Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
María Ricarda García Viveros, Maria de Lourdes Castellanos Villalobos, Carmen Sofia de Socorro Silva Cañetas and Rosa María Torres Hernández*
Received: December 22, 2025; Published: January 09, 2026
*Corresponding author: Torres Hernández Rosa María, Clinical research Faculty of Medicine, Universidad Veracruzana, Mexico
DOI: 10.26717/BJSTR.2026.64.010040
Introduction: Cardiac rehabilitation is a multidisciplinary program designed to support children and adolescents
who experience limitations imposed by their disease and to facilitate their reintegration into activities of
daily living.
Objective: To evaluate the impact of a cardiac rehabilitation program in pediatric patients after surgery for
congenital heart disease.
Methodology: A quasi-experimental study was conducted in six children who had undergone surgery for congenital
heart disease and were classified as low cardiovascular risk. All participants attended a phase II cardiac
rehabilitation program. Exercise testing and the WeeFIM scale were applied before and after the intervention,
which consisted of low-impact exercises. Exercise intensity was regulated using the EPInfant scale, with training
performed at 60% of heart rate reserve.
Results: Six patients were included, with a mean age of 9 ± 3.3 years; four were male and two female. Four patients
were diagnosed with atrial septal defect and two with Tetralogy of Fallot. At the beginning and end of the
rehabilitation program, a significant increase in VO₂, METs, and heart rate was observed. Pearson’s correlation
between the WeeFIM score and VO₂ was 0.736, indicating a strong positive relationship between these variables.
Conclusion: At the end of the program, patients showed improvement in physical capacity and level of independence,
as demonstrated by the strong positive correlation between the WeeFIM scale and VO₂.
Keywords: Cardiac Rehabilitation; Exercise Test; Congenital Heart Disease; WeeFIM Scale; Epinfant
Abbreviations: ASD: Atrial Septal Defect; VSD: Ventricular Septal Defect; CVR: Cardiovascular Risk Stratification; AACVPR: American Association of Cardiovascular and Pulmonary Rehabilitation; METs: The Number of Metabolic Equivalents
Congenital heart disease is defined as an evident structural abnormality of the heart or the intrathoracic great vessels with real or potential hemodynamic consequences. It is estimated that approximately 18,000 to 21,000 children are born each year with some type of congenital malformation. A higher prevalence of acyanotic congenital heart diseases has been reported (85.8%), with atrial septal defect (ASD) being the most frequent, followed by ventricular septal defect (VSD). Among cyanotic congenital heart diseases, single atrium and Tetralogy of Fallot are the most common, with a higher prevalence in males [1] Scientific and technological advances in recent decades, particularly the development of cardiac catheterization and echocardiography, have radically changed the prognosis of patients with congenital heart disease by establishing a strong foundation for cardiovascular surgery. As a result, an increasing number of patients with congenital heart disease survive into adulthood [1] Children with congenital heart disease are often discharged from the hospital without a consensus-based cardiac rehabilitation protocol, despite having congenital diseases or having undergone surgical procedures. Therefore, there is a need for a rehabilitation program specifically designed for the pediatric population, based on the different stages of development and structured according to cardiovascular risk stratification and type of congenital heart disease [2] Cardiac rehabilitation is a multidisciplinary program designed to support children and adolescents who experience limitations imposed by their disease.
