Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Boffo Aborasomalah*1 and Anthony Kwame Apedzi2
Received: January 08, 2025; Published: March 05, 2025
*Corresponding author: Boffo Aborasomalah, Ghana Health Service, Ghana
DOI: 10.26717/BJSTR.2025.60.009517
Introduction: This is an appraisal of the coping mechanism used by tuberculosis in managing their health challenges
in the Adentan municipality, focusing on the interventions in place, and highlighting the strengths and the
areas that need improvement in the healthcare system.
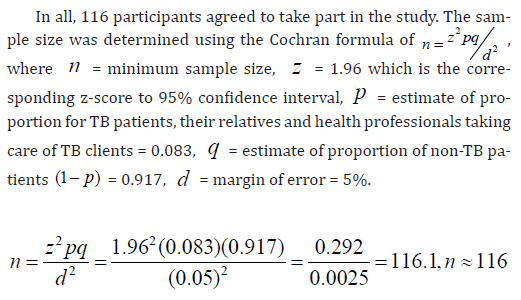
Methodology: A quantitative research method was used. The study targeted adult TB patients currently undergoing
or have completed treatment in selected healthcare facilities from 2020 to 2024, their relatives, and
healthcare providers. A number of 116 patients participated in the research.
Findings: Most respondents sought help from healthcare facilities upon noticing symptoms, demonstrating the
importance of the availability and proximity of healthcare services. Supporting systems for TB patients were
found to be robust, with a higher level of family and self-support and additional support provided by healthcare
facilities.
Conclusion: Supporting systems for TB patients were found to be robust, with a higher level of family and
self-support and additional support provided by healthcare facilities. These findings emphasize the crucial role
of comprehensive support involving financial, nutritional, psychological, and emotional assistance in the effective
management of TB.
Abbreviations: SDGs: Sustainable Development Goals; TB: Tuberculosis; DOTS: Directly Observed Therapy Short-course; WHO: World Health Organization; DR-TB: Drug-Resistant Tuberculosis
The appraisal of a coping mechanism of tuberculosis patients in urban centers especially in Africa needs to be studied to understand how they are managing it to inform decisions. Tuberculosis (TB) is a common communicable disease known worldwide. Studies show that it is caused by Mycobacterium tuberculosis which is a group of bacillus complex which can be transmitted through droplets while coughing, sneezing, shouting, or singing (Tadele, et al. 2022). Over the years, there has been a lot of improvement in the treatment of the disease. Despite the advancement in treatment, it still remains a public health concern. In 2017, approximately 10 million new Tuberculosis (TB) cases were recorded globally, resulting in 1.6 million deaths and 558,000 cases of rifampicin-resistant TB (Tesema, et al. [1]). Similarly, in 2018, 10 million individuals were diagnosed with TB worldwide, with nearly 1.5 million succumbing to the disease (Sylverken, et al. [2]). To combat the TB epidemic, the Directly Observed Therapy Short-course (DOTS) strategy has been adopted internationally as an effective cure for TB (Tetteh, et al. [3]). Between 2000 and 2017, TB diagnosis and treatment saved approximately 54 million lives, contributing to the goal of achieving the United Nations Sustainable Development Goals (SDGs) target of ending the TB epidemic by 2030 (Tesema, et al. [1]).
The DOT component accounts for about 75% of the provider costs of TB treatment, requiring patients to complete their treatment under the supervision of a trained and monitored treatment partner or supporter to ensure adherence (McLaren, et al. [4]). Its implementation relies on key pillars, including government commitment, case detection through passive case-finding, standardized short-course chemotherapy under proper case management, consistent drug supply, and a robust monitoring system for program evaluation and supervision. Despite these efforts, approximately 37% of new TB cases remain undiagnosed, particularly in Sub-Saharan Africa, though some improvements in detection and treatment rates have been reported (WHO [5]). Treatment success rates in the region remain critically low (Ejeta, et al. [6]). In Ghana, TB continues to be a significant public health issue, impeding development due to weak health infrastructure and inadequate case detection and management (Akese [7]). A recent TB prevalence survey indicated a prevalence of smear-positive TB of 111 per 100,000 among adults, with bacteriologically confirmed cases at 356 per 100,000 (Sylverken, et al. [2]). Although TB is a notifiable disease in Ghana, diagnostic challenges hinder early case identification and treatment. While an estimated 45,000 TB cases should be reported annually, only about 33.33% are detected, leaving many undiagnosed (Yahaya, et al. [8]).
