Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Boyan A Stoykov*1, Nikolay H Kolev1, Vladislav R Dunev1, Pencho P Genov2 and Manish Sachdeva1
Received: February 26, 2018; Published: March 08, 2018
*Corresponding author: Boyan Stoykov, Clinic of Urology, Medical University Pleven, Bulgaria
DOI: 10.26717/BJSTR.2018.03.000830
The objective of this study was to characterize time-dependent recovery of erectile function following robot-assisted radical prostatectomy (RARP) using the erection hardness score (EHS). This study included 42 patients with localized prostate cancer (PC) undergoing RARP without neoadjuvant hormonal therapy. The erectile function of each patient was assessed based on the international index of erectile function-5 (IIEF- 5) and EHS at the baseline and on every visit after RARP. In this series, potency was defined as the ability to have an erection sufficient for intercourse, corresponding to EHS ≥ 3, while patients with EHS ≥ 2 were regarded as those with erectile function. Of these 42 patients, 15 and 27 underwent bilateral and unilateral nerve-sparing procedures, respectively. A proportional increase in the IIEF-5 score according to EHS was noted at 12 months after RARP. At 3, 6 and 12 months after RARP, the recovery rates of erectile function were 22.6, 55.3 and 74.8 %, respectively, while those of potency were 11.7, 23.5 and 32.3 %, respectively. The results we obtained show that the EHS could be successfully used instead of IIEF-5 to assess post-operative EF recovery. Of the several factors examined, the age, preoperative outcome of IIEF-5 and the nerve-sparing procedure were identified as major independent predictors of EF recovery.
Keywords: Prostate cancer; Robot-assisted radical prostatectomy; Erectile function; Erection hardness score
Abbreviations: RARP: Robot-Assisted Radical Prostatectomy; EHS: Erection Hardness Score; PC: Prostate Cancer
In recent years, the proportion of patients treated with RARP as an initial therapy in prostate cancer has increased, as the number of patients diagnosed with prostate cancer at an early stage has increased significantly [1]. It is known that RARP can achieve excellent cancer control, with 10-year survival of > 90% [2]. Although significant advances have been made in recent years in exploring pelvic anatomy and the advancement of surgical techniques [3], RARP is still often accompanied by several types of postoperative adverse events such as incontinence and erectile dysfunction [3,4]. This has a negative impact on the postoperative quality of life of patients undergoing RARP [5].
Over the last decade, the introduction of RARP has led to a change in the paradigm in the field of surgical treatment of patients with localized prostate cancer. Robot-assisted radical prostatectomy has become the dominant procedure compared with other surgical approaches because robotic technology allows surgeons to perform more precise and accurate movements that help preserve the basic anatomical structures associated with achieving favorable functional outcomes [6]. Existing literature data also show relatively better functional outcomes after RARP than those following other approaches. In this study, we enrolled a total of 42 patients with localized prostate cancer who underwent RARP without neoadjuvant hormonal therapy. They were investigated for time-dependent changes in EF recovery following RARP based on the EHS.
This study includes a total of 42 patients with clinically localized prostate cancer who underwent RARP without neoadjuvant hormone therapy between May 2014 and December 2016 at the University Hospital "Dr. Georgi Stranski" Pleven. In our institution, RARP is performed with the help of robotic Da Vinci system (Intuitive Surgical Inc., Sunnyvale, CA, USA) using a transperitoneal approach. In our technique, we initially isolate and mobilize seminal vesicles, then proceed to dissection and ligation of the vascular plexus, followed by dissection of the bladder neck and continue the standard prostate removal. The preservation of the neurovascular bundle was usually performed by interfacial dissection in the avascular plane between the prostatic capsule and Denonvilliers fascia. We completed the posterior reconstruction of the rhabdosphincter and vesicourethral anastomosis using the techniquemdescribed by Van Velthoven [7].
The erectile function of the enrolled patients was assessed using a STP [8,9] where the patient responded to the question: "How would you rate the hardness of your erection?" and IIEF-5 [10] initially and on every patient visit at 3, 6 and 12 months after RARP. Potent are those patients who have an erection sufficient to achieve sexual intercourse consistent with the EHS ≥ 3, and patients with EHS ≥ 2 were only those with a sustained EF. The EF recovery rates and potency were calculated by the Kaplan-Meier method, and the differences were determined by the logarithmic test. The effects of some EF recovery factors were assessed using the Cox model for proportional hazard regression.
