Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Abdurehman Seid1 and Abdissa Boka2*
Received: August 06, 2024; Published: August 16, 2024
*Corresponding author: Abdissa Boka, BSc, MSc, MPH/RH, Assistant Professor, Addis Ababa University, College of Health Sciences, Ethiopia
DOI: 10.26717/BJSTR.2024.58.009129
Background: Tuberculosis continues to be one of the most important public health problems worldwide. Patient care givers (attendants) are vulnerable to Tuberculosis Infection when they give care. The problem will be very serious, if they have little Knowledge, unfavorable Attitude and poor Practice on infection prevention of Tuberculosis.
Objective: The main objective of this study is to assess knowledge, Attitude, Practice and determinant factors of infection prevention among Tuberculosis patient care givers in public hospitals, Addis Ababa, Ethiopia 2022.
Methods: An institution based cross sectional study was used. 628 Tuberculosis patient care givers who was giving care for Tuberculosis patients in selected public hospitals, included in the study. Study participants selected by simple random sampling technique. The data was entered in to and cleared using EPI -info version 7.2.1.0 and analyzed using SPSS 20 and Logistic regression used to identify factors associated with Knowledge, Attitude and practice. A Hosmers and Lemeshows rule was used to check potential confounders.
Result: 603 Tuberculosis caregivers with 96% response rate were involved in the study. Of these, 213 (35.1%) had good knowledge, 271(44.9%) positive attitude and 82 (13.6 %) good practice score towards infection prevention. Having knowledge on Infection prevention of Tuberculosis [AOR=6.50(3.35-12.23)] and Ventilated hospital [AOR = 1.81(1.26-6.55)] were significantly Associated with practice. Cough droplets [AOR=2.88(2.40-4.42)] was significantly Associated with knowledge.
Conclusion and Recommendation: Most of respondents had poor knowledge, half of respondents had unfavorable Attitude and one fourth of respondents had good practice.
Keywords: Tuberculosis; Infection Prevention; Knowledge; Attitude and Practice; Patient Care Givers
Abbreviations: AAHB: Addis Ababa Health Bureau; AFB: Acid Fast Basil; DOTS: Direct Observation Treatment; HCW: Health Care Workers; AIDS: Acquired Immune Deficiency Syndrome; DOTS: Directly Observed Treatment Short Course; ENHRL: Ethiopia Ministry of Health and National TB Reference Bureau; EPTB: Extra -Pulmonary Tuberculosis; HEWs: Health Extension Workers; HSDP: Health Sector Development Plan; IP: Infection Prevention; KAP: knowledge, Attitude, Practice; MDR: Multi Drug Resistant; PTB: Pulmonary Tuberculosis; RR: Rifampicin Resistant; TB: Tuberculosis; TBIC: Tuberculosis Infection Control; WHO: World Health Organization
Tuberculosis is a bacterial disease caused by Mycobacterium Tuberculosis; occasionally by Mycobacterium Bovis and Mycobacterium Africanum. The source of infection is a person with TB of the lung who is coughing. Coughing produces tiny infectious droplets (droplet nuclei). One cough produces 3,000 droplet nuclei. Mycobacterium Tuberculosis infects a third of the world’s population [1]. Tuberculosis remains a major global health problem [2] TB is the leading cause of mortality among infectious disease in the world [3]. World Health Organization estimated the global burden of disease caused by 2013 report 8.6 million Tuberculosis cases and 1.3 million diseases estimated in 2012 globally [4]. Worldwide Tuberculosis (TB) is one of the top ten causes of death. In 2017 there were an estimated 10.0 million new cases of TB and an estimated 1.3 million deaths among HIV negative peoples and 300,000 additional deaths from TB among HIV positives [5], as well as there were an estimated 558,000 new cases of Rifampicin –resistant TB(RR-TB) [6]. The incidence of TB Has more than double in Africa during the last decades [7]. TB is one of the major diseases that cause enormous economic crisis in low-income countries [8]. More than four million peoples suffer from active TB and 650,000 deaths occur every year in Africa and TB comprises 25% of avoidable adult death and the transmission of multi drug resistant TB(MDR-TB) among HIV infected individuals in hospitals has been documented with high case fatality rate [2].