Preliminary results from a nationwide survey revealed a national prevalence rate of 264 per 100,000, a bacteriological prevalence of 356 per 100,000, and a smear-positive rate of 105 per 100,000 (Ghana Health Service, 2015). These figures highlight the significant health risks posed by TB in Ghana, despite the implementation of the DOTS strategy (National TB Control Program, NTP, 2013). Effective TB management requires a multifaceted approach that includes early diagnosis, prompt and adequate treatment, and consistent monitoring to ensure adherence and prevent drug resistance (Uplekar, et al. [9]). However, TB patients often face numerous challenges, including physical side effects from prolonged drug therapy and psychological stressors such as stigma, fear, and isolation (Courtwright, et al. [10]). These challenges can adversely affect treatment adherence, leading to poor health outcomes and further transmission of the disease. Coping mechanisms play a critical role in managing these challenges. Coping strategies refer to individuals’ cognitive and behavioural efforts to handle stressful situations’ demands (Lazarus, et al. [11]). For TB patients, these strategies range from positive approaches, such as seeking social support and adhering to medical advice, to negative responses like denial or substance abuse (Shin, et al. [12]). Understanding these mechanisms is essential for healthcare providers to design interventions that address TB management’s clinical and psychosocial aspects.
Despite the acknowledged importance of coping mechanisms in TB treatment, limited research has explored the specific strategies patients use and their impact on treatment outcomes. This knowledge gap underscores the need for comprehensive assessments of the challenges faced by TB patients and the coping strategies they adopt. Such assessments are crucial for developing holistic, patient-centered care models that improve adherence, enhance the quality of life and reduce the global burden of TB.
Many countries, with support from the World Health Organization (WHO), have implemented various initiatives to control tuberculosis (TB). Ghana, like many others, has adopted WHO-recommended strategies for TB treatment and control. Despite these efforts, TB remains a significant public health challenge in the country. According to WHO estimates, Ghana should report approximately 45,000 TB cases annually, yet only about one-third of these cases are detected, with around 12,000 resulting in death (Yahaya, et al. [8]). TB affects not only those currently battling the disease but also the quality of life for those who have completed treatment. Drug-Resistant Tuberculosis (DR-TB) further exacerbates the problem, imposing substantial physical, psychological, and socioeconomic burdens on individuals and households. DR-TB poses a critical threat to the progress made in TB control and care. Additionally, the lengthy treatment regimen and the high number of daily medications present significant challenges for patients (Gyimah, et al. [13]). Globally, TB remains a pressing health issue, with an estimated 10 million people contracting the disease annually, despite it being preventable and curable (WHO [14]). Managing TB is particularly difficult in resource-limited settings, where access to adequate healthcare, nutrition, and social support is often constrained. These limitations contribute to poor treatment adherence, an increased risk of drug-resistant TB, and higher mortality rates (Kyu, et al. 2018).
One of the primary challenges in TB management is the prolonged and complex nature of the treatment, which typically lasts six months or more and requires multiple antibiotics. This extended duration often leads to patient fatigue, reduced medication adherence, and potential treatment failure or relapse (Chang, et al. [15]). Furthermore, side effects such as hepatotoxicity and gastrointestinal disturbances add to the difficulty of maintaining consistent adherence (Lee, et al. [16]). Social determinants of health, including poverty, stigma, and limited education, also complicate TB management. Many TB patients experience stigma and discrimination due to the infectious nature of the disease, leading to social isolation and mental health challenges such as depression and anxiety (Courtwright, et al. [10]). Additionally, TB disproportionately impacts individuals from lower socioeconomic groups, who often face financial barriers, transportation difficulties, and loss of income during their illness (Barter, et al. [17]). Coping mechanisms among TB patients vary significantly based on individual resilience, social support systems, and access to healthcare resources. While some patients rely on family and community support to adhere to treatment and manage the psychological impact of the disease, others may resort to harmful behaviours, such as substance abuse, as a way to cope (Shin, et al. [12]). Understanding these coping strategies is essential for developing targeted interventions that address both the clinical and psychosocial aspects of TB care.
