Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Leonidas Batas* and Lazaros Tsalikis
Received: March 07, 2018; Published: March 16, 2018
*Corresponding author: Leonidas Batas, Department of Periodontology, School of Dentistry, Aristotle University of Thessaloniki, Thessaloniki, Greece
DOI: 10.26717/BJSTR.2018.03.000862
In the last decade, body piercing has become increasingly fashionable especially among young adults. The growing trend of oral piercing must be a concern to dental professionals because of the risks and complications in the oral cavity. Oral piercings, such as tongue and lip piercing, can cause several complications such as hemorrhage, pain, swelling, lingual nerve damage, gingival recession, infection, periodontal distraction and fractured teeth. The purpose of this paper is to present case reports and methods of treating the complications of tongue and lip piercing that appeared to the periodontal tissues on the lingual and buccal sites of the lower incisors. In all cases EMD (Emdogain®) was used and the oral piercing was removed. All cases showed reduction of the pocket depth, gain in clinical attachment level and significant reduction of gingival recession. As a conclusion the use of EMD may be a treatment of choice in patients that had periodontal damage after oral piercing and these results seems to be reproducible.
Abbrevations: PD: Pocket Depth; CAL: Clinical Attachment Level; EMD: Enamel Matrix Derivative
Figure 1: A: The lower metal ball of the tongue piercing came in contact with area where the destruction of the lingual alveolar plate was present.
B: 8 mm pocket depth (PD) on the lingual surface of # 41.
C: Full thickness flaps raised, Lingual plate was missing.
D: EDTA was cautiously placed on the root surface for two minutes.
E: Emdogain® was placed on the surface of the root of # 41.
F: Flaps were sutured back.

A 26-year-old woman came in our office complaining of gum bleeding and swelling. Intraoral examination revealed a tongue piercing and also gum swelling in the lingual area of the lower central incisors and an 8 mm pocket depth (PD) on the lingual surface of # 41 (Figure 1). Radiographic examination showed distraction of the lingual plate in the area of # 31 and # 41. It was also noted that the lower metal ball of the tongue piercing came in contact with area where the destruction of the lingual alveolar plate was present (Figure 1). After explaining to the patient the problems that where created due to the tongue piercing, it was advised to her to remove the tongue jewel in order to begin periodontal treatment in the area. The goal of the treatment was to reduce inflammation and increase the clinical attachment level (CAL).
Conservative periodontal treatment (scaling and root planning) was performed. After one month there was reduction of inflammation but no reduction of PD was noted. At the surgical treatment a full thickness flap was performed at the area of # 31 - 41. Granulation tissue and residual calculus were removed from the area. Then, EDTA was cautiously placed on the root surface for two minutes, which was then removed by irrigating saline at the site (Figure 1). After the irrigation the root was dried and then carefully Emdogain was placed on the surface of the root of # 41 (Figure 1). Finally, the flap was sutured back using resorbable sutures (Figure1). The patient was given post-operative instructions and medication was administered (amoxicillin 500 mg every 8 hours, ibuprofen every 6 hours and chlorhexidine 0.12%). Sutures were removed after 2 weeks. After 6 months, a 6 mm reduction of the pocket depth, increased CAL and no inflammation was observed in the area (Figure 2). Comparison of radiographs before and after surgical treatment confirms the results (Figure 2).
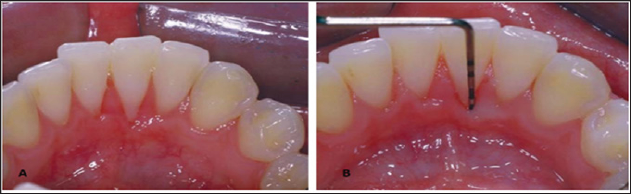
Figure 2: Clinical and radiographic findings before treatment (A,B) and 2 years after treatment (C,D).

A 21-year-old woman with a tongue piercing came in our clinic. The chief complain was bleeding gums and pain at her lower frond teeth. After intra oral examination, inflammation, bleeding on probing, deep pocket depth and extensive recession was observed at the area of # 41 (Figure 3). X-ray examination showed destruction of lingual plate in area 32-42 (Figure 3). And in this case also, the lower metal ball of the tongue piercing came in contact with area where the destruction of the lingual alveolar plate was present. Again it was advised to the patient to remove the tongue jewel in order to begin periodontal treatment in the area. Conservative periodontal treatment (scaling and root planning) was performed.At the surgical treatment, a partial thickness flap was applied at the lingual surface of the dental papilla, following the guide lines the double papilla technique, and then full thickness flaps were performed at the area of # 31 - 41.Granulation tissue and residual calculus were removed from the area. Then, EDTA was cautiously placed on the root surface for two minutes, which was then removed by irrigating saline at the site. After the irrigation the root was dried and then carefully Emdogain was placed on the surface of the root (Figure 3). The two papillae were sutured together and then the flap was sutured more coronally using resorbable sutures (Figure 3). Sutures were removed after 2 weeks. After 6 months, a 6 mm reduction of the pocket depth and recession was observed at the area and no inflammation was observed in the area (Figure 4).
Figure 3: A: Lingual recession #41
B: Deep pocket depth. Loss of clinical attachment level (CAL)
C: The lower metal ball of the tongue piercing came in contact with area where the recession was present.
D: Split thickness flaps were raised following the double papilla technique. The two papillae were sutured together.
E: Emdogain® was placed on the surface of the root of #
41.
F: Flaps were sutured coronally.
