Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Bruna Belineli Gomes Frisso Silva1, Rafaella Batista de Oliveira Falkovski2, Emily Cristina Ghiggi2, Steffany Aline Mori Guedes3, Marília Pase4, Edson Oliveira Silva5, Ana Tereza Bittencourt Guimarães6, Carlos Augusto Nassar7 and Patricia Oehlmeyer Nassar7*
Received: May 06, 2025; Published: May 22, 2025
*Corresponding author: Patricia Oehlmeyer Nassar, Department of Periodontology, School of Dentistry, State University of Western Paraná, Cascavel, Paraná, Brazil
DOI: 10.26717/BJSTR.2025.62.009684
Objective: The objective of this study was to evaluate the occurrence of oxidative stress resulting from periodontal
inflammation in the development of VAP in patients admitted to the Intensive Care Unit (ICU).
Method: Clinical, cross-sectional and observational study. Subjects were assessed for the presence or absence
of periodontitis and VAP. 117 patients were evaluated; however, 53 patients were included in the study. Divided
into 3 groups: Control (n=17), periodontitis and without VAP (n=30), Periodontitis and with VAP (n=6). Clinical
periodontal examination, collection and quantification of gingival crevicular fluid, collection of saliva and tracheal
secretion for analysis of the antioxidant system and oxidative stress, hematological tests and other patient
data were performed.
Results: in the clinical periodontal examination, patients with periodontitis, but without VAP, presented significantly
higher values. Hematological tests, urea and creatinine showed significant differences. The variables
related to the antioxidant system and oxidative stress, in saliva, were different in the group of control patients
and in the group with periodontitis, the SOD enzyme was inhibited and LPO was increased. And in the saliva of
the groups of patients with periodontitis, there was an increase in SOD, CAT and GR in the Periodontitis + VAP
group. In the integrative analysis of saliva, Dimension 3 (GST), there was a difference in the group with Periodontitis+
VAP. In the analysis of tracheal secretion in patients with Periodontitis, GR and GST showed significant
induction and inhibition.
Conclusion: The increase in oxidative stress caused by the inflammation of periodontitis can alter the antioxidant
status, facilitating the development of VAP.
Keywords: Periodontitis; Ventilator-Associated Pneumonia; Oxidative Stress; Intensive Care Unit
Abbreviations: ICU: Intensive Care Unit; OS: Oxidative Stress; OTI: Orotracheal Intubation; CPD: Clinical Probing Depth: GM: Gingival Margin; BOP: Bleeding on Probing; CAL: Clinical Attachment Loss; OS: Oxidative stress; LPO: lipid Peroxidation; ROS: Reactive Oxygen Species; PEEP: Positive End-Expiratory Pressure; GR: Glutathione Reductase; GST: Glutathione S-Transferase; CAT: Catalase; SOD: Superoxide Dismutase; SOP: Standard Operating Procedure; MM: Millimeters; GCF: Gingival Crevicular Fluid; CRP: C-Reactive Protein; MB: Mesio-Buccal; DB: Disto- Buccal; CEJ: Cementoenamel Junction
Pneumonia is responsible for affecting the lung parenchyma and can be caused by bacteria, mycoplasmas, fungi, parasites and viruses, with the bacterial cause being the most common [1]. Ventilator-associated pneumonia (VAP) is responsible for inflammation of the lung parenchyma, occurring 48 to 72 hours after orotracheal intubation and the start of mechanical ventilation [2,3]. These patients are under mechanical ventilation through a tracheal tube, undergoing tracheostomy, or may be in the process of disconnecting from the ventilator in the 48 hours prior to the onset of symptoms [3].The high risk of developing VAP is due to the presence of the orotracheal tube, altered levels of consciousness, dry and open mouth, changes in the oropharyngeal flora, oral inflammation, impaired airway self-cleaning mechanism, inhibition of the cough reflex and microaspiration of secretions, allowing the oral cavity to be colonized by pathogenic bactéria [4]. Additionally, individual factors, such as age over 70 years, malnutrition, underlying diseases, depressed level of consciousness, tracheal intubation and reintubation, immunological status, use of immunosuppressive drugs, severity of the disease, aspiration of contaminated secretions, position of the patient in bed and insufficient elevation of the headboard, prolonged time on mechanical ventilation, also contribute to the development of VAP [5,6]. The orotracheal tube provides an inert, non-scaling surface to which bacteria adhere and grow to form biofilms, from which the bacteria are shed and aspirated into the lower airway. Furthermore, the orotracheal tube induces mechanical abrasion, irritation of the respiratory mucosa, impairment of normal laryngeal function, and increased sedation – all leading to an increased risk of aspiration of secretions from the upper respiratory tract [7].