Despite recognition of these challenges, there remains a lack of comprehensive strategies that integrate medical treatment with psychosocial support to improve TB management outcomes. This gap highlights the need for further research into the specific health challenges faced by TB patients and the coping mechanisms they employ. Such research is critical to inform the development of holistic care models that improve treatment adherence, reduce drug-resistant TB, and enhance the overall quality of life for patients. While several studies in Ghana have examined the treatment outcomes of TB patients on Directly Observed Therapy Short course (DOTS), no research has yet been conducted in the Adentan municipality to explore the challenges faced by TB patients during treatment and the coping mechanisms they adopt. This study seeks to address this gap by assessing the health challenges and coping strategies of TB patients in the Adentan municipality.
Research Objective
To identify the coping mechanisms employed by TB patients in the Adentan Municipality.
Research Question
How do TB patients cope with the infection and its management?
Significance of the study
This study is significant because it aims to deepen the understanding of the health management challenges faced by TB patients and the coping mechanisms they employ, which are critical factors influencing treatment outcomes and overall quality of life. This exploration of the coping mechanisms utilized by TB patients offers important implications for enhancing treatment adherence. By identifying both positive and negative coping strategies, healthcare providers can develop tailored interventions that support patients in adopting more effective coping mechanisms, thereby improving adherence rates and reducing the incidence of drug-resistant TB. TB management has traditionally focused on the biomedical aspects of the disease, often overlooking the psychosocial dimensions that are equally critical to patient outcomes. This study is significant because it advocates for a more holistic approach to TB care that integrates medical treatment with psychosocial support. This holistic approach is essential for improving the overall well-being of TB patients and achieving better long-term health outcomes. Given the global nature of the TB epidemic, the findings of this study have the potential to contribute to broader TB control efforts. By highlighting the importance of addressing patient-centred challenges and supporting effective coping mechanisms, this research can inform global health policies and programs aimed at reducing the burden of TB.
Finally, this study is significant because it opens avenues for future research on TB management and patient care. The detailed assessment of health management challenges and coping mechanisms provides a foundation for further studies that can explore these issues in different contexts and among diverse populations. Such research is vital for developing culturally appropriate and context-specific interventions that can enhance TB care and improve patient outcomes across different regions.
Scope of the study
This study investigates the health management challenges and coping mechanisms of tuberculosis (TB) patients using a quantitative research approach. It focuses on adult TB patients who are either currently undergoing treatment or have completed it between 2020 and 2024, along with their relatives and healthcare providers. The study population includes individuals from both urban and rural settings to capture a broad spectrum of experiences and challenges related to TB management. The research was conducted in the Adentan municipality of the Greater Accra region of Ghana, encompassing all healthcare facilities involved in TB-related activities. These facilities reflect varying levels of healthcare access and socioeconomic conditions, providing a comprehensive understanding of the challenges faced by TB patients. The study examined key variables associated with TB management challenges, including economic barriers, difficulties accessing Directly Observed Therapy Short courses (DOTS), and issues related to healthcare service accessibility. It also explored the psychological and social impacts of TB, such as stigma and isolation.
Additionally, the research investigated coping mechanisms adopted by patients, ranging from adaptive strategies like seeking social support and adhering to medical advice to maladaptive behaviours. A standardized questionnaire was employed to collect data from TB patients, designed to assess the extent of their challenges and coping strategies.
Quantitative methods were used for data analysis, incorporating descriptive statistics to summarize the study population’s characteristics and inferential statistics to examine relationships between health management challenges and coping mechanisms. The study aims to identify significant factors influencing treatment adherence and patient outcomes, contributing to the development of more effective TB management strategies.
Limitation
While the study attempted to cover a broad range of coping mechanisms, it was not able to fully capture the complexity of individual coping strategies, particularly those influenced by cultural, religious, or personal factors that are difficult to quantify. Qualitative methods could provide deeper insights into these aspects but are not within the scope of this quantitative study.
Tuberculosis (TB) remains a significant global health issue, with high rates of morbidity and mortality, particularly in developing countries. According to the World Health Organization (WHO [18]), an estimated 10 million people contracted TB in 2021, resulting in 1.6 million deaths. The disease primarily affects adults in their most productive years, imposing substantial economic and social burdens. TB is among the top 10 causes of death globally and remains the leading cause of death from a single infectious agent (WHO [18]). Low- and middle-income countries bear the brunt of the burden, accounting for over 95% of TB cases and deaths (Centers for Disease Control and Prevention [CDC] [19]). In developing countries, citizens face numerous challenges that increase their vulnerability to TB. Limited healthcare infrastructure, poverty, inadequate nutrition, and environmental factors such as overcrowded living conditions, poor ventilation, and dusty surroundings contribute significantly to the spread of the disease. Additionally, lifestyle factors like smoking, alcohol consumption, and substance abuse further heighten the risk of contracting TB. Adults in their economically productive years often engage in extensive social interactions while striving to earn a livelihood, inadvertently increasing their risk of both acquiring and transmitting the disease. Many fail to take conscious measures to protect themselves or others, exacerbating the cycle of infection and spread.
