Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Jawaher Mays AlAnazi1#, Sara Abou Al-Saud2#, Nora AlZoman1 and Aliyah AlMomen1*
Received: September 29, 2025; Published: October 10, 2025
*Corresponding author: Aliyah AlMomen, Pharmaceutical Chemistry Department, College of Pharmacy, King Saud University, P.O. Box 22452, Riyadh 11495, Saudi Arabia
DOI: 10.26717/BJSTR.2025.63.009906
Hypertension has become a global epidemic, affecting approximately 1.13 billion people. Uncontrolled hypertension is the leading cause of stroke, heart failure, and kidney failure if left untreated and can eventually lead to death in individuals of all ages. Angiotensin-converting enzyme inhibitors are among the first-line therapeutic agents used in the management of hypertension. Two drugs are considered bioequivalent when they are equal in the rate and extent to which the active pharmaceutical ingredient becomes available at the site of drug action. Therefore, this study evaluated the bioequivalence of lisinopril, designated as the branded drug, and two generic formulations, referred to as Generic 1 and Generic 2, available in the Saudi market, as well as the pharmacokinetic parameters and safety effects on the liver and heart. Results demonstrate that the brand effectively controls blood pressure in rats over a two-week period, showing superior efficacy in reducing systolic blood pressure compared to generic 1 and generic 2, with no significant impact on liver and cardiac enzymes, and greater safety for kidney and heart function.
Keywords: Hypertension; Blood Pressure; ACE Inhibitors; Lisinopril; Generic and Brand
Abbreviations: ACE inhibitors: Angiotensin-Converting Enzyme Inhibitors; AST: Aspartate Transaminase; CKMB: Creatine Kinase MB; DBP: Diastolic Blood Pressure; HPLC: High-Performance Liquid Chromatography; LDH: Lactate Dehydrogenase; Cmax: Maximum Concentration; NCA: Noncompartmental Analysis; PK: Pharmacokinetics; SBP: Systolic Blood Pressure; Tmax: Time Taken to Reach Cmax
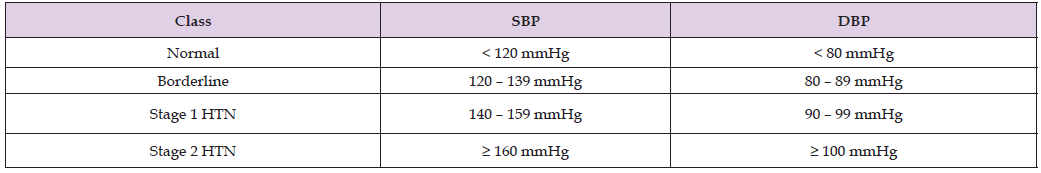
(Graphical Abstract) Clinically, hypertension is characterized by systolic blood pressure (SBP) exceeding 140 mmHg and diastolic blood pressure (DBP) over 90 mmHg [1]. Today, high blood pressure is considered one of the most common diseases worldwide, representing a global epidemic with more than a billion sufferers. Typically, high blood pressure has no symptoms, but there are underlying risk factors that can worsen its onset, such as an unhealthy lifestyle, alcohol use, tobacco smoking, lack of exercise, and obesity. The aforementioned risk factors are considered modifiable, meaning that they can be minimized or eliminated to avoid the likelihood of hypertension. On the other hand, non-modifiable risk factors include family history, age over 65, and diseases such as diabetes, kidney disease, and vascular disease. The Centers for Disease Control and Prevention conducted high blood pressure research in 2017 on a large population aged 18 and over, and the results showed that 29% of the population had high blood pressure [1]. In Saudi Arabia, Al Qassim University conducted cross-sectional research with nearly 10,000 participants, and the confirmed cases of hypertension were 15%, while cases of borderline hypertension were 40%. Left untreated, high blood pressure eventually leads to stroke, heart failure, and kidney failure, and in some cases can be fatal in all age groups. According to the American Heart Association, blood pressure is classified as shown in Table 1.
Table 1: Classification of hypertension. This table provides the classification of blood pressure levels based on the guidelines from the AHA. Blood pressure is categorized into four classes, based on systolic and diastolic measurements.