Raghavendram, et al. (2007) also mention that the bacterial microbiota and/or gastric contents may also be important in the pathogenesis of postoperative pneumonia. Although ventilators alone are not considered a major source of bacterial dissemination, respiratory circuits can become heavily contaminated with microorganisms from the oropharynx and trachea [7]. The link between dental plaque/biofilm and VAP has also been studied. The incidence of respiratory tract infections in patients requiring an orotracheal tube is substantial, and the risk of acquiring VAP increases by 1-5% per day of hospital stay [7]. Studies have demonstrated the association between periodontitis and VAP, which is biologically realistic, as bacterial proliferation in individuals with periodontitis can result in colonization of the oropharynx, which facilitates direct aspiration of pathogens and sustains infection, mediated by inflammatory factors and immunological [8- 11]. Saliva is an important physiological component, useful for the diagnosis and monitoring of many oral and systemic pathological conditions. Oxidative stress (OS) markers in saliva have been shown to be a local indicator of the inflammation process, the progression of periodontitis and the amount of periodontopathic bacteria in periodontal pockets [12]. Furthermore, enzyme-laden saliva associated with periodontal disease can modify mucosal surfaces to promote adhesion and colonization by respiratory pathogens. Cytokines originating from periodontal tissues can promote inflammation of the lower airways after aspiration and thus alter the epithelium to promote infection by respiratory pathogens [7].
Oxidative stress is caused by the imbalance between the production of reactive oxygen species and the activity of local endogenous antioxidants [12]. A study by Brock, et al. [13] assessed total antioxidant capacity as an indicator of tissue response in periodontitis and reported its decrease in the saliva of individuals with periodontitis, while SÁNCHEZ-VILLAMIL et al. [12] observed a greater capacity total salivary antioxidant. In view of the above, it is believed that the imbalance in the activity of the antioxidant system in patients with periodontitis increases the risk of oxidative stress, thus facilitating the development of VAP.
The objective of this study is to evaluate the antioxidant system and the occurrence of oxidative stress in development of VAP in patients with and without periodontitis admitted to an ICU.
Type of Study
This is a cross-sectional and observational clinical study, with quantitative analysis of data, including clinical and laboratory basis, aiming to assess the mechanisms by which inflammation caused by periodontitis can lead to the development of VAP in patients admitted to an ICU at a hospital in the macro-region of the city of Cascavel, state of Paraná, Brazil.
Sample Population
The selected patients were evaluated with a complete extraoral and intraoral clinical examination, considering their hospitalization condition, with a focus on diagnosing periodontal changes. In addition to the clinical examination, analysis of hematological tests was carried out, as well as health history, considering the possible association with the periodontal changes evaluated and allowing the correlation of systemic, blood, and periodontal data. The collection of patient characterization data (age, sex, body temperature, exams, and health history) was carried out using the hospital’s information system and electronic medical records – Tasy®. The study was conducted from April 2022 to January 2023 with adult patients using MV for all orotracheal disorders. All patients selected for data collection must be within a period of up to 72 hours of orotracheal intubation (OTI). The effects of the factor’s presence and absence of periodontitis and presence and absence of VAP were evaluated. The interaction of these factors established 4 groups for comparison (Without Perio and without VAP, Without Perio and with VAP, Perio without VAP, and Perio with VAP); however, the group without periodontitis and with VAP had no patients, thereby resulting in a total of 3 groups for the study:
1. Control group (without periodontitis and without VAP): group of patients without periodontitis and who did not develop VAP;
2. Periodontitis without VAP: group of patients with periodontitis who did not develop VAP;
3. Periodontitis with VAP: group of patients with periodontitis who developed VAP.
Inclusion Criteria
Individuals over 18 years old, admitted into the ICU of a reference hospital in the macro-region of western Paraná and patients on mechanical ventilation for a period of 24 to 72 hours and presenting at least six teeth (Almondes et al. [14]).
Exclusion Criteria
Patients with severe maxillofacial trauma, which made the possibility of examination difficult, using complete dentures (upper and lower), pregnant women, immunosuppressed patients, patients using any anti-inflammatory and antibiotic for more than three days, and patients with serious clinical or surgical complications.
