Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Mustufa Pervez*1, Idrees Shah2, Muhammed Umer Ahmed3 and Fiza Hassan Shah3
Received: March 09, 2018; Published: March 28, 2018
*Corresponding author: Mustufa Pervez, Department of Orthopedics, Ziauddin Hospital, Indus Residency, Block 4, Karach
DOI: 10.26717/BJSTR.2018.03.000895
Dynamic hip screws have been a mainstay of treatment for intertrochanteric fractures of the proximal femur and are also used to treat femoral neck fractures. Femoral neck fractures are usually common in older age but can also present in younger individual usually due to high energy trauma. Treatment of these fractures in young adults is debated due to higher energy demands of the age and need to salvage the bone instead of opting for a hemi arthroplasty or total hip arthroplasty as with older patients. Different other treatment options such as multiple cannulated screws have also been proposed but there still lies no consensus for the ideal treatment of such fractures. Displaced fractures are commonly associated with a vascular necrosis of the femoral head and multiple researches have been performed in this regard but if success of union occurs after a Dynamic hip screw is performed, the patient is able to regain his near physiological hip. Good bone quality and no comorbids usually present as an advantage in younger patients but still the surgery haunts orthopedic surgeons with its non-union and a vascular necrosis rates. Good anatomical reduction and stable fixation remains a mainstay of the treatment and can be perpetuated by a further use of a de-rotation screw.
Keywords: Femoral Neck Fractures; Osteonecrosis
Femoral neck fractures, though more prevalent in the elderly population, can occur in the young patients usually due to high energy trauma. Salvage of the femoral head is of prime concern to orthopedic surgeons given the age of the patients and there still lies a lack of consensus regarding the treatment of these kinds of fractures. Research and publications show a mixed result in this regard. These fractures are associated with a higher rate of osteonecrosis and nonunion and arthroplasty procedures are not ideal given the higher level of activity and age. Achieving an anatomic reduction and stable fixation is important and other factors such as timing of surgery and role of capsulotomy are still debatable. Dynamic hip screw (DHS) is based on the tension band principle which allows the screw to slide within the barrel to enable compression of the fracture at commencement of weight bearing. The union of the bone should ideally be primary type of bone healing which necessitates absolute stability at the fracture site. Other factors that make these kinds of fractures susceptible to nonunion are the intracapsular nature of the fracture and the synovial fluid also prevents blood clot formation. The intracapsular part also has no periosteal layer, hence the need for stable fixation with compression to achieve direct healing. Avascular necrosis presents as a common problem encountered after this method of fixation.
Figure 1: Gardens Classification of Hip Fractures I. Incomplete fracture II. Complete but undisplaced III. Complete fracture partially displaced IV. Complete fracture totally displaced.
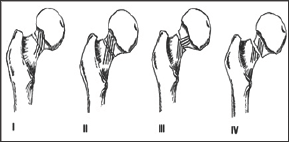
Different classification systems exist for the femoral neck fractures but the most commonly used are Gardens Classification and Pauwel's Classification. These systems attempt to differentiate the type of different fractures for the selection of an optimal treatment modality. The Garden's classification differentiates the femoral neck fractures into four types depending on the displacement and totality of the fracture. Type I and II fractures are UN displaced fractures but in type I fractures, the fracture line is incomplete. Type III and IV are complete fractures, Type III being partially displaced and Type IV being complete displaced (Figure 1).
Dynamic hip screw or sliding screw fixation consists of a lag screw, a side plate and cortical screws which fix the side plate to the proximal femoral shaft. The lag screw is inserted into the head of femur from the lateral aspect. For this surgery a C-arm image intensifier is required. The size of the hip is measured pre- operatively on the X-ray to get an idea about the probable size. The patient is supine on the fracture table with feet padded and placed firmly in the table boots. Contra lateral leg is either dropped down or abducted and flexed in a thigh holder. After preparation of the patient, the proximal femur is exposed using a lateral incision extending from the greater trochanter to 8-10cm distally. After bone exposure the guide wire is drilled into the proximal femur in ideally a centre-centre position and is measured. Triple reaming is done and the screw is inserted and a plate is applied to it which is secured with cortical screws (Figure 2). The idea behind the dynamic compression is that the femoral head component is allowed to move along one place and since bone responds to dynamic stress, the femur may undergo primary healing resulting in joint requiring no remodeling (Figure 3).
Figure 2: An illustration of Dynamic Hip Screw implant in the proximal femur.
