Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Momin Shah1*, Abdulmajeed Alharbi1, Clarissa Pena1, Ayman Salih1, Anas Alsughayer1, Abed Jabr1, Rahul Vyas2, Rohit Vyas3, Hafsa Shah5, Shahnaz Rehman1,4 and Ragheb Assaly1,4
Received: July 12, 2024; Published: July 15, 2024
*Corresponding author: Momin Shah, Department of Internal Medicine, University of Toledo, Toledo, Ohio, USA
DOI: 10.26717/BJSTR.2024.57.009028
Introduction: Takotsubo cardiomyopathy (TCM), or “broken heart syndrome,” is a distinctive form of acute
reversible heart failure triggered by stress, with recent evolving recognition of its potential morbidity and
mortality. Despite its traditional perception as benign, there is a growing need to understand its predictors and
outcomes, particularly in the context of the COVID-19 pandemic.
Methods: Utilizing the comprehensive National Inpatient Sample (NIS) for 2020, this study investigates
predictors influencing Takotsubo cardiomyopathy outcomes. The study cohort includes 33,225 hospitalizations,
with a focus on demographic factors, comorbidities, and the impact of COVID-19.
Results: Inpatient outcomes, including mortality, length of stay, and hospitalization costs, are assessed. Notably,
underweight TCM patients exhibit higher mortality risks (adjusted odds ratio: 2.48, 95% CI: 1.11 – 5.35, p-value:
0.02), while the presence of COVID-19 significantly increases mortality (adjusted odds ratio: 4.80, 95% CI: 1.86
– 12.3, p-value: 0.001), hospitalization costs (adjusted mean: $110,383, 95% CI: $8,797 – $211,968, p-value:
0.03), and duration (adjusted mean: 13.6 days vs. 8.0 days, p-value: <0.001). Gender and weight status influence
risks of acute heart failure (underweight adjusted odds ratio: 0.57, 95% CI: 0.35 – 0.91, p-value: 0.02) and atrial
fibrillation (female adjusted odds ratio: 0.56, 95% CI: 0.35 – 0.89, p-value: 0.01).
Conclusion: This extensive nationwide observational study contributes significant insights into the factors
influencing adverse outcomes among patients with Takotsubo cardiomyopathy. The findings underscore the
notable impact of COVID-19 on TCM outcomes, emphasizing the need for further research to elucidate the
complex interplay between TCM, COVID-19, and long-term patient outcomes.
Takotsubo cardiomyopathy (TCM), also known as stress-induced cardiomyopathy (SCM) or “broken heart syndrome,” is a unique and increasingly recognized form of acute reversible heart failure characterized by transient left ventricular dysfunction in the absence of significant coronary artery disease [1,2]. It is often triggered by emotional or physical stressors and predominantly affects postmenopausal women [3]. While initially considered a benign condition, growing evidence suggests that Takotsubo cardiomyopathy can lead to significant morbidity and mortality [4-6]. While most patients with Takotsubo cardiomyopathy have a favorable prognosis, a subset may experience complications such as heart failure, arrhythmias, cardiogenic shock, ventricular thrombus and even death [4,7,8]. Takotsubo cardiomyopathy, named after the ballooning of the left ventricular apex resembling a Japanese octopus pot, has traditionally been considered a relatively harmless condition [4]. However, our understanding of in-hospital and long-term outcomes remains limited despite evidence suggesting a risk of recurrence even years after the initial episode [9-12].
While the exact cause of takotsubo cardiomyopathy remains elusive, studies have explored the involvement of the brain-heart axis in its pathogenesis [13-14]. The impact of excessive catecholamine release in the development of takotsubo cardiomyopathy has been a topic of continuous discussion, prompting the consideration of beta-blockers as a potential therapeutic option [15]. As of December 2023, the COVID-19 pandemic has accounted for approximately 103 million cases and an estimated 1.1 million fatalities in the United States alone [16]. Additionally, there is a growing body of research that points to COVID-19 being associated with several cardiovascular conditions, including Takotsubo cardiomyopathy [17,18]. Our study seeks to analyze how the COVID-19 pandemic influenced outcomes among Takotsubo cardiomyopathy patients during their hospital stay. We aim to investigate whether TCM patients diagnosed with COVID-19 exhibit worse clinical outcomes when compared to those without COVID-19.