Sample Calculation
This sample calculation was carried out a posteriori, as we obtained a sample consisting of 53 subjects. We assumed a t-Student family for the calculation, with an effect size of 0.57 (medium) and a significance level of 0.05, reaching an analysis power of 0.80. The sample calculation was performed using the G-power software.
Clinical Periodontal Examination
The clinical examination was carried out by a previously trained examiner under appropriate ergonomic and lighting conditions in relation to the positioning and inclination of the millimeter probe, as well as in relation to the probe pressure (approximately 25 grams). Training was maintained during data collection and, to carry it out, the examiner used a periodontal mannequin, positioned on the tray of the AX200 precision digital scale (Shimadzu®, Japan), simulating periodontal probing, applying force until reaching the value of 25 grams, using a millimeter periodontal probe, North Carolina model (Millennium®, São Paulo), with a modified pen-shaped handle and keeping the active tip perpendicular to the manikin’s tooth until 10 repetitions are reached [15].
Parameters Evaluated
In sequential order and for convenience, the following were evaluated:
1. Clinical probing depth (CPD): distance from the gingival
margin (GM) to the bottom of the sulcus/pocket with presence or
absence recorded and measured in mm.
2. Bleeding on probing (BOP): every three teeth, with an interval
of approximately 30 seconds, to record the parameter that
corresponds to the probing time, with registration of presence or
absence.
3. Clinical attachment loss (CAL): distance from the cementoenamel junction (CEJ) to the bottom of the sulcus/pocket, with presence or absence recorded and measured in millimeters. Obtained from the sum of gingival recession and clinical probing depth (CAL = GR + CPD) – method used in a clinical study [16].
Dental Groups and Sites Evaluated
Considering that the study population were patients with possible hematological, oral and systemic alterations, who needed practical and minimally invasive examinations, the mouth examination was carried out, excluding third molars. At least 6 teeth were evaluated, with three sites evaluated for each tooth: mesio-buccal (MB), buccal (B) and disto-buccal (DB). The palatal and lingual surfaces were not evaluated, considering that the patients were on invasive mechanical ventilation via an orotracheal tube, thereby making the evaluation difficult and time-consuming [14].
Hematological Tests for Analysis
The results of the laboratory tests were collected on the same day as the other collections. Changes in laboratory tests may also be associated with the emergence of changes in the oral cavity. Therefore, this study analyzed the following parameters:
1. Leukocytes
2. Urea
3. Creatinine
4. C-Reactive Protein (CRP)
Quantification of Gingival Crevicular Fluid (GCF)
Three deeper sites, in millimeters (mm), were selected in different teeth, according to clinical periodontal examination, on the buccal surfaces and with previously detected gingival inflammation, using a #40 absorbent paper cone. The supragingival plaque was carefully removed in accordance with the standard operating procedure (SOP) established in the ICU in question. After the sites were isolated with cotton rolls and dried, the paper cones were then inserted below the gingival margin for 30 seconds and immediately placed in an alcoholic solution of 0.2% ninhydrin (2.2-dihydroxy -hydridene-1.3-dione) for 1 minute. They were then photographed from a distance of 10 cm and analyzed with software (Image Pro Plus® 4.5.0.29, Media Cybernetics, Silver Spring, MD, United States) to determine the amount of fluid absorbed in square millimeters (mm2) [17].
Saliva Collection
Saliva was collected immediately prior to the periodontal clinical examination, using the vacuum system by suction in a clean vacuum tube. Subsequently, the contents were aspirated with a syringe and placed in a single sterile Eppendorf tube. This sample was used to evaluate the antioxidant system (SOD, CAT, GR, GST), as well as the occurrence of oxidative stress. The samples were stored and frozen in a freezer at -70 °C.
Endotracheal Collection
The collection of tracheal secretion was carried out after the periodontal clinical examination and after the patient’s aspiration, by a professional trained for this procedure and using recommended personal protective equipment (PPE). A probe with an appropriate diameter was introduced, connected to the vacuum system via the endotracheal tube, until resistance was encountered. Once the probe reached the ideal amount of secretion, it was clamped and disconnected from the suction extender. Subsequently, the collected material was placed in a single sterile Eppendorf tube and frozen in a freezer at -70 ºC, for subsequent analysis of the antioxidant system (SOD, CAT, GR, GST), as well as oxidative stress.