As recommended by the Joint National Committee, to lower blood pressure and reduce the likelihood of developing hypertension, individuals should adopt lifestyle changes such as weight loss, smoking cessation, and increased physical activity. In some cases, lifestyle changes are not enough to lower blood pressure, so pharmacological therapy is required to achieve the desired blood pressure [2]. Lisinopril belongs to the ACE inhibitor class and is structurally derived from enalapril. Lisinopril is pharmacologically active in its administered form and does not require metabolic activation. The mechanism of action of lisinopril is mainly by dilating the arteries and veins by competitively inhibiting the conversion of angiotensin I to angiotensin II, which is a potent endogenous vasoconstrictor. In addition, lisinopril inhibits bradykinin metabolism, resulting in a reduction in cardiac preload and afterload [3]. Lisinopril also promotes sodium and water excretion by inhibiting angiotensin-2-induced aldosterone secretion. With the use of lisinopril as a therapeutic agent, an increase in serum potassium can be observed [4], Lisinopril is an orally administered drug, and the pharmacokinetics (PK) reported in previous studies show the onset of action within one-hour, maximum effects within 6 hours, a duration of action of 24 hours, bioavailability in adult patients of about 25% (with a range of 6-60%), an elimination half-life of about 12 hours, and the drug is excreted through the urinary system in an unchanged form [5].
There are numerous methods for quantifying lisinopril in monocomponent or multicomponent tablets, including spectrophotometry, high-performance liquid chromatography (HPLC), capillary electrophoresis, and gas-liquid chromatography. The spectroscopic and spectrofluorometric methods can provide low levels of detection; however, they are not selective for lisinopril degradation products. One of the advantages of HPLC/Mass Spectrometry (MS) is that the method can be selective, sensitive, and available at King Saud University’s central laboratory [5]. The chemical structure of lisinopril is shown in Figure 1. The bioequivalence of two products is considered equal when the speed and extent of the active pharmaceutical ingredient reaching the drug’s sites of action are the same. Bioequivalence studies are used in various aspects, mainly when a sponsor proposes to produce a generic version of an authorized new medicinal product (US FDA, 2022). Bioequivalence studies are conducted in two ways: either in-vitro bioequivalence studies or in-vivo studies. In-vitro studies are performed in a dissolution apparatus by providing all the necessary biological conditions similar to the human biological system. In general, in-vitro studies are not expensive and do not require large sample sizes. In-vivo studies are performed on humans or animals to measure both the rate and extent of the drug’s absorption into the bloodstream.
In-vivo studies usually provide very reliable results, but there are some limitations, such as variability, and they can be quite expensive. In 2005, a bioequivalence study of the lisinopril brand and the generic was conducted in 28 healthy volunteers who received one 20 mg tablet on two treatment days separated by a two-week washout period [6]. The conclusion of the study was that there was no statistical significance between the two formulations, and they had a comparable pharmacokinetic profile [6]. After three years, in 2008, another bioequivalence study was conducted among 18 healthy Chinese subjects who received 20 mg tablets of either the brand or generic, and the result was that generic lisinopril was found to be bioequivalent to the brand in terms of rate and extent of absorption [7]. The rationale for our research is that hypertension is a serious disease, and the treatment plan must achieve the desired result. Since the Saudi market carries both the brand and generic forms of lisinopril, this study evaluated the bioequivalence between these forms. To achieve this, the biological effects of branded lisinopril (brand) and two generic drugs (generic 1 and generic 2) were evaluated, as well as the pharmacokinetic parameters and safety effects on the liver and heart.
Experimental Animals
Twenty male albino rats (weighing 235–322 g) were obtained from the Animal House, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia. The rats were randomly assigned into four groups (n = 5), with the fourth group serving as the control. They were housed in Type IV Ventilated Cages (20” L × 11” W × 9” H), with 4–5 rats per cage. Cage hygiene and bedding were monitored and maintained daily. The animals were kept at a controlled room temperature of 25°C and 40% relative humidity. All procedures followed the ethical guidelines of the King Saud University - Ethical Committee for Animal Research (Protocol KSU-SE-22-31). Euthanasia was performed by asphyxiation in a controlled CO₂ chamber. Methods adhered to ARRIVE guidelines. Novelty Note: This study uniquely utilizes a salt-induced hypertensive rat model to evaluate the pharmacokinetics and potential bioequivalence of multiple lisinopril formulations (branded and generic) under standardized conditions—an approach not previously reported regionally.
Study Design
Rats were fed a high-salt diet (3 grams of salt in 1 liter of water) daily for 14 days to induce hypertension, with free access to standard commercial food [8]. The rats’ weight was measured before and after the development of hypertension on various days throughout the experiment to evaluate the effect of hypertension on their weight. After confirmation of hypertension, rats were divided into three groups (n=5), each receiving 5 mg of either (brand 20 mg) or generic (generic 1 or generic 2 20 mg) lisinopril daily for 14 days. The number of animals per group was based on previous studies showing that n=5 is sufficient for statistical significance [3]. SBP was measured on days 2, 6, 9, and 12. The lisinopril tablets (brand, generic 1, generic 2) were obtained from (UK), (Saudi Arabia), and (Saudi Arabia), respectively. To administer the drug, each tablet was crushed into a fine powder and dissolved in 20 mL of tap water to create a 1 mg/mL suspension. The rats were given the drug orally via gavage. After 14 days of treatment, blood samples (0.3 mL) were collected at predetermined time points (0.5, 1, 2, 3, 5, 24, 48, and 72 hours) following drug administration. Blood was drawn from the tail vein into heparinized tubes, then centrifuged at 4500 rpm for 10 minutes at 4°C.