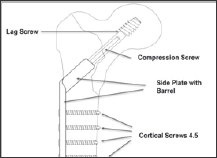
Figure 3: Xray Pelvis Anteroposterior and Lateral views showing a Dynamic Hip Screw Implant in the right proximal femur.

The treatment of femoral neck fractures has been debated for many years. The main issue during decision making is whether to fix it or to replace the neck. The optimal treatment for younger patients is still controversial and younger the patient, the more the orthopedic surgeon is obliged to pursue internal fixation [1]. Many factors can influence the decision namely the pre-injury functional status, mental ability and also the patient's demands. The criticism against internal fixation stems from its associated with higher association of non-union and osteonecrosis [2]. Nevertheless, when the femoral fractures heal, the patient has a chance of regaining their physiologically normal hip. Younger patients tend to have higher physiological reserves, good bone quality and usually no medical co-morbidities and the goal treatment is joint preservation. For internal fixation most orthopedic surgeons choose either a Dynamic Hip screw or multiple cannulated screws [3]. Tronzo in his research identified almost 100 different implants that are available for the fixation of this type of fracture [4].
Osteosynthesis with cannulated screws is a less invasive technique and reduces blood loss and soft tissue stripping but the Dynamic hip screw plate system provides a more stable fixation. Its disadvantages are large skin incisions, more soft tissue dissection, greater need for blood transfusion and a longer hospital stay. Makki showed no benefit in the union rates of osteonecrosis in fractures treated with either DHS alone or DHS with a de-rotational screw [5]. Furthermore Razik all studied 92 young patients and found that DHS supported with a de-rotational screw had siginificantly less osteonecrosis for Garden's type III and IV fractures [6]. Studies showed that age was an important factor while side or sex affected does not affect the final outcome and found no studies that show the role of these variables. According to Tolga Kaplan et all, physiological age rather than chronological age is more important in deciding the modality of treatment [7]. Most authors agree that the best position to fix the fracture is in anatomical reduction or slight valgus.
The results of osteosynthesis in young patients are debatable by presenting a considerable complication rates. However, little doubt is present that the most problematic complication is the occurrence of osteonecrosis [8]. Many variables have been associated with this complication after femoral neck fractures. Most literature does not support the differences in gender but higher rates of nonunion and AVN are more common in younger patients. Some explanations are given on the basis of high energy trauma and its correlation with dislocated fractures in young adults [9]. Lu-Yao et al published a meta-anyalysis of 106 published reports and concluded that the rate of loss of fixation or reduction after open reduction and internal fixation is about 16% (9-27%) which is significantly higher than the risk of dislocation after hemiarthroplasties and total hip replacements [10]. The rate of osteonecrosis ranges from 12-86%. Another controversial issue is the timing of the surgery. Barnes described a long term follow-up of 1503 sub capital fractures and concluded that the mortality rate increased if the operation was delayed more than 3 days following injury but no significant difference was found in osteonecrosis or late collapse when delaying the surgery upto 1 week [11].
Advocates of early surgery suggest that prompt reduction produces an unlinking of the proximal femoral vessels that leads to intracapsular decompression and restoration of the blood flow to the femoral head and minimizes the risk of osteonecrosis. Other studies also confirm that early surgery may decrease the rate of femoral head osteonecrosis while some studies show that there is no difference in osteonecrosis with more than 24 hour delay [12]. There also lays a controversy regarding the screw position in the femoral head. The main discussion concerns central versus posterior- inferior screw placement. There is a consensus that the anterior- superior position should be avoided because it is associated with a higher failure rate as called to attention by Barnes et al. There has been no paper in the literature regarding the position of the screw in relation to osteonecrosis of the femoral head. As the demands of young individuals are more as compared to an elderly patient and due to life spans of prosthesis, surgeons prefer to salvage the head in younger patients [13-20]. A recent research about treating young patients with DHS operated the fracture within 3 to 7 days. The union time was found to be 13.5 weeks and AVN was found only in 1 case for which implant removal and hemiarthroplasty was done and only 2 cases of non-union were found post operatively at an interval of 9 months. 1 patient developed superficial wound infection which responded to intravenous antibiotics and subsided [21-45].
The incidence of a vascular necrosis in patients younger than 55 with displaced femoral neck fractures that were treated with a Dynamic Hip Screw was found to be around 23.9%. No significant association between time to surgery, type of fracture and the application of a de-rotation screw with a vascular necrosis or nonunion was found.