Diagnostic Criteria for VAP
Notifications for the diagnosis of VAP were provided through a report from the Hospital Infection Control Commission (Comissão de Controle de Infecção Hospitalar – CCIH), based on the book Critérios Diagnósticos de Infecção Relacionada à Assistência à Saúde (“Diagnostic Criteria for HealthCare-Related Infection”) from the Brazilian Health Regulatory Agency (Agência Nacional de Vigilância Sanitária – ANVISA), referring to the year 2017 (Agência Nacional de Vigilância Sanitária [18]) and 2021 (Agência Nacional de Vigilância Sanitária [18]) [19].
Sample Preparation
Saliva and tracheal secretion samples were homogenized in Tris- HCl buffer pH 7.4, centrifuged at 13,680 ց and 4 ºC for 10 minutes and then placed in an ultra-low temperature freezer at -80 ºC. At the time of analysis, the samples were thawed, but kept cold during all procedures, as described below. Protein determination followed the Bradford method (1976), using bovine serum albumin as a standard, with reading at a wavelength of 595 nm [20].
Antioxidant system
Superoxide dismutase (SOD) activity was evaluated according to the modified method proposed by Crouch, et al. [21]. The principle of this analysis consists of quantifying the complex formed between superoxide and tetrazolium blue (NBT), measured at 600 nm for 1.5 hours. An aliquot of 0.75 mg/mL of protein in 25% ethanol was prepared in a volume of 800 μL and centrifuged at 13680 g (4 °C) for 20 minutes. From the supernatant, the reaction medium was prepared in a 96-well microplate. In triplicates, in a final volume of 200 μL containing 0.1 mg of protein. mL-1, 0.09 mM NBT, 0.015 mM EDTA, 34.78 mM hydroxylamine sulfate, 79 mM sodium carbonate buffer pH 10.2 and the plate read at 22 °C. One unit of SOD in nmol min-1 mg protein-1. Catalase (CAT) activity was accompanied by a decrease in absorbance at 240 nm [22] in a reaction system consisting of 1.0 M Tris-HCl buffer, 5.0 mM EDTA, pH 8.0, deionized water and 180 μl of H2O2 (30%, d=1.1 g.ml-1, MM = 34 g.mol-1; final concentration in the assay = 30 mM). The unit for expression of catalase activity was mmol of H2O2 min-1 mg of protein-1. The activity of the enzyme glutathione S-transferase (GST) was also evaluated using the methodology of Keen, et al. [23].
The activity of this enzyme was measured for 5 minutes, at intervals of 30 seconds, with an assessment of the increase in absorbance due to the formation of a thioether, at an n-1 in 1 mL of ethanol. GST activity is expressed in μmoles of thioether min-1 mg of protein-1. Glutathione reductase (GR) activity was evaluated according to the technique proposed by Sies, et al. [24]. The reaction system consisted of phosphate buffer 100 mmol L-1 (pH 7.0), EDTA 1 mmol L-1, GSSG 0.66 mmol L-1, NADPH 0.075 mmol L-1. The reaction will be initiated by the addition of GSSG and monitored for 5 minutes at 340 nm. The results will be expressed as NADPH oxidized min-1 mg protein-1.
Oxidative Stress
Oxidative stress was assessed by measuring lipid peroxidation, analyzing the product of the reaction of thiobarbituric acid with malondialdehyde, measured in a spectrophotometer at 535 nm and expressed in nmol of MDA.mg-1 of protein [25].
Statistical analysis
In the first stage of analysis, the quantitative variables referring to clinical analysis were evaluated for normality (Shapiro-Wilk Test) and homoscedasticity (Bartlett Test), considering the Control groups (without Periodontitis and without VAP), Periodontitis, and Periodontitis + PAV. Since the data failed to agree with these assumptions, the variables were compared between the groups using the Kruskal-Wallis non-parametric test, followed by Dunn’s follow-up test. Qualitative variables were compared between groups using the Chi Square test for Independence, followed by the Adjusted Residuals test. Next, assessments of normality and homoscedasticity of data from biochemical analysis of tracheal secretion and saliva were carried out, considering patients with and without periodontitis. Since the data failed to agree with these assumptions, the variables were compared between the groups (Normal – without periodontitis, and Periodontitis) using the non-parametric Mann-Whitney-U test. Afterwards, the same procedure was performed, considering, however, only patients with periodontitis and comparing them between patients who developed VAP and those who did not (normal). Finally, the matrices of tracheal secretion and saliva variables from the Control (without Periodontitis and without VAP), Periodontitis and Periodontitis + VAP groups were separated, standardized by the Z-score and subjected to multivariate principal component analysis (PCA). The factor loadings of the first three main components were compared between the groups using Single Factor Variance Analysis, followed by the Tukey-HSD test, as the data were within normality and homoscedasticity. All analyses carried out assumed a level of significance of 0.05, being carried out in the R program (R Core Team, 2023).
