Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Omar Imam1*, Khaled Alzubaidi2, Hiba Ghannam3, Amina Al-Abdallah1, Simon Dobson1, Andres Perez Lopez4, Osama Samarah5, Ali Basahel5, Ali Soliman5 and Zaid Imam6
Received: January 24, 2024; Published: February 03, 2025
*Corresponding author: Omar Imam, Pediatric infectious Disease Department, Sidra Medicine, Qatar
DOI: 10.26717/BJSTR.2025.60.009455
There has been an increase in Extended Spectrum Beta Lactamase (ESBL) organisms isolated from clinical specimens during abdominal surgery. There is no data on whether this is associated with higher complication rate or the duration of hospitalization. This retrospective cohort study compared the complication rate in ESBL positive and negative patients.
Appendicitis is the most common surgical cause of abdominal pain among children presenting to the emergency room [1]. Antibiotics, together with surgery, are the standard approach for treatment of appendicitis and have even been advocated as an option even without surgical intervention [2]. There is wide variance in antibiotics chosen for treatment of appendicitis among surgeons [3]. the latest guideline published by the 2010 American Pediatric Surgical Association Outcomes and Clinical Trials Committee, recommended the use of, broad-spectrum, single or dual agent therapy [4]. Additionally, with the rise of multi-drug resistant Enterobacteriaceae including ESBL organisms, antibiotic coverage has become more challenging. The role and need for coverage of Extended spectrum beta lactamases (ESBL) bacterial growth in routine peritoneal fluid culture taken during surgery has been a subject of wide debate among both surgeons and infectious disease specialists. This has a strong impact on both empirical coverage and duration of treatment, which directly affect the cost of health care and clinical outcomes. Our study was aimed at assessing the correlation between ESBL organisms in intraoperative peritoneal fluid culture and the post-operative complication rate and evaluating the effect of different empirical antibiotics regimen on the post-surgical outcome.
Retrospective Data analysis of cases of appendicitis admitted to Sidra Medicine between 2017 and 2020 was performed. patient characteristics were documented, and analysis was performed.
Patient Characteristics
The mean age of patients was 10.4 (SD 3.3). 60.3% of patients were male. The median duration of symptoms was 1 day prior to admission. In more than 75% of cases the culture was not of use in management. The culture did not grow (49.2%), or grew normal flora and anaerobes (25.8%), thus not helping with the antibiotic decision. E.coli was the most common bacterial isolate (7.6%), followed by isolated cases of staphylococcus aureus (1.1%), pseudomonas (1.1%) and other miscellaneous organisms (Raoultella spp., Collinsella spp.). Extended Spectrum Beta lactamase (ESBL) harboring isolates grew in 49 cultures, an incidence of 12.9%. All the isolates were detected with mixed flora containing E.coli and anaerobic growth, with an overall ESBL prevalence of 38% among E.coli isolates, The rate of complications was generally low. All appendectomies were performed laparoscopically, which has been associated with lower infection rates [1]. The Surgical Site Infection (SSI) rate was 1.8%,. All the cases of SSIs occurred in the non-ESBL cases. Need for intervention rate was 2.9% and the median length of stay was 5 days (+/- 2 days). The study showed correlation between ESBL status and younger age with ESBL cases being 1 year. younger. higher CRP on admission, perforated appendix, and longer Length of stay. Univariate analysis showed correlation between symptom duration prior to admission (OR 1.94, p <0.005), ESBL status (OR 3.35, p <0.005) , and perforated appendix (OR 29.7, p< 0.005) with a length of stay greater than 5 days. There was no statistical correlation between these variables and the rate of readmission or surgical site infection. Multivariate analysis however showed no significant correlation between any of the aforementioned variables and the clinical outcomes save for the perforated status (OR 19.6, p <0.005).