Data Source
For our study, we utilized the National Inpatient Sample (NIS) for the year 2020, a comprehensive healthcare database within the United States. The NIS is a vital component of the Healthcare Cost and Utilization Project (HCUP) database family and stands as one of the largest and most extensive repositories of its kind. It furnishes a wealth of data encompassing inpatient healthcare utilization, accessibility, cost, quality, and outcomes, both on regional and national scales. This remarkable resource incorporates information stemming from approximately 7 million annual hospital stays, which collectively represent approximately 20% of all hospitalizations throughout the United States. Notably, the NIS records feature diagnosis and procedure codes derived from the International Classification of Diseases, Tenth Revision, Clinical Modification. Since the database consists of de-identified, publicly available data, our study was deemed exempt from requiring Institutional Review Board approval.
Study Population
Within the confines of this investigation, we sought to identify individuals admitted for Takotsubo Cardiomyopathy while simultaneously evaluating the influence of specific predictors, including age, gender, race, and comorbidities. The utilization of the ICD-10- CM diagnosis code for this purpose has undergone prior validation and has been employed in various studies. Our final study cohort encompassed a total of 33,225 hospitalizations with Takotsubo Cardiomyopathy. To ensure that our findings could be extrapolated to the broader population, the sample underwent appropriate weighting procedures. Please refer to Supplementary Table 1 for a list of all ICD- 10 codes used in this study.
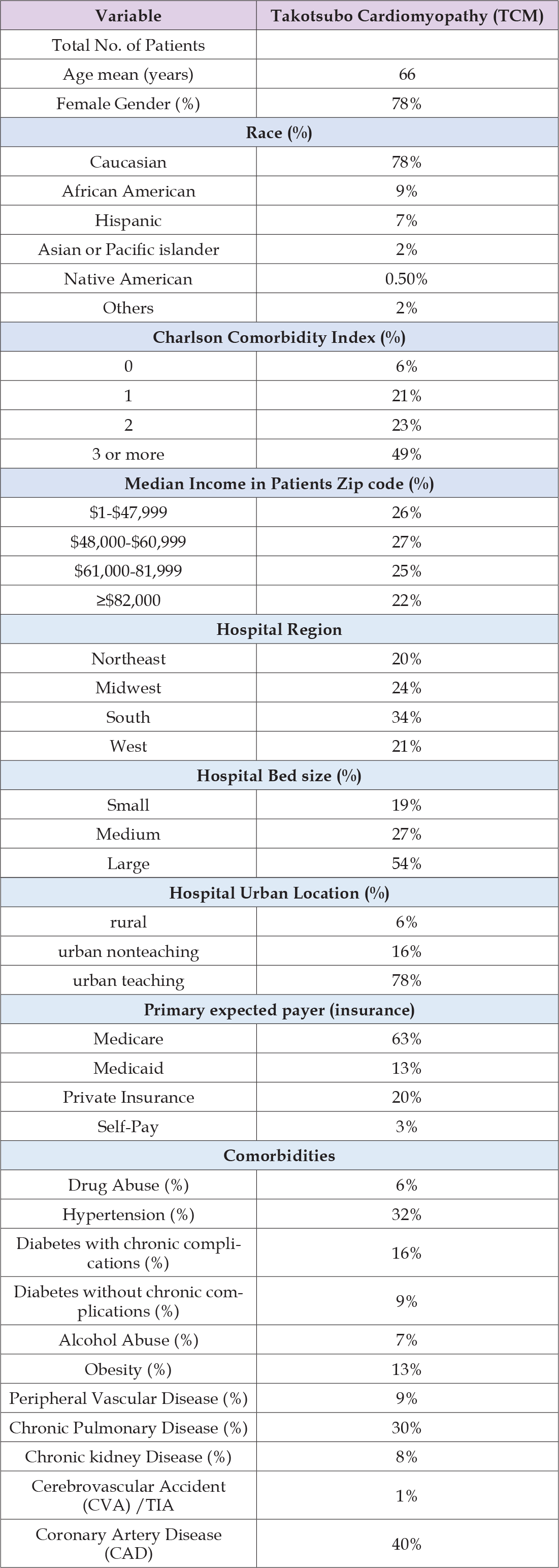
Table 1: Baseline demographic and characteristics of patients who had a diagnosis of Takotsubo cardiomyopathy (TCM)
Outcomes Measured
The primary objective of this study was to scrutinize the baseline characteristics of patients diagnosed with Takotsubo Cardiomyopathy and the impact of COVID-19 on their outcomes. Our primary endpoints of interest encompassed inpatient mortality, length of hospital stay, and hospitalization costs. Furthermore, we examined secondary endpoints, which included acute kidney injury (AKI), post-procedural bleeding, atrial fibrillation/flutter, pericardial effusion, and acute heart failure. We adjusted for potential confounders, including age, sex, Charlson Comorbidity Index (CCI), hospital bed size, hospital teaching status, primary expected payer, and hospital location.