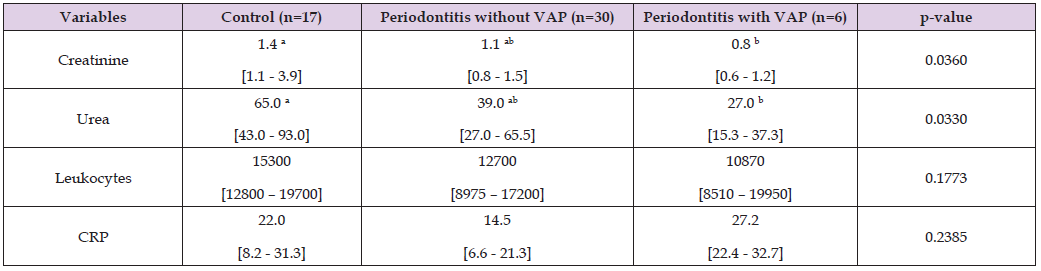
A total of 117 patients on mechanical ventilation via orotracheal tube (MV/OTT) were evaluated during the period from April 2022 to January 2023 and after applying the inclusion and exclusion criteria, with 53 patients were included in the study (Figure 1), and excluded patients being for reasons relating to: edentulism, being hemodynamically unstable during the examination period, or being underage. Given that no patient was included in the group without periodontitis and with VAP, patients were divided into 3 groups, with a total of 23 women and 30 men with a mean age of 49.8 years, with no differences between the mean ages. between the 3 groups (Table 1). Regarding clinical variables, it was possible to verify significant statistical differences in CPD, CAL, and BOP (p<0.05). The other variables did not show significant statistical differences between the groups (p>0.05) (Table 2). Regarding CPD, CAL and BOP, it was found that the group of patients with periodontitis, but without VAP, presented significantly higher values than the Control group, but similar to the group with periodontitis and VAP (p=0.0004; p=0.0003; p=0.0072) (Table 2). Regarding hematological tests, it was possible to verify significant statistical differences only in creatinine and urea (p<0.05) (p=0.036; p=0.033). The other variables did not present significant statistical differences between the groups (p>0.05), making it possible to verify that the values were higher in the Control group (without periodontitis and without VAP), intermediate in the Periodontitis group and reduced in the group with Periodontitis and with VAP (Table 3). Different letters indicate statistical differences between groups.
Table 1: Absolute frequencies and percentages (in parentheses) for sex and medians and interquartile ranges for age of patients in the groups. P-value of the Kruskal-Walli’s test.
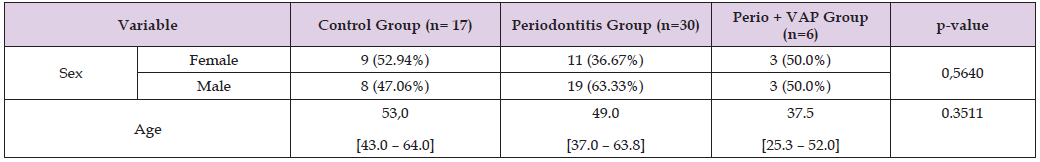
Table 2: Medians and interquartile ranges for clinical parameters between the groups studied. Cascavel, different letters indicate statistical differences between groups. P-value obtained using the Kruskal-Walli’s test.

Table 3: Medians and interquartile ranges of the hematological tests of the groups studied. Cascavel, 2022 Different letters indicate statistical differences between groups. P-value obtained using the Kruskal-Walli’s test.