Table 1: Characteristics of patients.
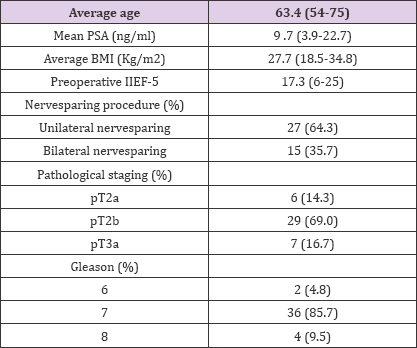
PSA-Prostate specific antigen, BMI-Basal metabolic index, IIEF- 5: International index of erectile function.
The clinical-pathological characteristics of these 42 clinically localized prostate cancer patients included in this study are summarized in Table 1. Initially, the mean IIEF-5 and EHS in these 42 patients were 17.3 and 3.1 points, respectively. In this series RARP was completed in all 42 cases without the need for conversion to open surgery. Of these 42 patients, 15 (35.7%) and 27 (64.3%) underwent bilateral and unilateral nerve preservation respectively. After comparing the results of IIEF-5 with EHS at the 3rd, 6th and 12th month after RARP, we found a significant proportional increase in points in the IIEF-5 and EHS. Mean IIEF-5 values were 6.7, 11.3 and 21.1, mean EHS values were 0-1, 2 and 3-4. EF recovery rates at 3, 6 and 12 months after RARP were 22.6, 55.3 and 74.8%, respectively, whereas those related to potency at 3, 6, and 12 months after RARP were respectively 11.7, 23.5 and 32.3%. We subsequently assessed the impact of several parameters to predict EF recovery using these statistical methods. Of these factors, age, preoperative outcome of IIEF-5 and the nervesparing preservation procedure were identified as major independent predictors of EF recovery (Table 1).
Robot-assisted radical prostatectomy has become a widely accepted surgical approach in clinically localized prostate cancer. There are several studies that perform systematic reviews and meta-analyzes of the EF after RARP [4,11]. For example, Ficarra et al. reported that at 12 months post-RARP, potency recovered between 54 and 90% and at 24 months between 63 and 94% [4]. According to Kilminster et al. potency at 48 months varied between 60-100% [11]. Our results show a 74.8% EF recovery in the first year after RARP, which is close to the above results. Because of the very small number of patients in this series, we assessed the impact of just a few parameters on EF recovery using the Cox model for proportional hazard regression, and we found that the age, preoperative outcome of IIEF-5 and the nerve preservation procedure are independent predictors of EF recovery . These results are consistent with those of previous studies identifying parameters to predict potency recovery [4,5,12-14]. For example, Ficarra et al. reported that age, preoperative outcome of IIEF-5, concomitant illness and choice of nerve preservation techniques were the most appropriate predictors of RARP recovery [4]. These findings also suggest that EF assessed by the EHS could be an alternative to study postoperative potency in patients undergoing RARP, especially in those with a relatively low sex profile. Another interesting point is to develop a system for more accurate prognosis of EF after RARP by combining potential predictors to achieve better individualisation of patient treatment.
In the study conducted by us on 42 patients with clinically localized prostate cancer, we evaluated changes in erectile function after RARP. Although these patients are characterized by a comparatively low sexual profile with a baseline score of IIEF-5 and the EHS of 17.3 and 3.1 points, we have found a corresponding proportional increase in the IIEF-5 and EHS 12 months after RARP. This indicates that the EHS can be used as an alternative to IIEF- 5 for assessing post-operative changes in erectile function. In our study, we also found that recovery of erectile function and potency at 12 months after RARP were 74.8 and 32.3%, respectively. We confirmed that the age, preoperative outcome of MEEF-5 and the nervesparing preservation procedure were independent predictors for restoring erectile function. To confirm these results, we need a long-term study involving a large number of patients.