The Tuberculosis control Program currently emphasize the Direct Observed Therapy Short Course (DOTS) strategy promote by the World Health Organization (WHO) and international union against tuberculosis and lung disease [9]. The current goals are to achieve 85% treatment success and 70% case detection among others. Tuberculosis global control currently confronts to challenge to meet those goals diagnosis delay and non -contemplation of treatment [9]. Undiagnosed and untreated person with pulmonary TB can infect an estimated 10-14 people in the year [10]. The most TB cases are in the Asia and in Africa, where higher rates of HIV and malnutrition weaken the immune system and accelerate the spread of disease (World Health Organization 2009) [9,11]. Consequently, the number of new TB cases in most African countries has more than quadrupled since 1990, with 2.8 million new cases and roughly 735 thousand deaths annually (WHO, 2005) [9]. The Sub-Saharan countries including Ethiopia are the highest TB epidemic according to WHO report. Among 30 high TB- MDR burden countries, incidence of TB -MDR in Ethiopia is ranked eight with estimated new cases are 2.7% [12]. Ethiopian ministry of health is implementing TB prevention and control program at all level of health facilities [12]. According to HSDP 2011 Report, the implementation of TB prevention and control intervention is guided by the five-year TB strategic plan, prepared in the line with the HSDP IV and the stop TB strategies. In the last 20 years much effort had been made to control and prevent TB throughout the country [9].
The recent scales up of community TB care by health extension workers ensured access of DOTS at grass root levels in the community. However, compared to the previous estimation of the TB burden for the country, the program achieved TB case detection rate less than 36% which is much lower than the minimum target (70%). The steady case detection rate raised a question whether the previous estimate was reliable or not [10]. As the TB prevalence is one of the indicators of millennium development goal (MDG) and Sustainable development goal (SDG) ending TB epidemic by 2030 is among the health target of the SDG [10]. Tuberculosis is one of the major causes of morbidity and mortality in the horn of Africa with Ethiopia caring a heavy burden. In Ethiopia TB is the major cause of death and hospital admission. Ethiopia is one of the top three in Africa and ranked 9th among the 22 countries in the world with the high burden of TB 2010 [13]. The incidence of TB in Ethiopia is 172/100,000 people and total cases notified in 2017. 117, 705 [11]. The global focus of TB control program is on early diagnosis and treatment of cases in high TB and HIV endemic areas [14]. However, the low TB detection rate and the emergence of multi drug resistant strains have been a challenge TB raising communities awareness contributes for early diagnosis of TB Which is one of the pillars of the end of TB strategy [14,15]. Studies documented shows there is a positive association between TB knowledge, Attitude, care seeking and Treatment adherence [16,17].
However, the level of knowledge should be known, also in relation to previous report before informed decision can be made when designing and implementing appropriate educational intervention [18,19]. In these regard studies conducted in general population of sub-Saharan countries documented misconception ranging from 66.3% to 99.7% of population on etiology (cause) of TB 27.6% to 90.1% on the symptoms, 0.1%-48.6% on transmission and 33.4% to 92.9% on prevention methods [18,19]. Literacy status, socio- cultural differences, gender, spatial variations have been reported to be factors affecting Knowledge, Attitude and Practice (KAP) [20]. Different studies demonstrated that limited knowledge was found to be observed among the uneducated, women, countryside residence, poor and youngsters. In addition, lower than half of the study subjects were conscious about the TB treatment and diagnosis which could act as a factor to diagnosing tuberculosis and considerably have an effect on the case notification rate [21,22]. Global experts recommended infection control (IC) is one of the key strategies for TB control and there are TB IC guidelines available even for the resource poor settings. However, its implementation seems to be inadequate in many settings. Several studies have reported poor IC measures in health facilities. TB is infectious when it occurs in the lungs or larynx until has three negative acid-fast bacilli sputum smear result after starting anti tuberculosis treatment [23]. MDR-TB is a world problem and it is more difficult and expensive to treat and cure.
There is often a delay in recognizing drug resistant TB that can lead to prolonged exposure which increases TB transmission. In addition, MDR- TB patients are remaining infectious for longer, even if treatment is initiated [24,25]. Poverty, lack of awareness, knowledge about TB causes, mode of transmission and symptoms also considered the most important factor that increases the risk of TB [13]. Factors such as infection with HIV, poor nutritional status, smoking, increased susceptibility of infants and the elderly and increased virulence and/or increased doses of bacilli have been identified as a substantial contributor for the development of the disease and its Epidemiological burden [8,26,27]. Scarcity of literature made it difficult to find research identifying Infection prevention practice and determinant factors of knowledge, attitude and practice in developing countries. So, there is a clear gap and prevalence of TB still increasing. This study was assessed knowledge, Attitude, Practice and Associated factors in infection prevention among TB Patient care givers in selected public Hospitals, Addis Ababa, Ethiopia 2019.