P-value obtained using the Kruskal-Wallis test. When evaluating the variables related to the antioxidant system and oxidative stress in the saliva of patients without and with Periodontitis, it was possible to see a tendency towards inhibition of SOD activity (p=0.070) and an increase in oxidative stress expressed by an increase in the lipoperoxidation reaction (p= 0.014; Figures 2A & 6E). When considering only patients with Periodontitis, it was possible to observe that there was a significant induction of the activity of the enzymes SOD, CAT and GR (p=0.022, p=0.048, p=0.060, respectively; Figures 3A-3C), in patients with Periodontitis-Associated VAP, which possibly led to a reduction in the lipoperoxidation reaction (p=0.034; Figure 3E). Since systems in an organism act in an integrated manner, it is necessary to carry out a correlational assessment between the variables analyzed through Principal Component Analysis (PCA). In the integrative analysis of saliva (Figure 4), the first principal component (Dimension 1 – Dim.1) presented the greatest contribution associated with the activity of LPO, SOD, and GR (Eigenvalue = 1.64; Variability = 32.78%). The second main component (Dimension 2 – Dim.2) presented a greater contribution from the CAT enzyme (Eigenvalue = 1.04; Variability = 20.87%). The third main component (Dimension 3 – Dim.3) presented a greater contribution from the GST enzyme (Eigenvalue = 0.94; Variability = 18.70%). When comparing the factor loadings of the dimensions, Dimension 1 did not show a statistically significant difference between the groups (p > 0.05). Dimension 2 (CAT) showed a statistically significant difference between the groups (F=3.43; p=0.040), with the group with Periodontitis + VAP showing significantly higher positive scores when compared to the Control group, which represents the induction of CAT activity (p<0.05). The group with Periodontitis presented intermediate values, being statistically equivalent to both the group with Periodontitis + VAP and the Control group (p>0.05).
In relation to Dimension 3 (GST), it was possible to observe a significant statistical difference between the groups (F=4.75; p=0.013), with the group with Periodontitis + VAP presenting significantly higher positive scores when compared to the Control and Periodontitis groups., representing the induction of GST activity (p<0.05). When evaluating the variables related to the antioxidant system and oxidative stress of the tracheal secretion of patients without and with Periodontitis, it was possible to verify that the enzymatic system (SOD and CAT) and GR, belonging to the auxiliary system of the antioxidant system, did not present statistically significant differences (p > 0.05; Figures 5A-5C). Conversely, GST, belonging to the auxiliary antioxidant system and responsible for detoxification processes, as well as lipoperoxidation showed statistically significant reductions between the groups studied (p=0.002 and p=0.026; Figures 5D-5E). When considering only patients with Periodontitis, it was possible to notice that the enzymatic system composed of SOD and CAT did not present statistically significant differences (p>0.05; Figures 6A-6B), as well as lipoperoxidation (p=0.257; Figure 6E). Conversely, the auxiliary enzymes, GR and GST, presented significant induction and inhibition, respectively (p=0.006; p=0.072), when comparing the VAP group with the group without VAP.
Among the tracheal secretion samples (Figure 7), the first main component (Dimension 1 – Dim.1) presented the greatest contribution associated with CAT activity and lipoperoxidation reaction (Eigenvalue = 1.64; Variability = 32.71%). The second main component (Dimension 2 – Dim.2) presented a greater contribution from the enzymes of the auxiliary system GR and GST (Eigenvalue = 1.23; Variability = 24.58%). The third main component (Dimension 3 – Dim.3) presented a greater contribution from the SOD enzyme (Eigenvalue = 1.04; Variability = 20.75%). When comparing the factor loadings of the dimensions, only Dimension 2 (GR and GST) showed a statistically significant difference between the groups (F=4.00; p=0.026). Positive Dim.2 scores indicate higher GST enzymatic activity and lower GR activity. The group of patients with Periodontitis and VAP were significantly different from the other groups, characterized by negative scores, thus indicating greater GR activity and lower GST activity.
Most critically ill patients require MV to facilitate survival. An OTT provides the interface between the patient and the ventilator and after insertion of the tube, with the possibility of changes occurring in the oral microenvironment and microbiome. The mechanisms underlying this “microbial displacement” are unclear, but may, in part, be due to the physical presence of OTT, which affects plaque removal, saliva flow, and mucosal dryness, in addition to interventions and medications related to the management of the underlying condition during critical illness [26].When evaluating the oral health condition of the patients this present study, it was possible to observe that the BOP was higher in the groups with periodontitis, when compared to the control group, although it was not significant between the Periodontitis + VAP and control groups. Similarly, there were no significant differences in the periodontal parameters of CPD and CAL in control patients and patients with periodontitis + VAP, corroborating the study by Almondes et al. [14], which also found no significant differences in periodontal parameters between the case groups (patients with VAP) and control (patients without VAP). In fact, this author showed that the control group presented worse periodontal conditions in relation to probing depth and loss of clinical attachment. According to Scannapieco, et al. [27,28], there is a tendency for attachment loss to increase when lung function is reduced, which did not occur in this study, which showed that there was no significant difference in CAL between the periodontitis and periodontitis + VAP groups. The occurrence of lung injury may also affect the kidneys. Ventilator-induced lung injury is the most studied example of lung-kidney interaction. MV causes hemodynamic abnormalities, which can, in turn, affect renal perfusion by reducing cardiac output, as well as hormonal and sympathetic pathway stimulation [29]. In this study, a significant increase in urea and creatinine values was observed in the control group.