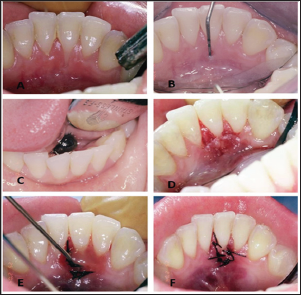
Figure 4: Reduction of recession and Probing depths were noticed 6 months after surgery.
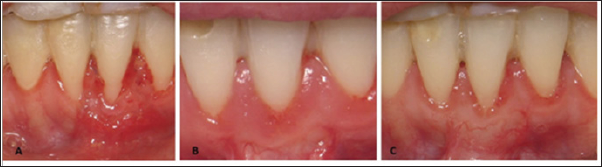
The third incident concerns a 29-year-old woman. The chief complaint was that she noticed a very big recession at the buccal area of the lower incisors. During the clinical examination a 8mm gum recession was noticed at # 31 (Figure 4) and also it was noted that patient had a lip piercing and the metal segment was in contact with the buccal plate were the recession was present. It was advised to the patient to remove the lip jewel in order to begin periodontal treatment in the area. The aim of the treatment was to reduce the recession and improve the prognosis of the tooth. It was decided to perform a connective tissue graft surgery at the site of #31. Connective tissue was harvested from the palate (Figure 4). A split thickness flap was raised at the site # 31. Then the root was conditioned with EDTA for 2 minutes. The connective tissue was then sutured in place covering the root of #31 (Figure 4). Emdogain was carefully then placed on the root surface and the flap were sutured back coronally covering the connective tissue graft with resorbable sutures (Figure 4). The patient received post-operative instructions. Sutures were removed after 2 weeks. After 6 months, reduction of recession was observed. 4 years post operatively the results remained the same (Figure 5).
Figure 5: A: The metal segment of the lip piercing came in contact with buccal plate at the area of 31.
B: Recession was noticed at the site of #31.
C: Partial thickness flaps were raised.
D: Root was conditioned with EDTA.
E: Connective tissue graft was haversed.
F: Emdogain® was placed on the root surface of #31
G: Connective tissue graft covered the root of #31.
H: Flaps were sutured coronally covering the connective tissue graft.
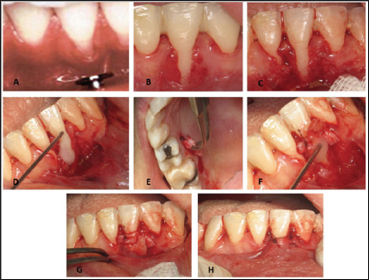
Figure 6: A: 1 month after surgery, B: 6 months after surgery, C: 4 years after surgery.
Oral piercing is an increasing social phenomenon. Therefore, dentists should be familiar with the consequences that this phenomenon may cause on dental and periodontal tissues. It is characteristic that in a survey conducted in Lancashire, in a sample of 106 clinical general dentists, 96.9% replied that patients with oral piercing, have come to their clinic13. In the literature it has been shown that there is a loss of attachment and bone support in the lower incisors, as well as severe ulceration and recession in the region [16-31]. In other cases, oral piercing patients caused fractures of teeth [32-35]. Also patients with trigeminal neuralgia are reported after tongue piercing [36]. There are also reports in which the perforation of the tongue has led to more serious complications, such as airway obstruction and dyspnea,[36], lingual problem [37,38], cerebral abscess due to streptococcus viridans infection [39,40], Ludwig [41-43], microbial endocarditis after Neisseria mucosa [43-45] infection, septicemia after prolonged bleeding [46], hepatitis [47], tetanus [48], chewing and chewing difficulties [49,50] , fractured teeth [51,52] and allergic reactions due to foreign body reaction.
Generally when a patient with oral piercing arrives our clinic, it must be explained to him/her all the risks and injuries that may occur, and try to convince that the best treatment is to remove it. When periodontal tissue lesions are present, the use of EMD (Emdogain) seems to be a reliable solution for reducing pocket depths, increasing clinical attachment levels and reducing inflammation. Enamel matrix derivative (EMD) (Emdogain- Straumann, Basel, Switzerland) is the most widely studied commercially available bioactive agent. It is derived from the tooth pouches of unerupted porcine teeth and is composed of amelogenins and enzyme components. The biological rationale for the use of EMD is to recapitulate developmental mechanisms whereby enamel matrix proteins are proposed to play a critical role in stimulating cementogenesis. The role of enamel proteins in periodontal ligament formation is supported by their presence in initial cementum formation during normal development of tooth attachment [53,54]. The major (>95%) constituent of EMD is amelogenins, a family of hydrophobic proteins derived from a single gene by alternative splicing and controlled post-secretory processing. The amelogenins are known to self-assemble into supramolecular aggregates that form an insoluble extracellular matrix [55] with high affinity for hydroxyl apatite and collagens [56]. When applied to denuded root surfaces, amelogenins therefore precipitates to form a stable extracellular matrix with a hydrophobic surface with potential for supporting interactions with cells in adjacent tissues. It should be noted that when EMD is used, for a period of six months from the surgical procedure it is important not to use periodontal probe in the area because it prevents proper healing of the area. Any evaluation of the result must be made after the end of the six months.
Oral piercings are a growing trend and dental care professionals are increasingly likely to treat a patient with at least one oral piercing. Having the knowledge to provide quality care to such patients, to educate the patient about the complications of oral piercings prior to the procedure and to recognize problems and appropriately treat or refer the patient is important in our ever- more-global society. From three case reports that was presented it was indicated that the use of EMD seems to have good and reproducible results in treating periodontal complications after oral piercing. Certainly, further research is needed on this.