Study Setting and Study Period
The study was conducted in Addis Ababa the capital city of Ethiopia, covering an area of 210 km2 according to the 2007 census [28]. Addis Ababa has 10 sub cities in which the city lies an Attitude of 7,546 feet (2,300 meter) each Sub city has 10-12 Woreda and 328 Kebeles [28]. The study was done in Tuberculosis treatment hospital. There are 11 public health hospitals and around 98 health centers in the city, and in their catchment area the hospitals are either tertiary or general hospital. The study period was from April to May 2022.
Study Design: Institution based cross sectional study design was used.
Source Population: The source populations for these studies were patients’ care givers (attendants) whose age is 18 and above in selected public hospitals Addis Ababa Ethiopia.
Study Population: The study populations were tuberculosis patient care givers which are available at the time of data collection in selected hospitals and who fulfill the Inclusion criteria.
Sample Size Determination:
The required sample size was determined using single population formula for Knowledge, Attitude and Practice.
45.0% taken from a previous study from Knowledge [29].
40.80% taken from previous study for Attitude [30].
45.9% taken from a previous study for Practice [30].
Level of significance =0.05
Marginal Error (d)= 5%
n =sample size
Z(α/2) =Z-score at 95% confidence interval=1.96
Q=1-p
Non-response rate =10%
The formula for calculating (n) is
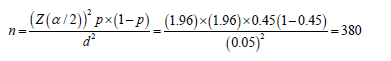
So calculated is n= 380 for Knowledge.
n= 371 for Attitude.
n=381 for Practice.
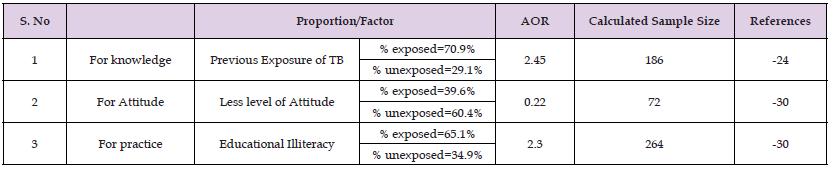
Epi- Info Version 7.2.1.0 was used to calculate the sample size for the second specific objective/independent variables using double population proportion formula with the following assumptions: power of the study=80%, 95% confidence level, and the ratio of unexposed: exposed is 1:1 (Table 1). Since all the sample sizes are too small and the largest sample size selected for this study, so the total sample size was taking design effect of 1.5 and considering 10% non-responses rate, the calculated sample size was 628.
Table 1: Sample size determination for factors associated with Knowledge, Attitude, and Practice of Infection Prevention in Tuberculosis Patient Care Givers in Selected Public Hospitals of Addis Ababa, Ethiopia 2022.
Sampling Technique
The Systemic random sampling technique was used to select study areas and by using Lottery method seven Hospitals selected which are, St Peter Hospital (SPH) it has 36 catchment area or health center and Alert Hospital (AH) also has 36 catchment area. Both Saint Peter and Alerts cover 72 health centers. The rest 26 health center catchment areas are covered by Saint Paul Hospital (SPH), Minilik Hospital (MH), Trunesh Beijing hospital (TBH), Ras Desta Hospital (RDH) and Torhailochi Hospital (TH).
Inclusion Criteria: All pulmonary TB Patient Care Givers who are available in selected hospital at a time of data collection are Included.
Data Collection Procedure: The data were collected by a structured questionnaire, which was translated into Amharic from English, and was back translate and pretest for consistency and the data collection Questionnaire was prepared in English by a researcher. The interviewee was done by trained data collector and the data collectors used data collection tool/questioner. The interviewee process was be closely monitored by investigators, the investigators also stay close with the data collectors to help when they get problem or face difficulties. Knowledge of TB patient care givers was assessed by these elements; able to recognize TB is caused by germ/bacteria, able to recognize the mode of transmission by air/through coughing droplets, able to know sign and symptoms of cough for ≥ two weeks and longer, able to recognize TB prevention method of TB.
Study Variables
Dependent Variables: Knowledge, Attitude and Practice on tuberculosis infection prevention practice in TB patient care givers.
Independent Variables: Socio- demographic characteristic of TB Patient care givers: sex, age, marital status, religion, education and income.
Institutional factor (Equipment supply and Infrastructure).
Behavioral factor (wearing mask and hand washing).
Operational Definition
Knowledge: knowledge of TB is an awareness of the TB transmission, symptoms, etiology and prevention. Knowledge was assessed by asking 17 questions, the question focuses on TB transmission, symptoms, etiology and prevention. Giving the correct answer earned 1 if not earned 0.
Excellent knowledge: if they score >80% [31].
Good Knowledge: if they score 60-79% [31].
Average Knowledge: if they score 40-59% [31].
Poor Knowledge: if they score < 40% [31].