Plasma was separated and stored at -20°C until analysis. Plasma levels of lisinopril were analyzed using a validated HPLC/MS approach (Agilent, USA) with a C18 column (15 cm × 4.6 mm, 5 μm particle size). The chromatography mobile phase included a mixture of acetonitrile and phosphate buffer (20:80 v/v) at a flow rate of 1 mL/ min. Quantification was performed using a linear calibration curve ranging from 1.56 to 100 ng/mL, with a correlation coefficient of 0.99 [3].
Design Innovation: The simultaneous comparison of a brand and two regionally manufactured generics within a controlled hypertensive model offers a unique and practical pharmacological insight that may influence therapeutic policy and regulatory standards. SBP was measured on Days 2, 6, 9, and 12. After 14 days of treatment, 0.3 mL blood samples were collected from the tail vein at predetermined intervals (0.5, 1, 2, 3, 5, 24, 48, and 72 hours). Samples were centrifuged at 4500 rpm for 10 min at 4°C, and plasma was stored at -20°C until analysis.
Pharmacokinetic Analysis
In all treated rats, lisinopril brand and generics analyses were performed using noncompartmental analysis (NCA) via Excel 2010, with the PKSolver add-in. Cmax and Tmax were obtained from the corresponding plasma concentration-time curves as shown in Figure 2. Linear regression of the terminal phase of the log-linear plasma concentration-time curve was performed using four points to estimate the terminal elimination rate constant (λ) and calculate t1/2 from the formula t1/2 = 0.693/λz. The area under the curve (AUC) of the plasma concentration-time curve from time 0 to the last sampling time t (72 h) (AUC0-t) was calculated using the trapezoidal rule. Apparent oral clearance (CL/F) was calculated as follows: CL/F = dose/ AUC0-∞, where CL represents drug clearance, F represents drug bioavailability, the dose was 5 mg for each rat, and AUC0-∞ is the area under the curve for plasma concentration-time from 0 to ∞. AUC0-∞ was derived by summing AUC0-t and the area obtained by extrapolation from time t to ∞. The latter area was calculated by dividing the last measured concentration (Clast) by λz [3]. After one day of treatment, to study the PK of the drug, the Cmax for drug absorption was approximately 200 ng/mL in brand.
In contrast, generic 1 and generic 2 showed a reduction of 50% in Cmax compared to brand, which is a statistically significant difference between the lisinopril brand and generics. For Tmax, the time taken to reach Cmax, brand and generic 2 showed similar values, and based on the data, no statistically significant difference was found between them. For other pharmacokinetic parameters such as AUC0-72, AUC0- ∞, and CL/F, brand exhibited a high statistically significant difference when compared to the generic forms [3]. Pharmacokinetic parameters are represented in Figure 2.
Methodological Novelty: The use of a high-resolution time-point strategy and open-access PKSolver software enables transparent, reproducible pharmacokinetic modeling—an innovative approach in local comparative drug studies. Statistically significant differences in PK parameters (Cmax, AUC, CL/F) were observed between branded and generic formulations. brand demonstrated a higher Cmax (~200 ng/mL) compared to generic 1 and generic 2 (50% reduction), with significant differences in AUC₀₋₇₂ and CL/F.
Statistical Analysis
Results are expressed as mean ± SD. One-way ANOVA followed by Bonferroni post hoc test was applied to compare pharmacokinetic parameters across groups. Statistical significance was set at p ≤ 0.05 [9].
Statistical Approach Note: This study’s design and multivariate comparison across time points provide robust differentiation in pharmacokinetic behavior among formulations, underscoring its practical and regulatory relevance.