Statistical Analysis
The study data underwent analysis using STATA version 17.0 software [10]. For categorical variables, we utilized the Rao-Scott chisquare test, tailor-made for the intricacies of survey data. This test factors in sampling weights, primary sampling units, and strata, ensuring precise estimations of population proportions and identification of statistically significant associations. In the case of continuous variables, such as means with standard errors, we employed linear regression. To unravel the relationship between Takotsubo Cardiomyopathy and both primary and secondary outcomes, we employed complex samples multivariable logistic and linear regression models. These models were thoughtfully adjusted for age, gender, admission status, as well as all baseline comorbidities and hospital characteristics, listed in Table 1. Univariate regression analysis was used to calculate unadjusted odds ratios for the study outcomes. As for adjusted odds ratios (aOR), these were computed using multivariate linear regression for continuous outcomes and logistic regression for binary outcomes. Inclusion of significant variables linked to the outcome of interest was integral to the multivariate models. To comprehensively address the complexity of the survey design, involving sampling weights, primary sampling units, and strata, our analysis incorporated svy commands. For robustness, standard errors were determined via Taylor series linearization. We considered a significance level of <0.05 as the threshold for statistical significance.
Demographic and Characteristics of Patients with Takotsubo Cardiomyopathy (TCM)
In this study, we analyzed the baseline demographic and clinical characteristics of patients diagnosed with Takotsubo cardiomyopathy (TCM). The study included a total of 33,225 patients with a mean age of 66 years. Most of the patients were female (78%), and Caucasian (78%). The Charlson comorbidity index was calculated for each patient, and a large segment of the patients had a score of 3 or more (49%). The primary expected payer was analyzed, and a significant portion of the patients had Medicare (63%). The hospital-related characteristics showed that more than half of the patients were treated in urban teaching hospitals (78%) located in the South (34%), followed by the Midwest (24%), West (21%), and Northeast (20%). Hospital bed size distribution indicated that 54% of patients received care in large hospitals, 27% in medium-sized hospitals, and 19% in small hospitals.
Inpatient Outcomes of Patients with Takotsubo Cardiomyopathy and Associated Predictors
In terms of inpatient mortality, the analysis revealed that age (adjusted odds ratio: 0.99, 95% CI: 0.98 – 1.01) and being female (adjusted odds ratio: 0.67, 95% CI: 0.40 – 1.05) did not significantly affect mortality risk, with p-values of 0.91 and 0.13, respectively. Underweight patients (BMI less than 19) (adjusted odds ratio: 2.48, 95% CI: 1.11 – 5.35, p-value: 0.02), and the presence of COVID-19 was associated with a significantly higher inpatient mortality risk (adjusted odds ratio: 4.80, 95% CI: 1.86 – 12.3, p-value: 0.001) as listed in Table 2. In terms of length of stay, both advanced age (adjusted mean: -0.14, 95% CI: -0.22 – -0.06, p-value: 0.001) and female gender (adjusted mean: -1.76, 95% CI: -3.36 – -0.16, p-value: 0.03) were associated with shorter stays. Treatment in urban teaching hospitals (adjusted mean: 2.88, 95% CI: 1.16 – 4.41, p-value: 0.001) was associated with prolonged hospital stays. The presence of COVID-19 (adjusted mean: 7.52, 95% CI: 2.47 – 12.6, p-value: 0.004) and hypothyroidism (adjusted mean: 1.51, 95% CI: 0.15 – 2.86, p-value: 0.02) were also associated with longer hospital stays. Regarding hospitalization cost, both advanced age (adjusted mean: -2332, 95% CI: -3396 – -1267, p-value: 0.001), and being female (adjusted mean: -27694, 95% CI: -52212 – -3177, p-value: 0.03) was associated with lower hospitalization costs. Treatment in urban teaching hospitals (adjusted mean: 60820, 95% CI: 41432 – 80207, p-value: 0.001) was associated with increased costs. The presence of COVID-19 also significantly increased hospitalization costs (adjusted mean: 110383, 95% CI: 8797 – 211968, p-value: 0.03).