Attitude: The study subject assumption or feeling regarding tuberculosis, TB infection prevention and control methods in decreasing TB transmission. Attitude was assessed by asking 4 questions, the question focuses on feeling regarding TB and TB infection prevention. Giving the correct answer earned 1 if not earned 0.
Positive Attitude: Tuberculosis patient care givers that was answer the four-question categorized as good attitude.
Negative Attitude: Tuberculosis patient care givers that was miss one or more question categorized as unfavorable attitude.
Practice: Focuses on Tuberculosis patient care givers general characteristics or behavior to control or prevent Tuberculosis infection. Practice was assessed by asking 4 questions and 2 observations. Giving the correct answer earned 1 if not 0.
Good Practice: Tuberculosis patients, care givers who practice all the listed five questions perfectly.
Poor Practice: Tuberculosis patient care givers that was not answer one question perfectly.
Data Management
The overall data management activity was controlled and monitored by the principal investigator of the study. All data collection forms were checked, examined for completeness and consistency during data management, storage and analysis. Then the data was be entered in to SPSS and further was checked and cleaned by principal investigator before analysis. The collected data was categorized, merged or adjusted as appropriate to the statistical model.
Data Quality Control
Two days training was given for data collectors with in an academic background of BSc degree in nursing and one coordinator working outside the study hospital and principal investigator in each hospital concerning the data collection tool and data collection process before the actual data collection period. Data quality was assured by designing a proper data abstraction tool. Pretest was done on 5% of the sample size outside the study area before the actual data collection period with a structured checklist and interview was done to check the question. It was internally consistent and checked reliability by cronsbachs alpha coefficient (P=0.82).
Data Analysis
Collected data was entered into and cleared using Epi- info version 7.2.1.0 and was analysis by SPSS Version 20 statistical software that is used for all statistical analysis in these studies. And before starting analysis, recording was done on some variables before starting the analysis. Frequencies and percentage were done for categorical variables and to measure central tendencies and variation was done to describe the study population in relation to infection prevention, control practice and socio-demographic and other relevant variables. Odd ratio with 95% confidence interval was competing to assess the presence and degree of association between the dependent and independent variables. Logistic regression model with p-value <0.05 were considered to be identify predictors of KAP of infection prevention practice. Significant factors were determined using crude and adjusted odds ratios with 95% confidence intervals. To assess the association between the different predictor variables with the dependent variables, first bi-variable relationships between each independent variable and outcome variables were investigated using a binary logistic regression model. Those independent variables with p-value < 0.25 at the bi-variable level were included in a multivariable logistic regression model to control potential confounding factors. After adjusting their effect on the outcome variables, those variables with a p–value < 0.05 with a 95% confidence interval were regarded as significant determinant factors. Multicollinearity among selected independent variables was checked by variance inflation factor (VIF) test done and was found (VIF=1.8) test passed. Normality of data was checked (Kolmogorov-smirnov test p=0.24) Assumption of fitness of goodness of the final model was checked by hosmers and lemeshow test and was found fit (P =0.08).
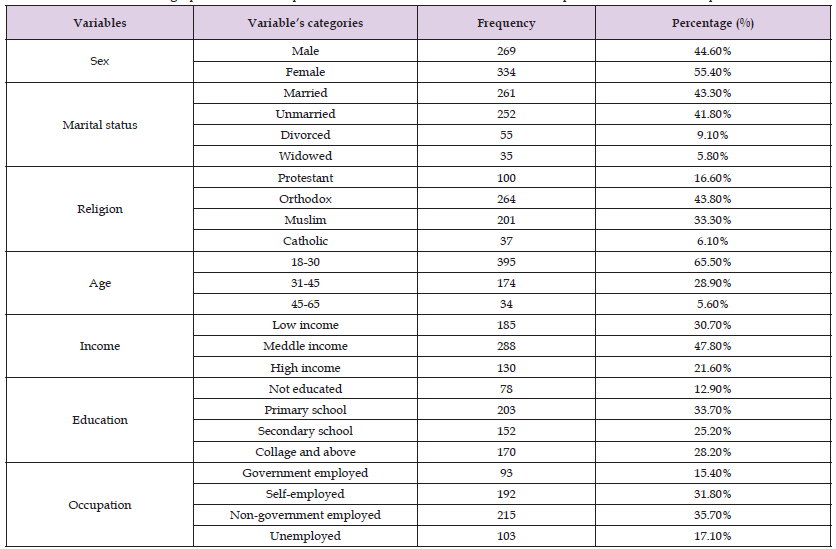
Among the total 628 care givers was expected, but 603 (96%) were the respondent’s rate. According to this study, the overall knowledge, Attitude and practice of care givers was 213(35.1%), 271(44.9%) and 82(13.6%) respectively. From total respondents, 334 (55.4%) of the study participants were females. The participant’s age was between 18-65 years with a mean age of 29 +8.4 SD years. Majority of the respondents 395 (65.5%) were between the age of 18 to 30 years and some of them 34(5.6%) were above 45 years. Regarding marital status of participants, 261(43.4%) were married, 252(41.8%) single, 55(9.1%) divorced and 35(5.8%) widowed group. According to this study, 78 (12.9%) participants did not have formal education, 203(33.7%) received primary education, 152(25.2%) completed secondary education and 170(28.2%) had colleague and above education. From the total care givers enrolled in the study, 215(35.7%), 192 (31.8%), and 103(17.1%) were non-governmental employed, self-employed, and unemployed respectively. The 85(30.7%) respondents’ monthly income was less than 2000 ETB as shown in Table 2.