Tuberculosis (TB) remains a pressing public health issue in Ghana, with the World Health Organization (WHO [14]) identifying the country as having a high TB burden. Urban areas, particularly densely populated municipalities, face additional challenges due to socioeconomic factors and limitations in healthcare infrastructure (Nyaaba, et al. [20]). Many urban residents belong to the middle-to-lower socioeconomic class and live under unfavourable conditions such as slum areas characterized by overcrowding, inadequate healthcare facilities, low income, poor nutrition, alcoholism, and smoking. These factors significantly increase their vulnerability to TB. Ghana is among the 30 high TB burden countries, with an estimated incidence rate of 156 cases per 100,000 population in 2021 (National Tuberculosis Control Program [NTP] [21]). Managing TB in the country is fraught with challenges, including insufficient healthcare infrastructure, limited access to diagnostic services, delays in seeking treatment, and stigma associated with the disease. The high burden of TB in Ghana is further compounded by factors such as poverty, overcrowded living conditions, and the high prevalence of HIV, which increases susceptibility to TB (Getahun, et al. [22]). Many individuals in overcrowded and impoverished settings often engage in risky behaviours such as unprotected sex, substance abuse, and excessive alcohol consumption, further predisposing them to TB.
In 2021, Ghana recorded an estimated TB incidence rate of 152 cases per 100,000 population (Ghana Health Service [GHS] [23]), reflecting the urgent need for targeted interventions to address these multifaceted challenges. This research seeks to identify the barriers to accessing Directly Observed Therapy Short-course (DOTS) among tuberculosis (TB) patients in the Adentan municipality, assess how these barriers impact TB control efforts, and propose strategies to address them. By examining qualitative studies from India, China, and Ghana, the research gains a broader perspective on the obstacles TB patients encounter in accessing DOTS. These studies confirm the existence of significant barriers and, due to their qualitative nature, provide detailed insights from participants about their experiences. However, none of these studies were conducted in the Adentan municipality, with the Ghana-based study focusing on the Western Region. This geographical difference may result in variations in the barriers identified in this research, although prior studies offer valuable clues about what might be expected. The reviewed literature consists primarily of qualitative studies conducted globally to explore the health challenges faced by TB patients. While no similar study appears to have been conducted in the Adentan municipality, these global insights confirm the challenges associated with TB care. Despite cultural and environmental differences influencing the specific challenges faced by TB patients, the findings highlight universal health barriers, offering a foundation for examining similar issues in the local context.
Adopting a quantitative descriptive cross-sectional design allowed for the systematic quantification and analysis of the health challenges experienced by TB patients in Adentan municipality. This approach provided a structured framework to identify and analyze the barriers to DOTS access, offering a localized understanding of the challenges and enabling the development of targeted interventions.
Coping Mechanisms Employed by Tuberculosis Patients Worldwide
Coping strategies refer to the specific efforts, both behavioural and psychological, that people employ to master, tolerate, reduce, or minimize stressful events about living with TB (Rajeev, et al. [24]). Positive coping strategies used by women to cope with the experiences of stigma included positive reframing, prayer, talking to other patients, focusing on schoolwork, and relaxation activities. Negative coping activities included self-imposed social isolation and anger. In some cases, non-disclosure due to stigma had an impact on TB transmission and control behaviours (Mukerji, et al. [25]). Adequate health education and counselling before commencement of treatment will help TB patients to adopt positive coping mechanisms especially when done with culturally acceptable measures. Several strategies have been adopted by TB patients to mitigate TB-related costs, and some strategies were reported as key to remaining in care. In a study conducted among TB patients, some participants shared examples of dissaving after the TB illness and taking loans. Most participants borrowed money from close people, such as family members, neighbours, and friends. A few people resorted to loan sharks or microcredit sums. Depending on the needs of the person, borrowed money ranged from $1.5 to $94. When other strategies had been exhausted, participants resorted to the sale of goods. A variety of goods were mentioned by participants; livestock and household belongings were the most frequently mentioned (Nhassengo, et al. [26]).
