Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Boryana Irinkova* and Iva Petkova
Received: August 21, 2025; Published: September 02, 2025
*Corresponding author: Boryana Irinkova, SHATED “Zora”, Petar Protich str.4, 1750, Sofia, Bulgaria
DOI: 10.26717/BJSTR.2025.63.009842
This study aims to evaluate and compare medium-distance visual outcomes in patients implanted with Comfort and Vario IOLs. A total of 136 eyes were included: 56 eyes with Comfort IOLs, 80 eyes with Vario IOLs. Medium- distance visual acuity at 70 cm was tested for bought IOLs after surgery at different timepoints. Preoperative evaluation of medium-distance vision was omitted due to cataract-induced inaccuracies. Comfort IOLs, utilizing advanced aspheric optics, and Vario IOLs, employing diffractive and refractive designs, were investigated to determine their efficacy in enhancing intermediate visual acuity, a key determinant of daily visual function and patient satisfaction after operation.
Cataract surgery has advanced beyond simple vision restoration to become a procedure that enhances patients’ quality of life through improved visual acuity at various distances [1]. Conventional monofocal intraocular lenses (IOLs) provide excellent distance vision but often necessitate the use of spectacles for intermediate and near tasks [2]. This limitation has led to the development of enhanced monofocal and extended depth of focus (EDoF) IOLs, such as Comfort and Vario lenses, which aim to extend the range of functional vision without compromising visual quality through dysphotopsias [2,3]. Comfort IOLs use refined aspheric optics to increase depth of focus, delivering superior visual acuity at intermediate distances with minimal side effects like glare or halos [4]. These enhanced monofocal lenses are particularly suited for tasks such as computer work, offering a broader focal range while preserving contrast sensitivity [5]. VarioIOLs employ wavefront-shaping or diffractive technologies to create an extended zone of focus [6]. These lenses function by creating a continuous elongated focal zone, thereby providing clearer vision across a broader range of distances, particularly benefiting intermediate vision. This optical design aims to reduce chromatic and spherical aberrations, providing clearer vision across a range of distances, particularly for intermediate tasks [7,8]. Despite the growing use of these lenses, few studies have directly compared their performance at medium distances (around 70 cm), which are critical for modern lifestyle activities. This study aims to compare medium-distance visual outcomes between patients implanted with Comfort and Vario IOLs, evaluating visual acuity, patient-reported visual quality, and satisfaction rates.
Study Design
This prospective, comparative study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review board. Patients undergoing routine cataract surgery were devided into two groups depending on the type of IOL chosen: Comfort IOLs (56 eyes) and Vario IOLs (80 eyes). Preoperative medium- distance vision was not assessed, as the presence of cataracts would compromise measurement accuracy and reliability.
Inclusion and Exclusion Criteria
Patients aged between 55 and 80 years, diagnosed with cataract, and without visually significant ocular comorbidities such as glaucoma, macular degeneration, or diabetic retinopathy were included. Patients with previous ocular surgeries, irregular corneal astigmatism exceeding 1.0 D, or other ocular pathologies impacting visual function were excluded.
Surgical Procedure
All surgeries were performed by 2 surgeons using standard phacoemulsification techniques. IOL power calculation was conducted using optical biometry and Zeiss IOL Master 700 and SRK-T, Hollady, Barrett Universal II formula to optimize refractive outcomes, targeting emmetropia.
Postoperative Assessment
Patients underwent comprehensive ophthalmic evaluations before the operation, at week 2, month three, and six months postoperatively. Medium-distance visual acuity was assessed at 70 cm using specialized ETDRS charts under standardized illumination conditions. The 70 cm test distance was selected to approximate typical computer workstation viewing distance, thereby measuring functional intermediate vision relevant to daily tasks such as monitor use and document reading.
Statistical Analysis
Data were analyzed using descriptive statistics for demographic characteristics and inferential statistics (SPSS-19, Fisher test and Sparman test) to compare visual outcomes between groups. Statistical significance was defined as a p-value less than 0.05.