Table 2: Shows Socio-Demographic Status of Respondents on IP Practice in Selected Public Hospitals Addis Ababa, Ethiopia, 2022.
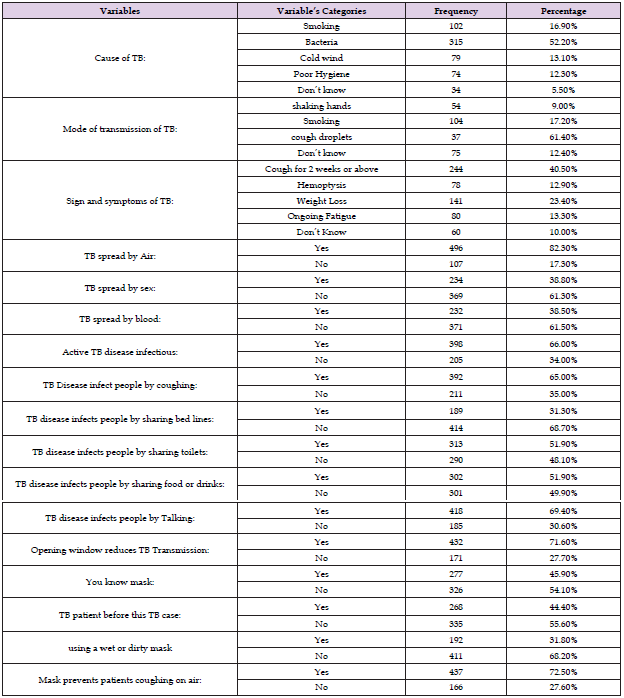
Knowledge of Study Participant Related with IP
Out of the total participants 315(52.2%) knew cause of Tuberculosis came from bacterial infection, 102(16.9%) from smoking cigarette, 79(13.1%) from cold wind, 74(12.3%) from poor personal hygiene and 34(5.5%) raised from unknown cause. Majority of the participants 370(61.4%) mode of transmission of Tuberculosis was through cough droplets and 54(9.0%) through shaking hands with infected person. From the total respondents, 244(40.5%) knew coughing for two weeks or above, 78(12.9%) hemoptysis, 141(23.4%) weight loss and 80(13.3%) had ongoing fatigue as the sign and symptoms of TB. Most of the respondents 496 (82.3%) knew that TB can spread from person to person through Air. Moreover, 234 (38.8%) participants had knowledge as TB spread from person to person through sexual contact, 232(38.5%) through blood, 392(65.0%) by coughing, 189(31.3%) by sharing bed lines, 313(51.9%) by sharing toilet, 302 (51.9%) by sharing food or drinks and 418(69.4%) by close talking. 432(71.6%) respondents had knowledge as TB transmission could be reduced by opening the window and 277 (45.9%) respondents knew what mask means. Most of participants 437(72.5%) knew Surgical Masks Keep and prevent TB patients’ caregivers from infection of TB particles or cough droplets released by TB patients in to the air. To assess knowledge of respondents 17 closed ended questions are asked only 213(35.3%) has good Knowledge as shown in Table 3.
Table 3: Frequency distribution IP on TB patient caregivers of knowledge among some of the independent variables in selected public hospitals Addis Ababa, Ethiopia, 2022.
Attitude of Study participant about IP
Attitude of respondents about infection prevention to Assess Attitude of respondent 4 closed ended question were provided over all respondents had 271(44.9%) positive Attitude. Only 146 (24.1%) females had positive Attitude, 138 (22.8%) unmarried had positive Attitude, 86(14%) who are at collage above educational level has positive attitude on infection prevention, about 198 (32.8%) Age 18-30, 165 (27.33%) TB is very serious, 101 (16.73%) had positive attitude on visit health facilities and 411(68.2%) respondent who had positive attitude revealed that isolation is necessary and 476(78.9%) respondents their choice of treatment is modern health (Figure 1).
