Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rikhsieva Nazira Takhirovna1, Urmanova Yulduz Makhkamovna2* and Aliyeva Dinara Abralovna3
Received: November 15, 2024; Published: November 25, 2024
*Corresponding author: Urmanova Yulduz Makhkamovna, Alfraganus University, Faculty of Medicine, Department of Clinical Disciplines, (DSc) Professor, Uzbekistan
DOI: 10.26717/BJSTR.2024.59.009329
Primary hyperparathyroidism (PHPT) is the third most common endocrine disorder in developed countries, and some authors consider PHPT to be one of the most common endocrine disorders in the world. The incidence of PHPT increases with age, but can occur in patients of all ages, including children. The extent of the PHPT problem is unknown. However, in many countries, there has been an increase in the diagnosis of PTG pathology. According to medical statistics, in 30% of cases in families with primary hyperparathyroidism, the disease manifests itself in children. The diagnosis of PHPT is directly confirmed by laboratory indicators [1]. The laboratory indicators that are determined in First of all, the levels of PTH, Ca, P, and ALP in the blood are related. In the classic version of PHPT, elevated levels of PTH, Ca, ALP and a low or lower-normal level of P are determined. Screening for hypercalcemia allows to significantly increase the early detection of PHPT and the effectiveness of treatment.
Keywords: Primary Hyperparathyroidism; Children; Parathyroid Hormone; Parathyroidectomy; Hypercalcemia
To evaluate hormonal and biochemical parameters of sick children who underwent parathyroidectomy for primary hyperparathyroidism in the long-term and immediate periods.
The source of the study was 90 sick children who applied to the RSPMCE clinic in 2001-2016, who, based on the diagnosis of primary hyperparathyroidism, were treated in inpatient settings and were under outpatient observation.All patients underwent ultrasound examination of the thyroid gland, parathyroid glands, and kidneys. The level of parathyroid hormone in the blood, vitamin 25(OH)-D, total and ionized calcium, phosphorus, alkaline phosphatase, and the level of calcium and phosphorus in the urine were determined.For each child examined, a questionnaire was filled out, which recorded anamnesis data, as well as clinical, laboratory and instrumental data [2-7].
Before treatment in the main group, 49 (98%) children had hypercalcemia, 47 (94%) had hyperparathyrinemia; high levels of ionized calcium were noted in 44 (88%), alkaline phosphatase in 39 (78%). In the main group of children who underwent parathyroidectomy, one month after the operation, the blood calcium level (2.33±0.09 mmol/l; p<0.01) was significantly reduced compared to the preoperative level (2.81±0.11 mmol/l;) and was close to control in the early observation period (3-6 months) (2.32±0.08 mmol/l; 2.34±0.09 mmol/l; p<0.01).Hypercalciuria was observed in 66% of patients. The level of calcium in the urine significantly differed from the control group (2.46±0.25 mmol/day) before the operation (3.42±0.27 mmol/day), after 3 months (2.46±0.14 mmol/day after; p<0.01) they were equal to the values of the control group (Table 1). Hypophosphatemia was observed in 78% of patients. Three months after the operation, blood phosphorus (2.12±0.12 mmol/l) was reliably closer to the values of the control group (Table 2).
Note: * - significant difference compared to the control group (p<0.01).
Table 2: Dynamics of biochemical parameters in the early stages before and after surgical treatment of patients in the main group.