ESBL organisms were first discovered in 1979. the prevalence of ESBL harboring E.coli has increased significantly from the early 2000s till now. with one meta-analysis showing an eight-fold increase [5]. The increase is higher in developing countries including Southeast asia compared to Europe [5]. The percentage of Escherichia coli isolates harboring ESBL genes in our study was 38%, which is a little higher than what was identified in other studies. 31.7% of isolates in a 2018 study of UTIs in Qatar were ESBL producers, versus 22.4% in diarrhagenic E.coli [6]. There are no high-quality trials assessing the significance of ESBL organisms in appendectomy cultures. The latest World Society of Emergency Surgery 2020 consensus statement merely mentions that empiric antibiotics used in appendicitis should be amoxicillin/clavulanate and that ertapenem should be used when ESBL organisms are suspected without strong data to support this recommendation [4]. Literature review identified no prospective trials comparing the use of ESBL directed therapy in cases of appendicitis. Only a single retrospective trial from India was identified that had 17 patients with ESBL isolates that were treated with carbapenem versus other antibiotics and showed no significant difference, however this was a retrospective trial with a low number of samples. Our center’s protocol suggests taking peritoneal cultures in all cases of appendicitis, whether simple or perforated. The results show that this practice is not cost effective or practical. 75% of isolates did not grow, grew normal flora, or mixed anaerobes which are of no consequence in management. A better approach might be to take cultures only in complicated/perforated cases. A 2010 Review also illustrated some points: simple appendectomy cases are in many times discharged before final culture results are available and the culture does not always reflect clearly the microbiologic diversity in the infected appendix [7]. Our surgical site infection rate was 1.8%, a favorable number compared to other developing nations (8.8%) [8]. The duration of symptoms prior to presentation has been related with more complications in a previous study [9]. Our study showed an aOR of 1.94 (p<0.005) of a hospital stay more than 5 days with longer symptom duration prior to admission, however this difference disappeared on multivariate analysis (Tables 1-3).
Table 1: Characteristics of Patients Admitted with Acute Appendicitis to Sidra Hospital Between 2018-2020.
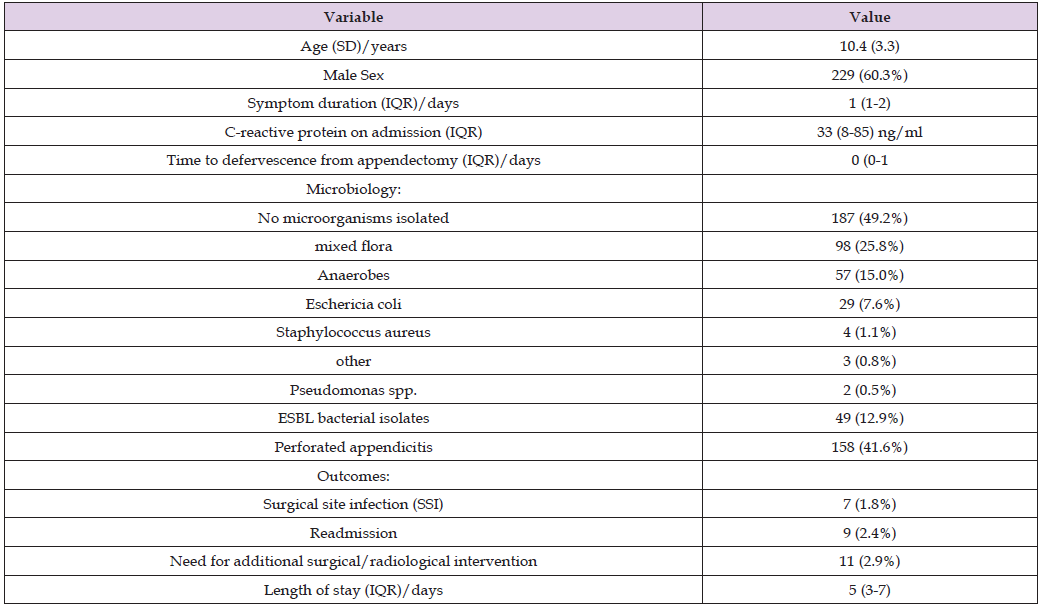
Note: SD: Standard Deviation, IQR: Interquartile Range, ESBL: Extended Spectrum Beta-Lactamase
Table 2: Comparing Characteristics of Patients With ESBL-isolates vs. Patients with no ESBL-isolates.

Note: SD: Standard Deviation, IQR: Interquartile Range, ESBL: Extended Spectrum Beta-Lactamase
Table 3: Correlates of length of stay, surgical site infections, and need for additional surgical/radiological intervention.