Practice of study participant related with IP
Frequency distribution of IP practice of the study participants is described in Table 4. Overall, 13.6% of study participants have excellent practice for infection prevention where as 86.4% have poor practice (Figure 2).
Table 4: Frequency Distribution of IP Practice among Some Independent Variables in Selected Public Hospitals Addis Ababa, Ethiopia 2022.

Infection Prevention of Knowledge Practice of Study Participants
The Association between base line variables and factors of Infection prevention of Knowledge was analyzed using logistic regression model. In bi-variable logistic regression model; level of education, causes of TB, TB spreading through cough droplets, through Air, by sharing bed lines, sharing toilet, sharing food and/or drink utensils, knowing and using masks, previous history of TB patient at home, using wet or Dirty masks, surgical masks can keep TB patients from coughing TB particles in to the Air, people with active TB in the lung or throat and coughing two or more than weeks. Those variables with P-value < 0.25 in Bi-variable were included in multivariable logistic regression analysis.
Multivariable analysis of factors affecting IP knowledge of TB patient caregivers
(Table 4) In multivariable logistic regression model; level of education, TB spreading through cough droplets, knowing and using of masks and TB spreading by sharing food /or drink utensils were significantly associated with knowledge of infection prevention (< 0.05).the result of multivariable analysis revealed that the odds of respondents who had complete secondary school had 1.67 times more likely knowledgeable towards infection prevention than other group of education status [AOR=1.67(1.28-3.14)]. The odds of care givers who know TB spreading through cough droplets had 2.88 times more likely knowledgeable on infection prevention as compared to those who do not know [AOR=2.88(2.40-4.42)]. The odds of care givers who knew and used masks had 1.54 times more likely to prevent TB while they gave care for patient who were infected with Tuberculosis compared to who did not know and use mask [AOR=1.54(1.35-2.83)]. The odds of Care givers of TB patients who knew as TB can spread through shearing of food or drink utensils had 1.44 times more likely to prevent TB compared to those who did not know [AOR=1.44(1.27-2.72)] (Table 5).
Table 5: Multivariable Analysis of Factors Affecting IP Knowledge of TB Patient Care Givers in Selected Hospital Addis Ababa Ethiopia, 2022.
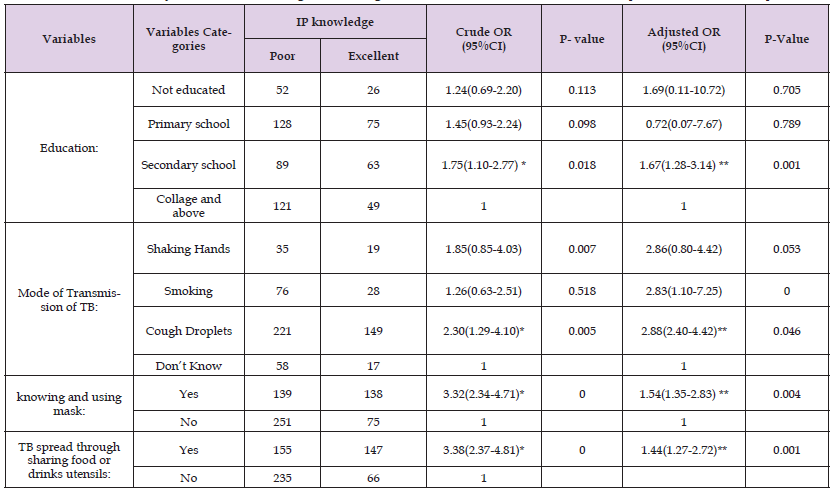
Note: * means P-value <0.25, OR; means odds ratio, **means p-value<0.05, CI; means confidence interval.
Factors Associated with Attitude on IP
The association between base line variables and factors of infection prevention attitude was analyzed using logistic regression model. In bi-variable logistic regression model; level of education, marital status, occupation, Age, treatment choice of TB, general thinking of TB (somewhat serious) and knowledge of care givers were all associated with infection prevention of practice. Those variables with P-value < 0.25 in bi-variable were included in multivariable logistic regression analysis.