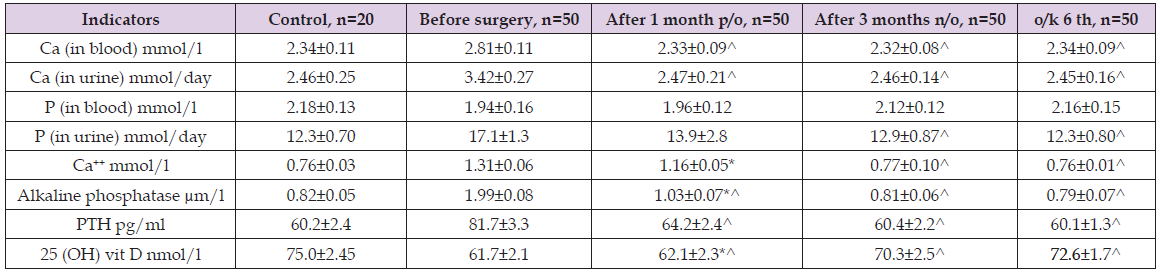
Note: * - the difference compared to the control group indicators is significant (p<0.01); ^ - the difference compared to preoperative indicators is reliable (p<0.01).
Hyperphosphaturia was observed in 76% of patients before surgery. A significant decrease in urinary phosphorus was observed 1 month after surgery (13.9±2.8 mmol/l/day), which was equal to the control values after 3 months (12.9±0.87; p<0.01). Ionized Ca++ levels were significantly higher before surgery (1.31±0.06 mmol/l) than in the control group (0.76±0.03 mmol/l). A decrease in the indicators compared to the preoperative level was recorded after 3 and (0.77±0.10 mmol/l; p<0.01;) 6 months after surgery (0.76±0.01 mmol/l; p<0.01). The parathyroid hormone level was higher before treatment (81.7±3.3 pg/ml; r<0.01) compared to the control (60.2±2.4 pg/ml), and in the immediate periods after treatment (1-3- 6 months) a decrease was observed. A trend was noted (64.2±2.4 pg/ ml; r<0.01), (60.4±2.2 pg/ml; r<0.01), (60.1±1.3 pg/ml; r<0.01). Alkaline phosphatase activity was high in 78% of patients in our study. Before surgery, its level (1.99±0.08 μm/L) was statistically significantly higher than in the control (0.82±0.05 μm/L). One month after surgery, alkaline phosphatase activity decreased (1.03±0.07 μm/L; p<0.01), and after 3 months (0.81±0.06 μm/L; p<0.01) it reached the control value. The level of 25(OH)vitamin D was lower before surgery (61.7±2.1 nmol/L) compared to the control (75.0±2.45 nmol/L) and 1-3-6 months after surgery (62.1±2.3; p<0.01); (70.3±2.5; p<0.01); (72.6±1.7; p<0.01)) increased significantly, but did not reach the control value.
In the comparison group without parathyroidectomy, during the initial examination, high blood calcium levels were noted in 39 (97.5%) patients, alkaline phosphatase in 35 (87.5%) patients, ionized calcium in 36 (90%) patients, and increased parathyroid hormone levels in 37 (92.5%) patients. Blood hypophosphatemia was registered in 33 (82.5%) and hyperphosphatemia in 34 (85%) patients. During the initial examination, the Ca level (2.90±0.03 mmol/l) was significantly higher than in the control group (2.34±0.11 mmol/l), and after 3-6 months (2.91±0.02 mmol/l, p <0.01; 2.92±0.03 mmol/l, p <0.01) a tendency to increase was noted. In this group, a high level of calcium in the urine was noted (3.41±0.12 mmol/day), and within 3-6 months (3.42±0.21 mmol/day, p <0.01; 3.44±0.26 mg/ day, p <0.01; ) a significant increase was noted (Table 1).A decrease in the blood phosphorus level was detected during the initial examination (1.88±0.07 mmol/l) and within 3-6 months (0.86±0.18 mmol/l, p<0.01; 0.85±0.06, p<0.01). A statistically significant decrease was observed [7-10].