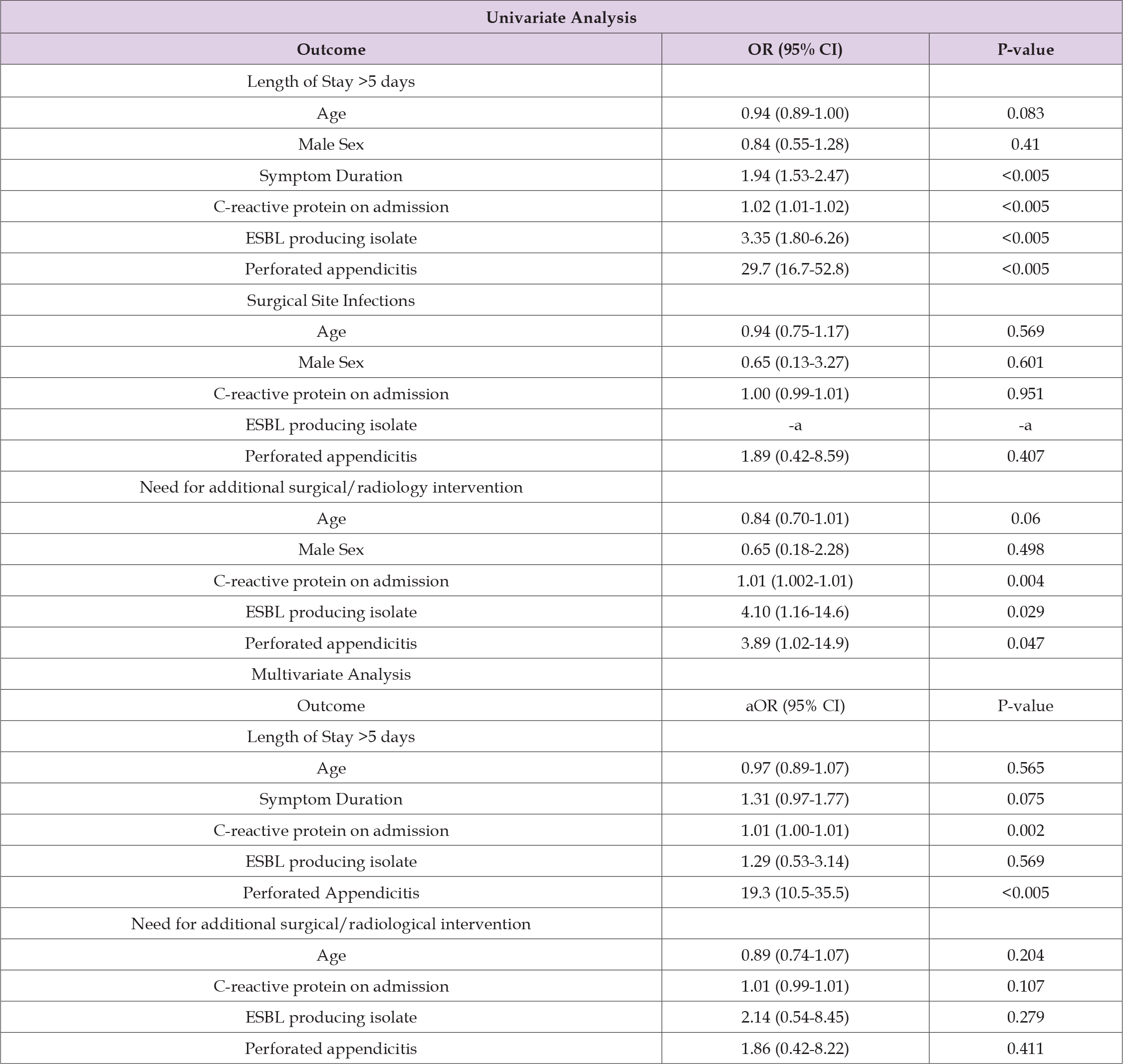
Note: OR: Odds Ratio, aOR: Adjusted Odds Ratio; ESBL: Extended Spectrum Beta-Lactamase
aComplete separation of this variable precluded ability to perform logistic regression analysis.
In summary this study shows that there is no significant difference in the complication rate between ESBL positive and ESBL negative cases. There was no significant difference in the length of stay or time to defervescence between both groups.