Abreu, et al. [29], when examining the factors associated with acute kidney injury and outcome in patients with lung disease, observed that the comparison between survivors and non-survivors showed that those who did not survive had a higher frequency of need for MV, levels more him lower PEEP (positive end-expiratory pressure) on admission, higher urea levels on admission and more frequently required dialysis. It is known that high PEEP values decrease urinary flow, urinary sodium excretion and creatinine clearance. This study did not evaluate PEEP levels or the presence or development of acute kidney injury in patients. Su, et al. [30], when evaluating the levels of Triggering Receptor expressed on myeloid cells 1 (TREM-1), procalcitonin and the pulmonary infection score in the diagnosis and prognosis of VAP, observed that comparing the non-VAP group with the group VAP, had significant changes in temperature, oxygenation index, sTREM-1 levels, procalcitonin levels, leukocyte count, CRP concentration. In this study, there were no differences in temperature or leukocyte counts and CRP in the groups evaluated. It should be noted that no study has compared these blood parameters in patients on MV with and without periodontitis, with and without VAP, nor the mechanisms by which periodontal inflammation may contribute to the development of VAP in patients on MV due to OTT.
Increasing evidence suggests that reactive oxygen species (ROS) are involved in the pathogenesis and progression of periodontitis. Low ROS levels are essential in several biochemical processes. They may, however, cause tissue damage through multiple mechanisms, including DNA damage, lipid peroxidation (LPO), and protein damage, as well as enzymatic oxidation. Oxidative stress (OS) occurs when cellular antioxidant defense is inadequate to completely inactivate ROS generated due to excessive production, loss of antioxidant defense, or both [31]. When performing saliva analysis, it was observed in the comparison between patients with and without periodontitis that the SOD enzyme was inhibited and the LPO reaction was increased among patients with this inflammation, thereby indicating the inhibition of the activity of the antioxidant system and a state of oxidative stress when compared to the Control group (without periodontitis). Other similar studies obtained similar results, with increased levels of oxidative stress in saliva in patients with periodontitis when compared to the control group [12,31-34]. analyzed gingival tissues from patients with severe periodontal disease and showed that the activity of SOD and CAT in these tissues was reduced. When analyzing only patients with Periodontitis and comparing those who did or did not develop VAP, it was found that the SOD, CAT and GR enzymes were more active in the group of patients with VAP, which may have led to a reduction in OLP. GR is present in high concentrations in bronchoalveolar lavage, providing protection to the lung against oxidative injury. Its importance is confirmed in studies where its depletion has been related to a greater risk of lung disease [35], unlike this study, in which antioxidant enzymes in the lung were increased, not even being altered by the oxidative stress of the periodontitis.
Considering that the entire enzymatic framework of a cell is interrelated, integrative analyses become relevant to enable an understanding of the functioning of the cellular machinery. In the integrative analysis of saliva, the group with Periodontitis + VAP showed a significant induction of CAT and GST activity when compared to the Control group (without periodontitis and without VAP). To combat ROS formed in the extracellular space or of exogenous origin, the respiratory tract relies on antioxidant defenses present in the fluid that covers the surface of its epithelium. The extracellular antioxidants present in this fluid include catalase, SOD, GSHPx, GSH [36], which may justify the induction of these enzymes. Additionally, studies report that oxidative stress resulting from periodontal disease has effects on systemic inflammation, such as respiratory disease [37,8].
Thus, in this study, when evaluating the variables related to the antioxidant system and oxidative stress of tracheal secretion considering only Control patients (without periodontitis) and with Periodontitis, a reduction in GST activity and a lower state of oxidative stress was observed, characterized by a reduction from LPO. GST comprises a group of enzymes capable of detoxifying a variety of compounds, including xenobionts derived from pathogenic microorganisms, catalyzing their conjugation with GSH [38]. An increase in the action of GST is able to combat the effects of ROS produced in the endogenous detoxification process or from exogenous sources [39], which differs from this study, or because periodontitis would not have reached a degree of severity sufficient to alter the lung’s antioxidant enzymes. When evaluating only patients with Periodontitis, it was possible to notice that the enzymatic system composed of SOD and CAT did not present significant statistical differences, as did lipoperoxidation. Conversely, the auxiliary enzymes, GR and GST, showed significant induction and inhibition, respectively (p=0.006; p=0.072), when comparing the VAP group with the group without VAP. Glutathione (GSH) has a vital protective function, at the intra- and extra-cellularly level, against oxidative stress in the lungs [40]. Changes in glutathione (GSH) metabolism in alveoli and lung tissue are widely recognized as a key feature of a number of lung diseases [41].