During the initial examination, phosphorus in the urine (16.1±1.2 mmol/l) was higher than the control value (12.3±0.70 mmol/l), during the repeated examination after 1-3-6 months, its increase was observed. (16.3±1.3 mmol/l, p<0.01; 16.7±0.9 mmol/l, p<0.01; 16.8±1.1 mmol/l, p<0.01). The level of ionized Ca++ was initially elevated (1.34±0.03 mmol/l) and after 6 months increased compared to the control (1.35±0.09 mmol/l; p<0.01). The alkaline phosphatase level at the initial examination was 1.98±0.09 μm/l, after 3-6 months (2.01±0.08 μm/l, r<0.01; 2.03±0.09 μm/l, r<0.01) it was higher than the control values (0.82±0.05 μm/l). The PTH level was initially elevated (82.3±3.5 pg/ml) compared to the control value (60.2±2.4 pg/ml). After 3-6 months (82.4±3, p<0.01; 84.1±2.4 pg/ml, p<0.01; p<0.05) a statistically significant increase was revealed compared to the control. The level of 25 (OH) -D nmol/l at the initial examination was 61.4±2.0 pg/ml, and after 6 months its values significantly decreased (56.3±0.01 pg/ml; p<0.01). Thus, compared with the initial examination parameters, patients in the comparison group without PTE after 6 months had increased levels of calcium in the blood and urine, a decrease in phosphorus in the blood, as well as increased levels of alkaline phosphatase and PTH.
Long-term dynamic observations (1-5-10 years) after parathyroidectomy in children with primary hyperparathyroidism showed that the levels of calcium, phosphorus, PTH, 25(OH) and vitamin D in the blood after surgery became equal to normal values (Table 3). It was noted that in children of the comparison group with primary hyperparathyroidism, the levels of calcium, PTH, and alkaline phosphatase in the blood increased statistically significantly during long-term examination (1-5-10 years) (Table 4). In patients who underwent parathyroidectomy, preoperative hypercalcemia was 98%, and hyperparathyrinemia - 94%; high levels of ionized calcium were noted in 88%, alkaline phosphatase in 78% of patients. Parathyroidectomy led to recovery in 88% of patients. Based on reliable positive dynamics of clinical signs, positive dynamics of phosphorus-calcium metabolism was noted in 84% (3-6 months) and hormonal status in 76% (1-3 months) of cases [11,12].
Table 3: Dynamics of biochemical parameters in the early stages before and after surgical treatment of patients in the main group.
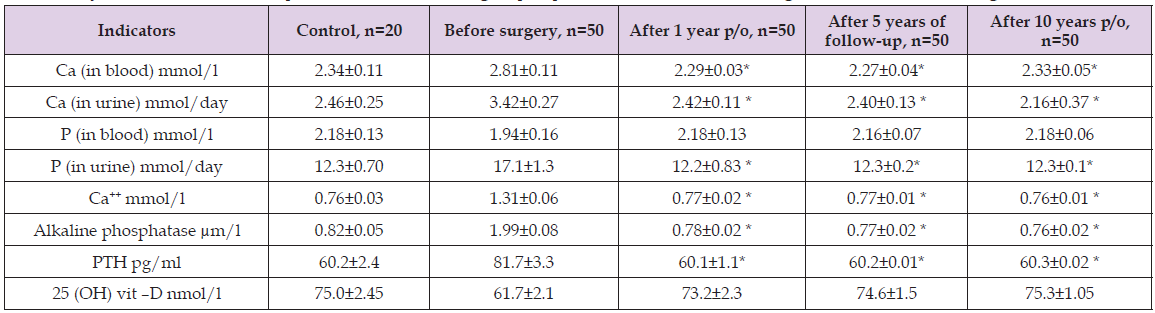
Note: * - the difference compared to preoperative values is significant (p<0.01).
Note: *-significant difference compared to the control group (p<0.001).^ - the difference compared to the indicators at the initial examination is reliable (p<0.001).
Remote observation after parathyroidectomy showed a positive effect of parathyroidectomy on Ca-F metabolism in patients of the main group. On the contrary, in patients of the comparison group who did not undergo pathogenetic therapy, the results for these parameters during the observation period were unsatisfactory. Successful surgical treatment along with normalization of the level of metabolism of the parathyroid glands led to a positive increase in the quality of life of patients.