Methodological Innovation
To the best of our knowledge, this is the first preclinical study in the region to:
• Compare branded vs. multiple local generic lisinopril formulations in hypertensive rats
• Utilize an 8-point sampling strategy to model detailed PK profiles
• Apply open-source software for accessible pharmacokinetic analysis, supporting local regulatory evaluation of generics
Results and DiscussionThe Effect of Lisinopril Brand and Generics on Blood Pressure
On day 14 of the treatment, systolic blood pressure (mmHg) for brand, generic 1, generic 2, and the control group were 141.4 ± 5.32, 135.4 ± 3.36, 136.4 ± 4.61, and 144 ± 5.33, respectively, as shown in Figure 3. Brand showed a statistically significant reduction in blood pressure within the first few days of treatment. In contrast, the generic forms, generic 1 and generic 2, did not achieve the same level of blood pressure reduction during the experimental period, when compared to the brand.
The Effect of Lisinopril Brand and Generics on Liver Enzymes and Cardiac Enzymes
Liver Enzymes: Aspartate transaminase (AST) levels for generic 1, generic 2, brand, and control were (20.26 ± 8.09), (70.49 ± 28.15), (6.97 ± 1), and (7.51 ± 1.25), respectively, as shown in Figure 4A. Brand had a similar effect on AST levels as the control group, with minimal changes. However, generic 1 caused a minor increase in AST, while generic 2 caused a substantial increase in AST levels compared to the other groups.
Lactate Dehydrogenase (LDH): The mean values for LDH were (76.17 ± 17.30), (90.76 ± 8.46), (41.95 ± 6.99), and (41.31 ± 11.68) for generic 1, generic 2, brand, and control, respectively, as shown in Figure 4B. Brand had a minimal effect on LDH levels, similar to the control, while both generic forms, generic 1 and generic 2, exhibited higher LDH levels.
Cardiac Enzymes: For creatine kinase MB (CK-MB), the mean values were (38.81 ± 10.15), (61.30 ± 20.45), (17.54 ± 7.22), and (17.50 ± 17.77) for generic 1, generic 2, brand, and control, respectively, as shown in Figure 4C. The generic forms, especially generic 2, caused a significant increase in CK-MB levels, which was notably higher than the brand and control groups.
The Effect of Lisinopril Brand and Generics on Rats’ Weight
Figure 5 shows that there was no statistically significant difference in the weight changes between the branded and generic lisinopril groups. Despite developing hypertension, all treated groups showed a significant increase in body weight after the treatment. This suggests that while hypertension was induced, lisinopril (regardless of the form) did not significantly affect weight gain.
The Effect of Lisinopril on PK
After one day of treatment, pharmacokinetic parameters were assessed. For maximum concentration (Cmax), brand reached approximately 200 ng/mL, while generic 1 and generic 2 showed 50% lower levels than brand, indicating a statistically significant difference between the branded and generic forms (Figure 2A). For the time taken to reach Cmax (Tmax), brand and generic 2 were quite similar, with no significant difference between them (Figure 2B). For other pharmacokinetic parameters, including AUC0-72, AUC0-∞, and CL/F, brand showed highly significant differences compared to the generic forms (Figure 2C-2F), indicating superior bioavailability and pharmacokinetic performance of the branded drug [3].
The significance of our research lies in the finding that brand was statistically significant in controlling rats’ blood pressure within the two-week treatment duration, with no significant effect on increasing liver and cardiac enzymes. Brand was more effective in reducing systolic blood pressure compared to the generics 1 and 2 after two weeks of treatment. Moreover, brand demonstrated greater safety concerning kidney and heart function, as evidenced by the pharmacokinetic studies.
We want to acknowledge Jawaher Alanazi for her poster presentation titled ‘Bioequivalence Evaluation of Lisinopril Trade vs Generic in Saudi Market using LC-MS’, which contributed to this work. The poster is available at: https://coprd-ksu.com/wp-content/uploads/ 2022/05/Postgraduate-KSU-Jawaher-Alanazi10-04-22-1.pdf.
The authors declare that there are no conflicts of interest to disclose.
This project was funded by the Researchers Supporting Project, King Saud University, Riyadh, Saudi Arabia (Project No. [RSP2025R215]).
All procedures followed the ethical guidelines of the King Saud University - Ethical Committee for Animal Research (Protocol KSUSE- 22-31). Euthanasia was performed by asphyxiation in a controlled CO₂ chamber. Methods adhered to ARRIVE guidelines.
Not applicable, as the study did not involve human participants.
The datasets generated and analyzed during this study are available from the corresponding author upon reasonable request.
• Jawaher Mays AlAnazi: Laboratory experiments, sample
preparation, and LC-MS analysis.
• Dr Sara Abou AlSaud: Study conception, experimental design,
and supervision.
• Dr Nora AlZoman: Data analysis, statistical interpretation,
and validation.
• Dr Aliyah AlMomen: Drafting and critical revision of the manuscript.
All authors reviewed and approved the final version of the manuscript.