Also, most patients coped by selling their assets or borrowing money from family members, which often strained relationships (Hutchison, et al. [27]). No one knows when sickness will strike and what measures to take before it happens. Normally those affected do not already have enough financial resources and when they stay out of work for a short time, they run out of funds thereby worsening their situation. Patients reported using accumulated cash savings from previous years to pay for the costs associated with treatment or selling household assets such as livestock and crops. It was not atypical for a patient from a farming background to report with most of them selling livestock and farm produce to pay for treatment (Hutchison, et al. [27]). No one knows when sickness will strike and what measures to take before it happens. Normally those affected do not already have enough financial resources and when they stay out of work for a short time, they run out of funds thereby worsening their situation. Another study revealed that patients with pulmonary TB in Ghana use coping mechanisms by self-medication without going to a health facility to cope with stress. This is due to distance from health facilities, moving to different health facilities for fear of facing the social stigma that arises, and implementing spiritual coping mechanisms (Gyimah, et al. [13]). Coping strategies for management problems can reduce the pressure within and produce positive effects (Tsaur, et al. [28).
Adequate health education and counselling before commencement of treatment will help TB patients to adopt positive coping mechanisms especially when done with culturally acceptable measures. As pointed out by the patients, the diagnosis and subsequent initiation of treatment were delayed because most of them attributed their symptoms to other diseases and spent extended periods in the community on self-medications (Dodor [29]). Proper community engagement and education on TB should be done to increase people’s knowledge of tuberculosis. Several coping strategies were used to cope with TB costs. Around one-quarter of the study population used dissaving, two-thirds borrowed, and one-third sold items, (Ghazy, et al. [30]). This is a known fact of tuberculosis patients’ financial coping mechanisms. Four strategies for coping with TB stigma among TB patients were identified in a study conducted by Rahkmaawati and colleagues consisting of isolating themselves, keeping their TB status a secret, ignoring people, or trying to convince people, (Rahmawati, et al. [31]). When people keep the status of a disease to themselves, it becomes dangerous as the transmission rate increases. So proper health education is needed to change community perception about TB. Coping mechanisms are the strategies individuals use to deal with the stress and challenges associated with TB. These mechanisms can be emotional, such as seeking support from family and friends, or behavioural adjustment, such as adhering to treatment regimens (Nguyen, et al. [32]).
Understanding these mechanisms is crucial for improving patient support and outcomes. Efforts must always be made to make sure patients adopt positive coping strategies rather than negative coping strategies. Coping mechanisms for TB patients vary widely, often influenced by cultural and social contexts. Some patients rely on family support, while others turn to religious or community-based organizations (Addo, et al. [33]). Every human behaviour is influenced by culture to some extent. Negative cultural practices that affect tuberculosis control should be addressed using culturally sensitive ways through community engagements. Adaptive health behaviours, such as adhering to treatment regimens and lifestyle modifications, are also critical in managing TB (Sarpong, et al. [34). This must be encouraged at all times to ensure effective management of TB. Patients with TB often develop coping mechanisms to deal with the disease. These may include seeking social support, adhering to prescribed treatments, and, in some cases, turning to alternative therapies (Awofeso [35]). Understanding these coping mechanisms is essential for healthcare providers to offer better support to TB patients. Coping mechanisms are the strategies that TB patients use to manage the psychological and physical impacts of the disease. These may include seeking emotional support from family and friends, adhering strictly to prescribed treatment, and utilizing community resources (WHO [18]).
TB patients often develop coping strategies to manage the challenges associated with their condition. These strategies can be categorized into problem-focused coping, which involves taking active steps to manage or alter the stressor, and emotion-focused coping, which involves managing the emotional response to the stressor (Folkman, et al. [36]). In resource-limited settings, social support from family and community members plays a critical role in helping patients adhere to treatment (Kipp, et al. [37]). Additionally, some patients resort to traditional healing practices, which may or may not be complementary to conventional medical treatment (Kayombo, et al. [38]). The objective was to identify the coping mechanisms employed by TB patients in the Adentan Municipality. That was to identify the specific efforts, both behavioural and psychological, that people employ to master, tolerate, reduce, or minimize stressful events about being a patient of TB in the municipality. The global nature of the literature review above confirmed that TB patients adopted certain behaviours to deal with the effects of TB disease based on their cultural background. The literature also confirmed that some people adopted positive behaviours while others also adopted negative behaviours, and they all have an impact on the health and their TB treatment outcomes (Figure 1).