Multivariable Analysis of Attitude on IP
In multivariable logistic regression model; level of education, knowledge of care givers, general thinking of Tb (somewhat serious) was significantly associated with Infection prevention Practice (< 0.05). The result of multivariable analysis revealed that the odds of the attitude of respondents who had complete secondary school were 2.57 times higher than from other groups of educational status regarding infection prevention [AOR= 2.57 (1.28-4.14)]. The odds of Care givers who had knowledge concerning infection prevention of TB had 2.70 times more likely positive attitude towards infection prevention than who did not have [AOR=2.70 (1.85-3.94)]. The odds of Respondents who had an attitude of Tuberculosis was somewhat serious had 2.11 times more likely to exposed for TB infection compared to others [AOR= 2.11(1.17-3.82)] (Table 6).
Table 6: Multivariable Analysis of Factors Affecting IP of TB Patient Care Givers Attitude in Selected Hospitals Addis Ababa Ethiopia 2022.
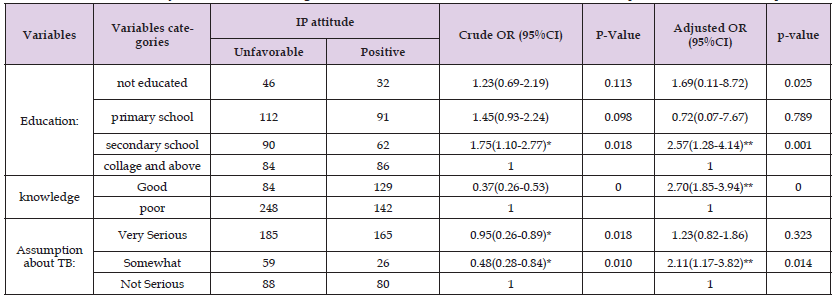
Note: * means P-value <0.25, OR; means odds ratio, **means p-value<0.05, CI; means confidence interval.
Multivariable Analyses of Factors Affecting IP Practice of TB Patient Caregivers
In multivariable logistic regression model; level of education, knowledge of caregivers, previous exposure in giving care and observing care giver open window while giving care, hand washing after giving care and ventilation of hospital wards were significantly associated with infection prevention practice (< 0.05). The result of multivariable analysis revealed that the odds of participants who had complete secondary school had 1.39 times more likely infection prevention practice as compared to other educational status [AOR= 1.39(1.13-2.65)]. The odds of respondents who had excellent knowledge concerning Infection prevention of Tuberculosis had 6.50 times more likely to practice infection prevention [AOR=6.50(3.35-12.23)]. The odds of Care givers who had previous exposure before the first TB case had 62% less likely infection prevention practice as compared to new care attendant or caregivers [AOR 0.38(0.18-0.80)]. The odds of Care givers who open window during caring had 1.37 times more likely to reduced TB spread towards them than individuals who did not open window during patient support [AOR =1.37(1.16-2.87)].the odds of Patients care givers who made hand washing after giving care had 1.47 more likely preventive IP practice than who did not wash their hand after giving care [AOR = 1.47(1.24-3.91)].the odds of Care givers who gave care at ventilated hospitals had 1.81 times more likely prevent TB transmission than not ventilated hospitals[AOR = 1.81(1.26-6.54)] (Table 7).
Table 7: Multivariable Analysis of Factors Affecting IP Practice of TB Patient Caregivers in Selected Hospitals Addis Ababa, Ethiopia 2022.

Note: * means P-value <0.25, **means p-value< 0.05, COR mean crude odds ratio, AOR means Adjusted odds ratio and CI; means confidence interval.
This study has investigated knowledge, Attitude, and practice and determinant factors of infection prevention of TB patient caregivers at public Hospitals in Addis Ababa among adult age18 and above. A total of 603 TB patient care givers were responded for TB infection prevention practice, resulting a non-respondent rate of 4%. According to this study, the overall knowledge of care givers was 213(35.1%). This may be suggestive for inadequate public health education. Tuberculosis infection control is a combination of measure aimed at minimizing the risk of Tuberculosis transmission within the population following the center for disease control and World Health Organization (WHO) guideline the Ethiopia Federal Ministry of Health has published guideline on Tuberculosis infection control Using and knowing mask is one of the recommended techniques of infection prevention to reduce the transmission of Tuberculosis [32]. this study also similar with the WHO Guideline it revealed that care givers who knew and used masks had 1.54 times more likely to prevent TB while they gave care for patient who were infected with Tuberculosis compared to who did not know. This study also showed that respondents with educational level of secondary school had 1.67 times more likely good level of overall Tuberculosis knowledge of infection prevention compared to not educated individuals because education enables care givers to gather information on Tuberculosis transmission. It is similar with a study done in Somalia [32].
