (Figure 1A). Although surgical treatment was initially considered to achieve hemostasis, a limited effect was anticipated because of thrombocytopenia.The combination of TIPS and variceal embolization was chosen to control portal hypertension. Written informed consent was obtained from the patient. All endovascular procedures were conducted in an interventional radiology suite under local anesthesia. Portography via the percutaneous transhepatic approach revealed enlarged duodenal varices with hepatofugal flow (Figure 1B).
Figure 1C: Variceal embolization was successfully performed using coils and glue, and TIPS was performed.
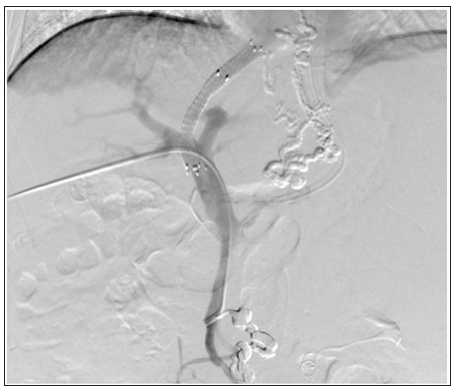
Varices were embolized with a mixture of N-butyl-2- cyanoacrylate (NBCA; Histoacryl, B. Braun, Germany) and iodized oil (Lipiodol; Guerbet, Aulnay-sous-Bois, France), and coils (Cook Medical Inc., USA). Then, TIPS was performed via traditional approach, and one bare metal stent (8mm × 8cm; Luminexx; Bard, Germany) and one covered stent (8mm × 6cm; Fluency Plus; Bard, Germany) were deployed to cover the parenchymal tract (Figure 1C) (as the use of GORE® VIATORR® TIPS Endoprosthesis had not been approved by China Food and Drug Administrationat that time). Finally, portosystemic pressure gradient decreased from 21 to 11mm Hg(Figure 1D). After the procedure, the patient had a stable hemoglobin level and no recurrence of melena or hematochezia and discharged. He remained asymptomatic and the shunt patent during the follow-up of 42months.
Figure 1D: 24 months after the procedure, CT image demonstrates shunt patentcy (black arrow) and obliteration of duodenal varices (white arrow).

EcVs present as large portosystemic venous collaterals located at sites other than the gastric and esophageal regions. Bleeding EcVs may present with anemia, shock, hematemesis, melena or hematochezia. EcVs frequently occur as a consequence of portal hypertension. EcVs are an infrequent cause of gastrointestinal hemorrhage, and they account for up to 5% of all variceal bleeding[1]. Although EcVs are rare, they merit special attention because of their association with high mortality rates. However, optimal treatment of EcVs remains relatively controversial because of the lack of standardized guidelines and randomized controlled studies. In EcVs, 17% were in the duodenum[2]. Thus, an endoscopic approach may be difficult and surgery may not be recommended as many patients have a history of cirrhosis with poor liver function. Endovascular therapy should be considered. TIPS has mainly been used to treat esophagogastric varices secondary to portal hypertension by creating artificial communication between the hepatic and portal veins[3].
As a durable shunt procedure, TIPS can effectively decompress the portal venous system to prevent recurrent vericeal bleeding and the development of new varices elsewhere. There were also some case reports of endovascular therapy for the hemostasis of EcVs [4,5]. However, EcVs may rebleed despite a patent shunt or even a reduction in the portosystemic pressure gradient by 12mmHg or by 25–50% of baseline after TIPS. To minimize rebleeding, the combination of TIPS and variceal embolization has the advantages of being minimally invasive, effective, while not precluding subsequent liver transplantation. In our case, endoscopic and surgical approaches were not feasible. We performed TIPS and variceal embolization concomitantly to achieve complete hemostasis, because the portosystemic pressure gradient was high, and the duodenal varices were large. EcVs, although a rare cause of gastrointestinal hemorrhage, are associated with a high mortality, which may be because they are difficult to diagnose or there are no guidelines for their diagnosis and management. EcVs may result from portal hypertension or other rare causes. Our experience suggest that endovascular therapy could be an optimal treatment for EcVs.
The Science and Technology Planning Project of Guangdong Province, China, No. 2017A020215021.