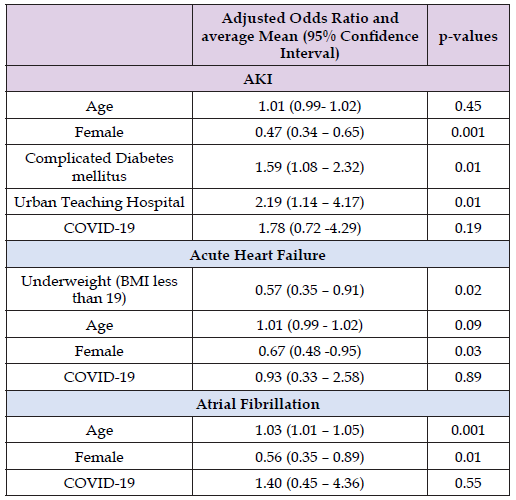
Inpatient Complications among Patients with Takotsubo Cardiomyopathy and Associated Predictors
In terms of secondary outcomes, advanced age did not significantly affect the risk for acute kidney injury (AKI) (adjusted odds ratio: 1.01, 95% CI: 0.99 – 1.02, p-value: 0.45). Female gender (adjusted odds ratio: 0.47, 95% CI: 0.34 – 0.65, p-value: 0.001) was associated with a lower risk, while complicated diabetes mellitus (adjusted odds ratio: 1.59, 95% CI: 1.08 – 2.32, p-value: 0.01) and treatment in urban teaching hospitals (adjusted odds ratio: 2.19, 95% CI: 1.14 – 4.17, p-value: 0.01) was associated with increased risk of AKI. The presence of COVID-19 did not show a significant association (adjusted odds ratio: 1.78, 95% CI: 0.72 - 4.29, p-value: 0.19). (Table 3) For acute heart failure, being underweight (BMI less than 19) was associated with a lower risk (adjusted odds ratio: 0.57, 95% CI: 0.35 – 0.91, p-value: 0.02). Age (adjusted odds ratio: 1.01, 95% CI: 0.99 – 1.02, p-value: 0.09), and the presence of COVID-19 (adjusted odds ratio: 0.93, 95% CI: 0.33 – 2.58, p-value: 0.89) did not significantly affect the risk of developing acute heart failure. For atrial fibrillation, age (adjusted odds ratio: 1.03, 95% CI: 1.01 – 1.05, p-value: 0.001) was associated with a higher risk, and being female (adjusted odds ratio: 0.56, 95% CI: 0.35 – 0.89, p-value: 0.01) was associated with a lower risk. The presence of COVID-19 did not significantly affect the risk (adjusted odds ratio: 1.40, 95% CI: 0.45 – 4.36)
Table 3: The Adjusted Odds Ratios and Average Means (95% Confidence Intervals) Along with their Respective P-Values for Inpatient Complications Among Patients with Takotsubo Cardiomyopathy and their Associated Predictors.
Impact of COVID-19 on Takotsubo Cardiomyopathy (TCM) Outcomes
We observed differences in outcomes between patients with Takotsubo cardiomyopathy (TCM) who had COVID-19 and those without COVID-19 (Table 4). Patients with TCM and COVID-19 had a notably higher total inpatient mortality rate (39% vs. 9%, p < 0.001) and increased incidence of acute kidney injury (AKI) (49% vs. 28%, p < 0.001) compared to TCM patients without COVID-19. Additionally, the prevalence of acute heart failure was significantly greater in the TCM with COVID-19 group compared to the non-COVID-19 group (39% vs. 29%, p = 0.01). There were no statistically significant differences in the rates of acute coronary syndrome (ACS), cerebrovascular accident (CVA), acute pulmonary edema, atrial fibrillation, pulmonary embolism, or elective admission between the two groups. Patients with TCM and COVID-19 experienced longer hospital stays (13.6 ± 2 days vs. 8.0 ± 1 day) and substantially higher hospitalization costs ($224,190 ± $4,000 vs. $12,700 ± $1,000) compared to those without COVID-19 (Table 4).
Table 4: Comprehensive Outcomes in Patients with Takotsubo Cardiomyopathy and the Influence of Covid-19.
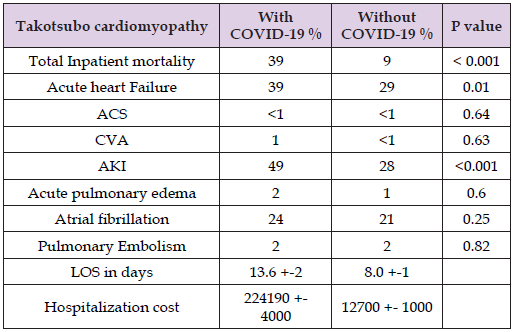
Note: Significance is denoted by P-value ≤ 0.05.
