Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Faruk De Jesús Hernández Sampayo1* and Ismael De Jesús Yepes Barreto2
Received: November 05, 2024; Published: November 15, 2024
*Corresponding author: Faruk De Jesús Hernández Sampayo, General Surgeon Universidad Metropolitana, Residente de Gastroenterología Universidad de Cartagena, Colombia
DOI: 10.26717/BJSTR.2024.59.009306
Xanthosis cutis (xanthosis, xanthochromia, xanthoderma, carotenoderma) comes etymologically from the word ξανθος (xanthos = yellow) refers to the unspecific orange-yellowish coloration of the skin [1], it is mainly due to the elevation of carotenes in blood, which generally affects palms, soles, nasolabial and axillary folds; without involvement of sclerae, except in exceptional cases where the whole skin is affected [2]. Carotenoids are a widespread group of natural plant pigments responsible for most of the yellow, orange and red colors throughout the natural world. They are found in the plant kingdom, providing bright colors to fruits, vegetables and flowers. In leaves, they are found in chloroplasts as photosynthetic pigment-protein complexes and in mature fruits and flowers within chromoplasts. In green tissues, although the color of carotenoids is masked by the remarkably high green pigment of chlorophyll, the color appears during fruit ripening and in leaves with the onset of autumn which is associated with chlorophyll degradation [3].
Although more than 600 carotenoids have been found in nature, predominantly α-carotene, β-carotene, lutein, zeaxanthin, bcryptoxanthin, lycopene and canthaxanthin have been detected in human blood present mainly in foods such as carrot, pumpkin, orange, papaya, mango, and in general those possessing the above-mentioned colors during their life cycle (Table 1) [3]. Carotenoids are the precursors of vitamin A, the enzyme in charge of this conversion is the 15-150 -carotenoid dioxygenase. Vitamin A has many health benefits and is mainly related to vision, cell differentiation and maintenance of cell membranes, embryogenesis and immune enhancement, so the consumption of such foods rich in carotenoids is beneficial and necessary for the human body [2]. There are very few studies about this pathology, so its prevalence is uncertain, however, its presentation is rare; in a study by Priyadarshani conducted in 615 children, a prevalence of 2% was observed [4].
Hypercarotenemia is a benign condition characterized by carotenoderma caused by carotenoid deposition in the stratum corneum of the epidermis resulting in a yellowish coloration similar to jaundice of the skin [4]. It is not accompanied by any subjective symptoms; if these symptoms are present, they are due to concomitant diseases. There are three main mechanisms involved in hypercarotenemia: increased serum lipids, decreased carotenoid metabolism and excessive dietary increase, the latter undoubtedly the most frequent etiologic mechanism [5]. Carotenoids are transported in blood bound to circulating lipoproteins, so an increase in serum lipids is associated with an increase in carotenoid levels. Decreased metabolism occurs in certain pathological states, where the conversion of carotenoids to retinol is slowed, which can lead to decreased clearance and increased plasma levels such as hypothyroidism, diabetes mellitus, anorexia nervosa, nephrotic syndrome and liver disease [6].
As we said before, the main cause is the increase in intake, so we will make special emphasis on this, we could determine it by an intake higher than 20-30 mg per day during a period that will depend on the amount consumed. The average intake of adults in the USA is around 2.3 mg/day [7]. When carotenoids are ingested in excess for prolonged periods, provitamin A carotenoids are not converted to retinol, if the blood level of vitamin A is adequate. This self-limiting conversion is important in the prevention of hypervitaminosis, generating an increase in serum cartenoid concentration and leading to hypercarotemia. On the other hand, the inability to cleave provitamin A carotenoids into retinal due to genetic defects of the enzyme 15-150 -carotenoid dioxygenase can also lead to metabolic carotenemia with lower or normal intake, being extremely unusual [4].
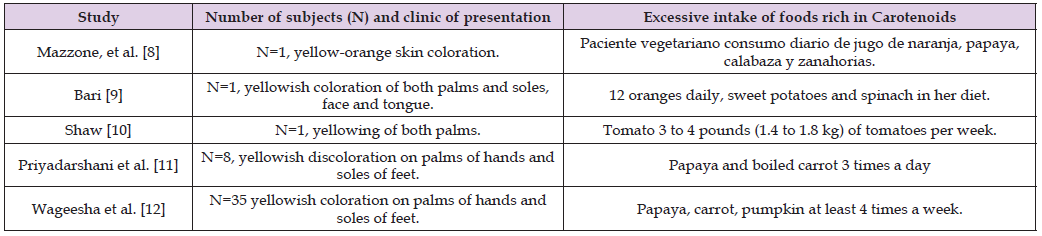
Several studies have demonstrated the causality between the consumption of foods such as carrot, papaya, orange, pumpkin and tomato with hypercarotemia, clarifying that in tomato it would be called lycopenemia, because the carotenoid that is present is lycopene (Table 2) [8-12].
Table 2: Clinical presentation, serum carotenoid/carotenoid intake associated with hypercarotenemia.
The only study conducted on the prevalence of hypercarotenemia in the western province of Sri Lanka and included 780 schools, within which it found 615 children with high carotenoid diet, of whom twelve (2%) had developed hypercarotenemia. It is noteworthy that 98% of the patients, despite having a diet high in carotenes, did not develop the disease, which allows us to speculate that there are individual genetic factors, possibly related to the level of ENZYME, which predispose to the development of the entity. The most significant differential diagnosis is with jaundice (Table 3) which is caused by bilirubins above 2.5 mg/dl [13], in rarer cases some chemicals that can cause yellow pigmentation of the skin, such as quinacrine, mepacrine, saffron, santonin, fluorescein, tetryl, dinitrophenol, canthaxanthin, picric acids and acriflavine [6].
Male patient 52 years old, with only history of cardiac revascularization surgery for ischemic heart disease, presents with 1 year of evolution characterized by yellow-orange tinge in the palms of hands, feet and face, During this time, negative serial biliopancreatic profiles were performed, fibroscan reported 6.9 kpa 2.1 iqr 30 iqr % te 10/11, ruling out hepatic fibrosis, colagioresonance reported mild splenomegaly, hiatal hernia, normal liver, esophagogastroduodenoscopy showed hiatal hernia. Taking into account the multiple negative studies, ruling out direct pathology in the biliary tract with the cholangioresonance, and fibrosis with the fibroscan, the patient was reinterrogated about his diet and stated that every day he consumed 1 kilo of papaya, and carrot several times a week to control constipation. We applied our differentiation table, where the pigmentation of our patient was self-perceived and corroborated by the examiner as yellow-orange, non-uniform, never had pruritus or bilirubin elevation in serial examinations. As for the ocular conjunctiva, it was a very curious case, since at first sight it looked yellow (Photo 1), but the tone was due to a bilateral pterygium, that when performing a correct exploration of the conjunctiva, lifting the eyelid and ordering the patient to look down (Photo 2), and retracting the lower eyelid and ordering him to look up (Photo 3), we could clarify that he had no conjunctival pigmentation, so we oriented the patient to look up (Photo 3), we could clarify that he had no conjunctival pigmentation, and we ordered him to look up (Photo 4). The realization of carotenes in blood obtaining elevation above the reference value 365. It is worth clarifying that the test was oriented, and the consumption of papaya and carrot was suspended; for administrative reasons the blood test was performed 35 days after the suspension of these foods, so we assume that they should be considerably higher if the consumption had not been suspended [14-20].