Study Design
This study adopted a quantitative descriptive cross-sectional design since survey data is collected from many individuals at a single point in time and allows the use of questionnaires with closed-ended questions.
Study Location
The study location was the Adentan Municipality in the Greater Accra Region, and it involved all treatment centers in the municipality.
Study Population
A research population is defined as “the entire group of people that a particular study is interested in”, the sample is the part or portion of the population (Divakar, et al. [39-43]). The study population refers to the entire group of individuals or entities the research intends to generalize about. It is the group from which a sample is drawn for a study, and the characteristics of this population define the scope and applicability of the research findings. These individuals have similar important experiences and characteristics to provide insightful information related to the study. The research population therefore consisted of TB patients, their relatives or treatment supporters and healthcare professionals who take care of TB patients in the Adentan municipality.
Sample Size
Sampling Method
The study participants were selected using simple random sampling. Simple random sampling is a fundamental technique in statistical sampling that ensures that every member of a population has an equal chance of being selected and helps make unbiased inferences about the population.
Tools and Methods of Data Collection
Data was collected using a structured questionnaire administered to the study participants. Data collected data was transferred into Microsoft Excel from the questionnaires.
Method of data analysis
Data collected in Microsoft Excel was later exported into SPSS Version 22.0 software for analysis. Microsoft Excel 2010 version was also used to draw charts and tables. Pearson’s chi-square test was finally used to get the required solution.
Sociodemographic Characteristics of Study Participants
Table 1 presents the sociodemographic characteristics of the study participants, which include age, religion, marital status, educational level, and occupation. Most participants were aged 25-34 years (37, 31.9%), followed by those aged 35-44 years (31, 26.7%) and 45-54 years (25, 21.6%). The lowest representation was from participants aged over 60 years (3, 2.6%). In terms of religion, most participants identified as Christians (101, 87.1%), followed by Muslims (12, 10.3%). African Traditional believers accounted for 2 participants (1.7%), while 1 participant (0.7%) adhered to another religion. Regarding marital status, the majority were married (63, 54.3%), with the remaining participants being single (53, 45.7%). For educational attainment, nearly half of the participants had secondary-level education (57, 49.1%), followed by those with tertiary education (34, 29.3%). Participants with junior high school education accounted for 16.4%, while only a few had no formal education (4, 3.4%) or primary- level education (1, 0.9%). With respect to occupation, slightly over half of the participants engaged in menial jobs (63, 54.3%), followed by those unemployed (17, 14.7%). Government workers constituted 16 participants (13.8%), while farming was the least common occupation (5, 4.3%). Coping Mechanisms adopted by people living with TB disease Table 2 presents the coping mechanisms adopted by tuberculosis (TB) patients in the Adentan municipality while managing their condition.
The table highlights how patients dealt with financial burdens, negative reactions, discrimination, and other challenges associated with TB. When asked about handling financial expenses related to their condition, 29 participants (25.0%) indicated that they relied on their savings. Similarly, 27 respondents (23.3%) reported borrowing money or receiving financial assistance from close relatives. A smaller proportion, 6 participants (5.2%), coped by selling personal goods and services, while 2 individuals (1.7%) resorted to taking loans to manage the costs of treatment. Regarding social experiences, most participants (82, 70.7%) stated that they had not encountered any form of discrimination because of their TB diagnosis. However, 31 participants (26.7%) reported experiencing various forms of discrimination, while 3 respondents (2.6%) could not recall whether they had faced any such treatment. For the 31 individuals who experienced discrimination, various coping strategies were employed. The most common approach, reported by 24 participants (20.7%), was to isolate themselves from social gatherings to avoid negative reactions. Additionally, 22 respondents (19.0%) chose to confide exclusively in health staff, ensuring that only medical professionals were aware of their condition. Meanwhile, 21 participants (18.1%) adopted self-supervision strategies to monitor their medication adherence independently. Other coping mechanisms included spiritual reliance and disengagement.