The similarity is due to the same socio- economic status and same study design. Tuberculosis is caused by M. Tuberculosis. People who have Tuberculosis disease in their lung can release tiny particle M. Tuberculosis into the air by coughing these particles are called droplet nuclei. They are invisible to our naked eye. Droplet nuclei can remain airborne in room air for many hours, until they are removed by natural or mechanical ventilation [32]. This study also revealed that Tuberculosis can spread to care givers through cough droplets 3 times more likely knowledgeable towards infection prevention than to those who do not know. Regarding Attitude, this study shows 271(44.9%) respondents had positive attitude. Respondents with educational level of secondary school had increased odds of having good level of overall positive Attitude of infection prevention compared to not educated individuals. Care givers who had knowledge concerning infection prevention of TB had 2.70 times more likely positive attitude towards infection prevention than who did not have. Respondents who had an attitude of Tuberculosis was not serious had 2.6 times more likely to exposed for TB infection compared to others. The ever practice of infection prevention on this study was low because only a limited number of respondents had proper practice infection prevention on TB. The finding shows that, only 82 (13.6%) practice of Infection prevention properly. According to this study, respondents who had excellent knowledge concerning Infection prevention of Tuberculosis had 6.4 times more likely to practice infection prevention.
Patients who were identified Tuberculosis suspect or cases by screening must be separated from other patients and requested to wait in a separate well-ventilated waiting area, and provide with surgical mask to cover their mouth and noses while waiting [32]. This study also revealed that Care givers who gave care at ventilated hospitals had 1.81 times more likely prevent TB transmission since TB transmission at ventilated area is obviously reduced than crowded areas. In this study, education was one factor for practice which revealed that participants who had complete secondary school had 1.39 times more likely infection prevention practice as compared to other educational status. This study also shows those who have previous exposure of Tuberculosis Care givers who had previous exposure before the first TB case had 62% less likely infection prevention practice as compared to new care attendant or caregivers. Global strategy to prevent and control Tuberculosis transmission Tuberculosis treatment wards should be ventilated and open window to reduce Tuberculosis cough droplets on Air [32]. And The WHO policy on Tuberculosis infection control recommends not living in the same compartment with an infectious Tuberculosis patient or sharing air from a close circuit or not open window ventilation is the core method of Tuberculosis transmission prevention [32].This study also similar with this policy it revealed that on infection prevention Care givers who open window during caring had 1.37 times more likely reduced TB spread towards them than individuals who did not open window during patient support because opening window able to in and out air that prevent floating of tuberculosis cough droplets.
Principles of infection prevention and recommended practice to prevent Tuberculosis transmission: washing hands before and after any procedure for preventing cross contamination (person to person) and transmission of Tuberculosis [32]. This study also in lined with principles of infection prevention.it shows Patients care givers who made hand washing after giving care had 1.47 times more likely preventive IP practice than who did not wash their hand after giving care. As washing hands after giving care reduced Tuberculosis transmission by avoiding or reducing cough droplets.
Generally, Tuberculosis patients’ care givers who knew and use of mask, Tuberculosis spreading through cough Droplets and educational status (secondary school) were statistically significant associated factors in infection prevention knowledge of tuberculosis patients’ care givers or attendants. Tuberculosis patient’s Care givers or attendant perception towards Tuberculosis (somewhat serious), educational status (secondary school) and Knowledge of care givers concerning Tuberculosis infection prevention were statistically significant associated factors on Attitude. The results of this study revealed that significantly high proportion of Tuberculosis patient care givers had relatively poor over all knowledge, Attitude and Practice on Infection prevention of Tuberculosis. Knowledge, ventilated hospitals’ wards and hand washing after giving care were statically significant associated factors in infection prevention practice of tuberculosis patients’ care givers or attendants.
Ethical clearance was obtained from the institutional Review committee of GAMBY Medical and Business Collage. A Formal letter was submitted to Addis Ababa Health Bureau and each selected study hospital and permission was assured to keep the confidentiality. Verbal consent was asked and consent obtained from Tuberculosis patient care givers. The TB patient care givers information is strict and orientation was given to BSC nurses who collect the data of the care givers. The data collection process was held within the selected hospital and the study participants was informed before starting the interview about the whole thing the benefit and risk of participating in the study, they have the right to participate, refuse or stop even after starting or during the interview, and they have the right not to answer the question if they do not want to answer.
I would like to thank GAMBY Medical and Business College of public health for providing the opportunity to develop this thesis. Next my deepest gratitude will go to my advisor Dr. Zewdie (PhD) for his invaluable commitment, support and guidance during overall process of the research development. I also thank the study respondents at large for their wholesome effort and contribution in provision of the information. The last but not the least, I would like to thank the supervisor and data collectors for their effort to accomplish data collection.