The program includes preventive, physical, nutritional, educational, and psychological components, with the aim of improving physical condition in a controlled and monitored environment. Initially, cardiovascular risk stratification (CVR) is performed, which is understood as a comprehensive clinical and paraclinical assessment that allows estimation of the probability that a patient will experience an adverse outcome in the future. This scientifically based predictive method classifies patients as low or high risk. Low-risk patients are asymptomatic, whereas high-risk patients include those with severe pulmonary hypertension, documented long QT syndrome, heart failure, hemodynamically significant arrhythmias, hypertrophic cardiomyopathy with symptoms, outflow tract obstruction or documented arrhythmias, Marfan syndrome with suspected aortic dissection, acute myocardial infarction, exercise-induced syncope, severe mitral or aortic stenosis, as well as active hepatitis or pneumonia. In this latter group, cardiac rehabilitation is contraindicated [3-5]. In physical rehabilitation, the Functional Independence Measure for Children (WeeFIM) is an assessment instrument used to determine the degree of independence and maximum functional capacity that children with disabilities can achieve in activities of daily living. It estimates functional independence by measuring how consistently a child performs a given task. The WeeFIM is designed to evaluate children with disabling conditions such as cerebral palsy, trisomy 21, spina bifida, epilepsy, cardiac disorders, Rett syndrome, shaken baby syndrome, limb deficiencies, and genetic or motor disorders, ranging from 6 months to 7 years of age or older, even up to 18 years [5-8]. The WeeFIM consists of 18 measurement items scored from 1 to 7, grouped into three subcategories: self-care (8 items: feeding, bathing, grooming, upperand lower-body dressing, toileting, bladder and bowel management), mobility (5 items: walking, stair use, transfers, chair-to-toilet, chairto- shower), and communication and social cognition The score for each subdomain ranges from 1 to 7 according to the subject’s level of dependence. These scores are summed by domain and compared with reference tables included in the WeeFIM scale to determine, using standard deviations, whether the evaluated child falls within normal ranges of independence for their age [9]. The EPInfant scale is included in the exercise monitoring guidelines of the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR).
The WeeFIM scale determines the level of independence, while the EPInfant scale is used to regulate exercise intensity. Exercise testing is performed on a treadmill using the Bruce and Naughton protocols to evaluate cardiovascular responses, including blood pressure, resting heart rate, maximum heart rate, increases in blood pressure and heart rate during the stages of the Bruce protocol, and their decrease during the recovery phase. The number of metabolic equivalents (METs) achieved is estimated, as well as treadmill time, which has been reported as 11.8 ± 1.2 minutes in boys and 10.7 ± 1.2 minutes in girls [10]. There are few centers that offer cardiac rehabilitation programs for the pediatric population. However, many of the problems experienced by children with congenital heart disease can be improved through these programs. Therefore, the aim of this study was to evaluate the benefit of a cardiac rehabilitation program in pediatric patients after surgery for congenital heart disease [11].
Six patients were enrolled in the cardiac rehabilitation program, with a mean age of 9 ± 3.3 years. Four were male (66.7%) and two female (33.3%). Diagnoses included atrial septal defect in four patients (66.7%) and Tetralogy of Fallot in two patients, all classified as low cardiovascular risk. In the initial exercise test, maximum heart rate was 63 ± 10.5 beats per minute, compared to 71 ± 7.5 beats per minute in the final test (p < 0.014). Mean VO₂ increased from 17 ± 7.89 to 30 ± 4.62 ml/kg/min (p < 0.002). METs increased from 5 ± 2.26 to 8 ± 1.31 (p < 0.002) (Table 1) Pearson correlation analysis showed a correlation coefficient of r = 0.431 between initial WeeFIM and VO₂, and r = 0.736 between final WeeFIM and VO₂, indicating a strong positive linear relationship between final variables (Table 2).
Table 1: Differences between baseline and final measurements after the cardiac rehabilitation program in postoperative patients with congenital heart disease (HRmax = maximum heart rate; VO₂ = maximal oxygen consumption; MET = metabolic equivalent).
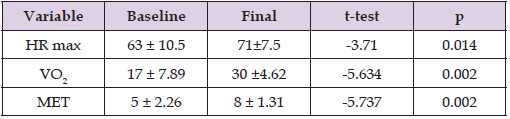
Note: t-test with a level of significance of p < 0.05.