Comfort IOL: Medium-distance (70 cm) Best-Corrected Visual Acuity Over Time
(Graph 1) Among eyes implanted with the Comfort IOL (n=56), the distribution of decimal visual acuity (VA) at 70 cm improved progressively from 2 weeks to 6 months postoperatively is shown in (Tables 1 & 1A) and the accompanying graph. Improvement is achieved from week 2 to month 6, where over 80% of the subject achieve vision above 0,7. Fisher exact tests comparing timepoints and achieved results demonstrated a significant shift toward better medium-distance VA between 2 weeks and 6 months as well:
• >0.7: 58.9% → 82.1%; p = 0.0129 (2w vs 6m).
• 0.4–0.7: 33.9% → 16.1%; p = 0.0495 (2w vs 6m).
• ≤0.4: 7.1% → 1.8%; p = 0.3601 (2w vs 6m).
Table 1: Distribution of best-corrected medium-distance (70 cm) visual acuity after Comfort IOL implantation (n = 56). Values are n (%).
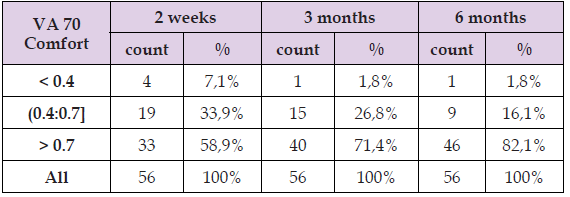
Note: Bold indicates p < 0.05.
No statistically significant changes were observed between 2 weeks and 3 months (>0.7: p = 0.2340; 0.4–0.7: p = 0.5376; ≤0.4: p = 0.3601) or between 3 and 6 months (>0.7: p = 0.2631; 0.4–0.7: p = 0.2496; ≤0.4: p = 1.0000) respectively.
Clinical Interpretation
Most Comfort-implanted eyes achieved functional medium-distance acuity (>0.7 decimal, approximately ~20/30 Snellen) as early as 2 weeks, with additional, statistically significant gains by 6 months. This improvement plateaued between 3 and 6 months, suggesting refractive stability and neural adaptation [9,10]. The pattern is showing the expected postoperative refractive stabilization and continuing neuroadaptation.
Vario IOL: Medium-distance (70 cm) Best-Corrected Visual Acuity Over Time
(Graph 2) Among eyes implanted with the Vario IOL (n = 80), the distribution of medium-distance VA at 70 cm showed progressive improvement from 2 weeks to 6 months as shown in tale 2 and the graphic respective graphic. The statistical analysis shows improvement by month 6, where over 65% of eyes have VA over 0,7 (Tables 2 & 2A).
Table 2: Distribution of best-corrected medium-distance (70 cm) visual acuity after Vario IOL implantation (n = 80). Values are n (%).
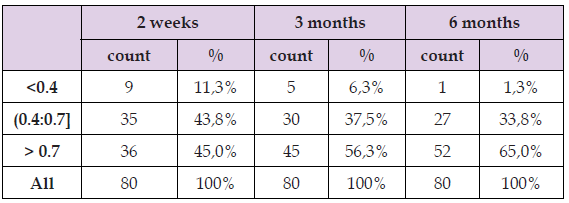
Note: Bold indicates p < 0.05.
The Fisher exact tests demonstrated a significant shift toward better medium-distance VA between 2 weeks and 6 months:
o >0.7: 45.0% → 65.0%; p = 0.0171 (2w vs 6m).
o ≤0.4: 11.3% → 1.3%; p = 0.0222 (2w vs 6m).
o 0.4–0.7: 43.8% → 33.8%; p = 0.2560 (2w vs 6m).
No statistically significant changes were observed between 2 weeks and 3 months (≤0.4: p = 0.4013; 0.4–0.7: p = 0.5197; >0.7: p = 0.2059) or between 3 and 6 months (≤0.4: p = 0.2119; 0.4–0.7: p = 0.7413; >0.7: p = 0.3316).