GSTs do not use hydrogen peroxide as a substrate but are able to catalyze the GSH-dependent reduction of non-physiological hydroperoxides [42], thereby demonstrating that there may be an imbalance in the antioxidant system in these patients. Although the number of patients in the Periodontitis + VAP group was reduced (n=6), these results may strengthen the hypothesis that the existing imbalance in the antioxidant system of patients with periodontitis may be a risk factor for the development of VAP, as the inflammatory profile of periodontitis causes the release of lymphocytes, which when activated, produce a large amount of ROS [37], thereby justifying these results and the objective of this study, considering that, to date, no other study has evaluated this mechanism in relationship between the two diseases. VAP results found in this study may have occurred due to the Saúde em Nossas Mãos (“Health in Our Hands”) project, which was implemented at HUOP in 2021.
The project was developed collaboratively by the PROADI-SUS hospitals, and the technical teams of the Coordinator’s Office of the National Program for Patient Safety (Coordenação do Programa Nacional de Segurança do Paciente – PNSP), General Coordinator’s Office of Hospital and Emergency Care of the Hospital Care Department of the Health Care Secretariat (Coordenação Geral de Atenção Hospitalar e de Urgência do Departamento de Atenção Hospitalar da Secretaria de Atenção à Saúde – CGHOSP/DAHU/SAS/MS).Aligned with the National Health Plan (Plano Nacional de Saúde – PNS), Saúde em Nossas Mãos (“Health in Our Hands”) hopes to reduce, in the medium term, the incidence of the main indicators of hospital infection, in addition to disseminating the improvement model to other units and hospitals, as well as demonstrating the financial impact from the prevention of infections. In the long term, the expectation is to contribute to changing the culture of healthcare organizations regarding patient safety. Between 2021 and 2023, Saúde em Nossas Mãos had the participation of 204 hospitals, including HUOP – Cascavel. The main limitation of this study was the small sample size of the periodontitis + VAP group, due to the reduction in VAP during the collection period, probably due to the Saúde em Nossas Mãos project. Therefore, studies with a larger sample and longer collection time are necessary to confirm the imbalance of the antioxidant system and the occurrence of oxidative stress as a mechanism for the development of VAP in patients with and without periodontitis admitted to the ICU.
According to the results obtained and based on the clinical significance of the results, it can be concluded that the increase in oxidative stress caused by the inflammation of periodontitis may lead to an imbalance in the antioxidant status, thereby facilitating the development of VAP. Clinical studies with larger samples and longer collection times are needed to confirm these findings.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
The authors have no relevant financial or non-financial interests to disclose.
All regulations for conducting studies with human beings were followed, with approval from the UNIOESTE Human Research Ethics Committee, under opinion Nº 5.340.334.
The objective and nature of the study were explained to all companions/ guardians of the patients, and they were included as study participants after agreeing and signing the informed consent form (ICF).
All authors contributed to the study conception and design.
Bruna Belineli Gomes Frisso Silva, Rafaella Batista de Oliveira Falkovski, Emily Cristina Ghiggi, Steffany Aline Mori Guedes, Marília Pase and Edson Oliveira Silva - clinical and experimental studies, data and statistical analysis; manuscript preparation, editing and review. Ana Tereza Bittencourt Guimarães- experimental studies, data and statistical analysis; manuscript preparation. Carlos Augusto Nassar, Patricia Oehlmeyer Nassar - definition of intellectual content; design; clinical and experimental studies, data and statistical analysis; manuscript preparation, editing and review. [9] To whom correspondence should be addressed at Torres Avenue, number 200, house 249, FAG, Cascavel, Paraná Postal Code 85806-095, Brazil.
This study had financial support from the State University of Western Paraná - UNIOESTE and CAPES. (Coordination for the Improvement of Higher Education Personnel). The authors would like to thank the doctors and physiotherapists of the ICU - HUOP -UNIOESTE for their collaboration in the research.