In this extensive nationwide observational study, we attempted to investigate factors that could influence outcomes among patients hospitalized with Takotsubo cardiomyopathy in the setting of the COVID-19 pandemic. Our findings reveal several significant insights. Firstly, Takotsubo cardiomyopathy patients who tested positive for COVID-19 demonstrated significantly higher mortality rates, when compared to those who did not have COVID-19. Secondly, it was observed that TCM patients with COVID-19 experienced prolonged hospitalization stays and incurred greater hospitalization costs when compared to patients without COVID-19. Thirdly, we observed an increased risk of inpatient mortality among TCM patients with a BMI of less than 19 when compared to their normal weight counterparts. Additionally, the incidence of acute heart failure and acute kidney injury was found to be higher among TCM patients with COVID-19 in comparison to those without COVID-19. Regarding the association between COVID-19 and Takotsubo syndrome, it is essential to note that Takotsubo’s mechanism is believed to be primarily influenced by physiological stressors. Some researchers have hypothesized that the increased incidence of Takotsubo syndrome during the COVID-19 pandemic may be attributed to the widespread stress experienced within the population, similar to the higher diagnosis rates observed during environmental events such as storms and earthquakes [19- 22]. Shared pathophysiological mechanisms between COVID-19 and Takotsubo syndrome, including increased sympathetic activity, microvascular dysfunction, and immune-mediated damage, may contribute to the development of both conditions [17].
Furthermore, there is mounting evidence linking COVID-19 to various cardiovascular conditions, including heart failure, myocarditis, Takotsubo syndrome, and acute coronary syndrome [18]. In our study, it remains unclear whether patients had asymptomatic COVID-19 or if COVID-19 might have triggered the inflammatory response leading to Takotsubo syndrome. This intriguing connection underscores the complexity of Takotsubo cardiomyopathy and warrants further investigation to unravel the intricate interplay between COVID-19, sympathetic activity, and patient outcomes. With regards to the observation that underweight individuals experience higher mortality rates; it is worth noting that previous research has suggested that obesity can act as a protective factor against Takotsubo cardiomyopathy. Our study’s findings align with those of an observational study conducted by (Zalewska-Adamiec, et al. [23]), which revealed that individuals with a low BMI had a striking 100% mortality rate during the 5-year follow-up period. Conversely, patients with a BMI exceeding 25 exhibited more favorable mortality outcomes, implying that obesity may indeed exert a protective effect [23,24]. (Esler, et al. [25]) attempted to shed light on the mechanism responsible for these findings. Their study elucidated that in non-obese patients, there is a notable reduction in cardiac sympathetic outflow and noradrenergic reuptake compared to obese patients. Extrapolating these findings to individuals with Takotsubo syndrome, it becomes conceivable that the heightened circulation of noradrenergic factors in obese patients may play a role in the improved outcomes observed [24,25].
Several limitations should be considered when interpreting the findings of this study. First, due to the use of a database for data collection, there is the possibility of documentation and coding errors that could have influenced the data analyzed. This potential for inaccuracies in the data may have implications for the results and conclusions drawn from this study. Second, the database does not provide longitudinal tracking of patient outcomes, which may lead to underreporting of adverse outcomes, particularly in terms of mortality. Third, the database records hospitalizations as discrete entries, without accounting for repeated hospitalizations of the same patient, which could impact the analysis of outcomes. Lastly, the study did not incorporate patient-specific data such as individual testing or imaging results that could potentially influence the measured outcomes, thus limiting the depth of the analysis. In summary, our study has highlighted important associations between COVID-19 and adverse outcomes in patients diagnosed with Takotsubo syndrome. Specifically, we found that COVID-19 infection was linked to increased mortality rates, prolonged hospitalization stays, and higher hospitalization costs among these patients. The findings underscore the need for further largescale prospective studies to assess the enduring consequences of TCM patients with COVID-19, with a particular focus on determining potential interventions to decrease morbidity and mortality. These insights can aid healthcare providers in better understanding and managing the clinical course, contributing to improved patient care and outcomes.
We employed ChatGPT to enhance grammar and writing, ensuring accuracy and clarity throughout the article. We meticulously checked for appropriateness in language usage, tone, and content to maintain a professional and scholarly demeanor throughout the article.
The authors declared no conflict of interest.
None.
All authors drafted the manuscript, critically revised the manuscript and reviewed the literature. All authors read and approved the final manuscript.
1. All authors have participated in the work and have reviewed
and agree with the content of the article.
2. None of the article contents are under consideration for
publication in any other journal or have been published in any
journal.
3. No portion of the text has been copied from other material
in the literature (unless in quotation marks, with citation).
4. I am aware that it is the author’s responsibility to obtain
permission for any figures or tables reproduced from any prior
publications, and to cover fully any costs involved. Such permission
must be obtained prior to final acceptance.
This study was deemed exempt by the Institutional Review Board of the University of Toledo, as it was a database study that included de-identified patient information.
The authors declare that all the data supporting the findings of this study are available within the manuscript.


