Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mwaffaq El Heis*, Maha Gharaibeh, Mammon Al-Omari and Ruba Khasawneh
Received: April 09, 2018; Published: April 17, 2018
*Corresponding author: Mwaffaq El Heis, Radiology department, Jordan University of Science and Technology, Jordan
DOI: 10.26717/BJSTR.2018.03.000971
Mycobacterium malmoense is a rare infection with increasing prevalence since its first reported cases. It is not easy to be diagnosed. The objective of this study was to report our experience in managing this infection. A total of 24 cases were included from Jordan and United Arab Emirates. Our finding showed that in M. malmoense thick-walled cavitating lesions are common especially in the upper lobes. In our series, there was almost equal distribution of unilateral and bilateral disease. Underlying fibrosis was commonly present with pleural effusions rarely seen. Middle and lower lobe involvement was rare. The findings show the diverse range of radiological appearances seen in patients with non- tuberculous mycobacterial infections. Taken together, although the appearances are non-specific, an awareness of the varied presentations of these infections is important in order to expedite the correct diagnosis and the commencement of appropriate therapy.
Keywords: Mycobacterium malmoense; Pulmonary; Cavities; CTscan; X-Ray Radiography
Mycobacterium malmoense is known as a slow- growing non- tuberculous mycobacterium (NTM) and leads to human infection mainly among patients who are suffering from cellular immunity conditions [1] Although M. Malmoense mainly causes pulmonary infections, but extra pulmonary infections including cervical lymphadenitis and tenosynovitis are likely to exist [2]. M.malmoense is considered as an atypical mycobacterial strain that has been discovered in Sweden since 1954 [3] although the incidence of M. malmoenseis still rare, it has been shown to increase since the 1980s [4]. It has been noted that the majority of patients with M. malmoense infections have been affected by lung disease that impacts immune system including chronic obstructive pulmonary disease (COPD) [3]. According to the study of Hoefsloot, the occurrence of infection is significantly associated with contaminated water or soil.
It is of great importance to manage M. malmoense infections in terms of diagnosis at appropriate time and administration of appropriate treatment [3]. In their study, [5] showed the difficulties in diagnosis of pulmonary infection due to M. malmoense, a matter that impacts the appropriate treatment. They reported a case with delayed diagnosis because of thinking of pulmonary Mycobacterium tuberculosis infection. We have showed our experience of this infection in north Jordan and United Arab Emirates, and report the radiological findings in 24 patients seen over a 4 years period (Between January 2012 and December 2016).
A retrospective study design was conducted to review chest radiographs including CT scan and X-ray radiographs in Jordan and United Arab Emirates. There were 24 cases positive for this infection. The data for these cases were collected including age and gender. A radiographic description was give and summarized in tables and figures. Data was presented as frequencies and percentages for categorized variables, and as means for continuous variables.
As shown in Table 1, the study included 24 patients of whom two thirds (66.67%) were males. The mean age was 53 years in the range of 2-68 years. The chest X-ray showed that there was no pleural effusion, 24% had emphysema, 50% had fibrosis, about 17% had well circumscribed opacity, about 17% had air space shadowing, about 13% developed pleural disease, and about 4% developed primary focus (Table 2) and (Figures 1-4). A total of 8 patients out of 24 patients had CT scan of chest. Consolidation was exhibited in 25% of patients, nodes (mediastinum) were developed in 12.5% of patients, Pleural thickening in 12.5% of patients, and pleural effusion in 0% of patients.
Figure 4: Chest radiograph showing RT upper lobe cavitation and left upper lobe cavitation/consolidation.
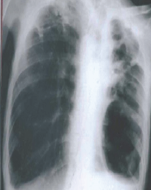
The results also showed that 37.5% of patients developed fibrosis, emphysema in 37.5%, cavities in 37.5%, focal abnormalities in 25%, interstitial thickening in 12.5%, and bronchiectasis in 25% of patients (Table 3) and (Figures 5-8). Cavities related variables included number of cavities, size of cavities, and wall thickness. In 90% of patients, the number of cavities was more two cavities. In 80% of patients, the size of cavity was more than 2cm. The majority of cases (80%) developed thick wall cavities (Table 4). As it can be seen in Table 5, pulmonary abnormalities were unilateral (41.77%), bilateral (58.33%), right upper lobe (37.5%), left (29.17%), right- apices (20.83%), and each of middle lobe and right lower lobe (4.17%].
The present study reported our experience in diagnosing the infection of M. malmoense through X-ray radiation and CT scan. A total of 24 cases were included. Although it is not common to find M. malmoensein clinical practice, there is still a possibility to be found. Our data showed that M. malmoense caused several pulmonary lesions including emphysema, pleural effusion, and pleural disease. These findings are consistent with previous studies [3]. Using CT scan showed multiple with sizes more than 2 cm in 80% of cases. These findings do agree with those of Evans et al. [3] who reported 6 cm cavity size in about 50 % of cases.
Our finding showed that in M. malmoense thick-walled cavitating lesions are common especially in the upper lobes. In our series, there was almost equal distribution of unilateral and bilateral disease. Underlying fibrosis was commonly present with pleural effusions rarely seen. Middle and lower lobe involvement was rare. The findings show the diverse range of radiological appearances seen in patients with non-tuberculous mycobacterial infections. Although the appearances are non-specific, an awareness of the varied presentations of these infections is important in order to expedite the correct diagnosis and the commencement of appropriate therapy [6,7].