Clinical Interpretation
Nearly half of Vario-implanted eyes achieved functional medium- distance acuity (>0.7 decimal, ≈20/30 Snellen) as early as 2 weeks, with further improvement to 65% by 6 months. The statistically significant results from 2 weeks to 6 months and the plateau between 3 and 6 months are consistent with postoperative refractive stabilization and continuous neuroadaptation for EDoF optics, very much like the results observed in the Comfort group.
Between-group comparison: Comfort vs Vario at 70 cm (proportion with VA > 0.7)
(Graph 3) Using Fisher’s exact test to compare the proportion of eyes achieving VA > 0.7 at 70 cm between the Comfort and Vario cohorts at matched timepoints showed a significant difference only at 6 months (Tables 3 & 4):
• 2 weeks: Comfort 58.9% vs Vario 45.0%; p = 0.1542 (ns).
• 3 months: Comfort 71.4% vs Vario 56.3%; p = 0.1053 (ns).
• 6 months: Comfort 82.1% vs Vario 65.0%; p = 0.0457.
Table 3: Fisher’s exact p values for between group comparison (Comfort vs Vario) of the proportion with best-corrected medium distance VA > 0.7 (decimal).

Clinical Interpretation
While both IOLs show improvement in medium distance function, by 6 months the Comfort lens demonstrated a higher probability of achieving VA > 0.7 at 70 cm relative to the Vario EDoF design. Early postoperative results (2 weeks, 3 months) show the same direction but did not reach statistical significance. This suggests that, in this population, the Comfort may provide an advantage for medium distance vision by 6 months, though the clinical significance should be measured against other performance points (depth of focus, dysphotopsia), to be tested and analyzed in future studies.
The aim of this study was to explore how Comfort and Vario IOLs perform in real-world, medium-distance vision tasks-things like reading on a screen or viewing objects at arm’s length, which are essential to daily life. While previous research has shown lenses like the Comfort IOL often provide better intermediate vision than standard monofocal lenses-without significant issues like glare or halos-direct comparisons with the Vario, are still relatively scarce. EDoF lenses were specifically designed to address some of the limitations in both monofocal and multifocal IOLs, offering a smoother visual experience across a wider range of distances while minimizing light-related disturbances. Studies on Vario lenses have reported promising results, especially for intermediate tasks, with outcomes often matching or even surpassing those of multifocal lenses when it comes to patient satisfaction. By directly comparing these two technologies, this study provides valuable insight that can help eye care professionals choose the most suitable lens for each patient. Finding the right balance between quality vision, depth of focus, and overall satisfaction is more important than ever, especially as intermediate vision plays an important role in maintaining independence and quality of life.
The results affirm that both IOLs enhance medium-distance vision after cataract surgery. However, Comfort IOLs showed a statistically significant advantage in reaching higher VA at a fixed 70 cm distance. This aligns with prior findings suggesting enhanced monofocal lenses can deliver excellent intermediate vision without the dysphotopsias often associated with multifocal designs [4,5,9]. Vario IOLs also performed well, particularly in their ability to offer a broader continuous focus range, a hallmark of EDoF lenses [7,8,10-11]. While their peak intermediate acuity was slightly lower, their performance may be better across varying intermediate distances, which this study did not measure.
Both Comfort and Vario IOLs significantly improved medium-distance vision after cataract surgery. By 6 months post-op, 82.1% of Comfort IOL recipients achieved functional VA (>0.7) compared to 65.0% with Vario lenses. While Comfort lenses provided slightly better performance at a specific working distance (70 cm), Vario lenses remain valuable for patients seeking a broader range of spectacle-free intermediate vision. Lens selection should be based on individual visual priorities-those focused on specific workstation clarity may benefit more from Comfort IOLs, while those preferring a continuous range may opt for Vario IOLs.
Limitations
This analysis focuses on categorical acuity and the parallel assessments of contrast sensitivity and dysphotopsia are in the process of being analyzed. Future work will incorporate this analysis to broaden and enhance the study.