Two respondents (1.7%) stated that they turned to prayer as a way to cope with the emotional toll of discrimination, while an equal number (1.7%) said they did nothing to address the situation. These findings demonstrate the diverse ways in which TB patients in the Adentan municipality managed the physical, financial, and emotional challenges of their condition. Financial coping strategies were predominantly reliant on personal resources or social networks, reflecting the importance of family and community support. Social and emotional coping mechanisms varied widely, from self-isolation and selective disclosure to active engagement with healthcare providers. These approaches highlight the resilience and adaptability of patients in navigating the multifaceted challenges posed by TB.
This study revealed that 25.0% of respondents coped with financial expenses by using saved, 23.3% said they borrowed or received assistance from close relatives, 5.2% also said they sold personal goods and services, 1.7% of the respondents resorted to loans to help them through the journey of treatment. This work results are in line with other studies done where around one-quarter of the study population used dissaving, two-thirds borrowed, and one-third sold items, (Ghazy, et al. [30]). Several strategies have been adopted by TB patients to mitigate TB-related costs, and some strategies were reported as key to remaining in care. In a study conducted among TB patients, some participants shared examples of dissaving after the TB illness and taking loans. Most participants borrowed money from close people, such as family members, neighbours, and friends. A few people resorted to loan sharks or microcredit sums. Depending on the needs of the person, borrowed money ranged from $1.5 to $94. When other strategies had been exhausted, participants resorted to the sale of goods. A variety of goods were mentioned by participants; livestock and household belongings were the most frequently mentioned (Nhassengo, et al. [26]). Since this existing work is qualitative and did not quantify the findings, it is a little bit difficult to compare the two works. However, it confirms the fact that TB patients adopt some measures to help them financially through their treatment journey.
Also, most patients coped by selling their assets or borrowing money from family members, which often strained relationships (Hutchison, et al. [27]). Patients reported using accumulated cash savings from previous years to pay for the costs associated with treatment or selling household assets such as livestock and crops. It was not atypical for a patient from a farming background to report with most of them selling livestock and farm produce to pay for treatment (Hutchison, et al. [27]). In trying to know whether the study participants suffered any form of discrimination from other people due to their condition, most respondents (70.7%) said no, which is an indication that people in Adentan municipality have a good understanding of TB. When the 31 people who said they experienced some kind of discrimination were asked how they coped with it had most 20.7% said they isolated themselves from gatherings, 19.0% said they only spoke to the health staff about their condition as the only people who know about their condition, followed by 18.1% of respondents who said they self-supervised the uptake of their medication, and 1.7% each said they resorted to prayers and did nothing about it respectively. This is related to, four strategies for coping with TB stigma among TB patients that were identified in a study conducted by Rahkmaawati and colleagues consisting of isolating themselves, keeping their TB status a secret, ignoring people, or trying to convince people, (Rahmawati, et al. [31]).
The results also relate to positive strategies many people adopt to cope with the possibility of discrimination from other people noted in other studies. Positive coping strategies used by women to cope with the experiences of stigma included positive reframing, prayer, talking to other patients, focusing on schoolwork, and relaxation activities. Negative coping activities included self-imposed social isolation and anger. In some cases, non-disclosure due to stigma had an impact on TB transmission and control behaviors (Mukerji, et al. [25]). Another study revealed that patients with pulmonary TB in Ghana use coping mechanisms by self-medication without going to a health facility to cope with stress. This is due to distance from health facilities, moving to different health facilities for fear of facing the social stigma that arises, and implementing spiritual coping mechanisms (Gyimah, et al. [13]). Coping strategies for management problems can reduce the pressure within and produce positive effects (Tsaur, et al. [28]). Several coping strategies were used to cope with TB costs.
The study highlighted the resilience of individuals in overcoming life’s challenges, demonstrating various coping strategies adopted by respondents. Participants managed financial burdens primarily through personal savings and financial assistance from relatives. While most respondents did not experience overt discrimination, some chose to isolate themselves, relied on self-support, and limited discussions about their condition to healthcare staff. The assessment of support systems revealed a strong reliance on family support, emphasizing its crucial role in managing difficult situations. Additionally, many respondents reported receiving assistance from healthcare facilities beyond the provision of medication. This underscores the significance of a positive relationship between TB patients and healthcare staff. Finally, participants overwhelmingly agreed that the additional support from health staff had a positive impact on their recovery journey. These findings reinforce the importance of holistic care and social support systems in managing and overcoming health-related challenges.