Congenital heart disease is defined as an evident structural abnormality of the heart or the intrathoracic great vessels with real or potential hemodynamic consequences. It is subdivided into two major groups: a cyanotic and cyanotic congenital heart diseases. The most frequent conditions are left-to-right shunt lesions, followed by those that produce pressure overload. The global prevalence continues to increase, and up to 90% of these patients now reach adulthood due to improvements in diagnosis and treatment over recent decades. Because most surgical techniques are palliative rather than curative, these patients face increased mortality, high reintervention rates, and complications in adulthood [4]. In primary cardiovascular prevention, individual cardiovascular risk estimation is essential to identify pediatric patients who are candidates for a cardiac rehabilitation program. Cardiac rehabilitation is a multidisciplinary program designed to support children and adolescents with limitations imposed by their disease. The minimum age for inclusion in a cardiac rehabilitation program is 7–8 years, as reliable exercise testing can be performed at this age. The study population fell within this range, with a mean age of 9 ± 3.3 years; four patients were male (66.7%) and two female (33.3%) [8]. Initial assessment of pediatric cardiac patients includes cardiovascular risk stratification. To complement this evaluation, it is necessary to use a scale that assesses the level of independence in activities of daily living. One of the most widely used tools in physical rehabilitation is the Functional Independence Measure for Children (WeeFIM). This assessment instrument determines the degree of independence and maximum functional capacity that children with disabilities can achieve in daily activities by measuring how consistently a child performs a given task. It is designed for children with disabling conditions such as cerebral palsy, trisomy 21, spina bifida, epilepsy, cardiac disorders, Rett syndrome, shaken baby syndrome, limb deficiencies, and genetic or motor disorders, ranging from 6 months to 7 years of age or older, up to 18 years [7,8]. The WeeFIM consists of 18 items scored from 1 to 7, grouped into three subcategories: self-care (8 items: feeding, grooming, bathing, upper and lower body dressing, toileting, bladder and bowel management), mobility (5 items: walking, stair use, transfers, chair-to-toilet, chair-to-shower), and communication and social cognition (including comprehension, expression, social interaction, problem-solving, and memory).
Each subdomain is scored from 1 to 7 according to the subject’s level of dependence. In all six patients, improvement in physical independence was observed through the application of the WeeFIM scale, which is noteworthy since this scale has not been commonly used in studies similar to ours, where quality-of-life scales are more frequently applied. During the initial phase, patients demonstrated a level of disability that limited dressing, feeding, and hygiene activities, requiring partial assistance from a caregiver or supervision and guidance during task performance. In terms of mobility, activities such as walking and ascending or descending stairs required total assistance from a caregiver for climbing stairs and supervision for descending. At the end of the program, patients were able to perform all activities independently, with only two patients requiring supervision when climbing or descending stairs. Regarding academic activities, only one patient required caregiver assistance to complete schoolwork, in addition to support from other specialties to improve academic performance [7,8]. In the final exercise test, all patients showed significant improvements in VO₂, maximum heart rate, and metabolic equivalents (p = 0.002), findings comparable to those reported in a systematic review by N Duppen, et al. [12] who evaluated the effects of an exercise program in children with congenital heart disease. These improvements reflect increased physical capacity and tolerance to physical activity, as demonstrated in our study, where patients were able to reintegrate into activities of daily living, including recreational exercise [8]. To evaluate physical capacity and degree of independence after the intervention, the WeeFIM scale was used, along with correlation analysis between VO₂ indirectly obtained through exercise testing. MET values were calculated by multiplying the total METs achieved during the test by 3.5 ml/kg/min (VO₂), using two different protocols: Bruce and Naughton, the latter applied to severely deconditioned patients. The Bruce protocol consists of seven stages, each lasting three minutes, with progressive increases in speed and incline, resulting in increasing energy consumption. Stage 1 corresponds to 4.6 METs and stage 7 to 19.5 METs. The Naughton protocol also consists of seven stages, each lasting two minutes, with a constant speed of 3.2 km/h and gradual increases in incline; the initial stage corresponds to 2.5 METs and the final stage to 8.3 METs. Patients who underwent the Bruce protocol completed up to stage 3 (10.3 METs), while those who performed the Naughton protocol reached stage 6 (7.4 METs). A strong relationship between these variables was established, confirming that at the conclusion of the cardiac rehabilitation process, patients improved their degree of independence in parallel with theoretical VO₂, corroborated by the final energy expenditure of each exercise test [3,8,9,13,14].
The pediatric cardiac rehabilitation program considered cardiovascular risk, neurodevelopment, and level of disability and was structured according to patient preferences, with individualized dosing and supervision by trained personnel. The program resulted in improvements in heart rate response, maximal oxygen consumption (VO₂), self-esteem, functional independence, and quality of life. Exercise intensity and progression were monitored using the EPInfant scale, which allowed assessment of disability level and its gradual reduction, achieving independence simultaneously with improvements in maximal oxygen consumption.
The authors declare no conflict of interest.


