Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Nagaeva GA1*, Mukhamedova MG2, Li VN1, Rustamov BE1, Mukhamedov MS1, Ganiev RS1, Narziev Kh S1, Ismatov K Kh1, Saidnazarov AM1, Berdiev ZA1 and Zhuraliev M Zh1
Received: June 04, 2024; Published: July 15, 2024
*Corresponding author: Nagaeva GA, JV LLC Multidisciplinary Medical Center “Ezgu Niyat”, Uzbekistan
DOI: 10.26717/BJSTR.2024.57.009022
Purpose: To analyze the compliance (adherence) of patients in relation to various factors, as well as to study its
role in assessing the short-term and long-term (5-year) prognosis in patients with ACS.
Material and methods: This study was carried out in two stages. The retrospective part of the study included
all patients admitted to cardiology hospitals during the period from January 1, 2015 to December 31, 2015 (449
patients: 243 men and 206 women). The prospective part (5 years after ACS) included 431 surviving patients
discharged from the hospital. The assessment of the level of compliance was carried out on the basis of an
analysis of anamnestic data on medications taken, described in medical records and included a list of medications:
aspirin-containing drugs (ASA); beta-blockers (BAB); inhibitors of the renin-angiotensin-aldosterone system
(ACE inhibitors and sartans); statins; nitrates; calcium antagonists.
The average number of medications taken per day was the average value of the “individual” amount of
medications taken by the patient per day. Differences were considered statistically significant at p<0.05.
Results: In the entire sample, compliance for the main groups of drugs (ASA-containing drugs, beta blockers
and ACE inhibitors) was over 40%. Compliance was characterized by a direct correlation with age (p<0.0001),
but not with gender. Among men, the number of patients who were NOT adherent or who took ≥ 5 drugs/day.
was more than among women (p>0.05).The presence of any concomitant pathology contributed to an increase
in the level of compliance in patients with ACS.The low level of adherence to drug therapy was characterized by
an inverse correlation with the immediate (hospital) prognosis (p <0.05), in which the mortality rate was 4.0%.
In deceased women who had relatively higher compliance, the body’s endurance to acute cardiac pathology
was higher, which had a direct relationship with the period of hospital stay (p>0.05), which was slightly longer
(difference 1.9 days) than in dead men.Over the 5-year period, the mortality rate was 5.3%. Among those
who died over a 5-year period, the level of compliance was ≈ 1.5 times lower than among survivors, while in
deceased women compliance was slightly higher than in deceased men (p>0.05). Among the survivors, 64.2% of
respondents received inpatient treatment and 35.8% received only outpatient treatment, while the latter had a
comparatively higher level of compliance than those who received inpatient treatment.
Conclusion: The reviewed evidence suggests the need to introduce multifaceted, complex interventions to
increase the adherence of patients with ACS to medical recommendations and drug treatment. Increasing the
level of compliance in medical practice is an integral part of modern CVD prevention.
Keywords: Acute Coronary Syndrome; Compliance; Comorbidity; Short-Term Prognosis; Long-Term (5-Year) Prognosis
Cardiovascular diseases (CVD) remain the leading cause of morbidity and mortality in both the United States and the European continent [1]. Acute coronary syndromes (ACS), including unstable angina and acute myocardial infarction (AMI) with or without ST-segment elevation, are the main forms of acute coronary artery disease (CAD) and affect approximately 1.4 million adults annually [2]. In modern medicine, it is of great importance to analyze the behavior of a patient with an acute cardiac catastrophe, such as AMI or ACS, in relation to the prescribed therapy, when there are highly specific pharmacological drugs that cause various reactions (including unfavorable ones) of the body due to violations of their correct reception [3,4]. Patients who survive an ACS are at increased risk of developing a wide range of complications, including recurrent coronary events and death, highlighting the importance of secondary prevention measures [5]. The American College of Cardiology/American Heart Association (ACC/ AHA) guidelines currently recommend that all patients with ACS, unless otherwise contraindicated, begin taking angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs), beta blockers (BBBs).), statins and antiplatelet therapy (drugs containing acetylsalicylic acid and/or antiplatelet agents - ASA) for longterm treatment after an acute coronary event [6].
Numerous large-scale randomized clinical trials have demonstrated the effectiveness of guideline-recommended treatments in reducing the risk of recurrent ischemic events and mortality in patients who have had an ACS [7-9]. However, available data indicate suboptimal adherence of patients to medical recommendations [10]. Non-adherence to treatment is associated with an increased risk of cardiovascular mortality, hospitalization for CVD, coronary revascularization procedures and increased costs [11,12].The purpose of our study was to analyze the compliance (adherence) of patients in relation to various factors, as well as to study its role in assessing the immediate (in-hospital) and long-term (5-year) prognosis in patients with ACS.
The methodological basis of the study was the clinical database of patients diagnosed with Acute Coronary Syndrome (ACS), treated in health care facilities in one of the districts of Tashkent during the period from 01/01/2015 to 12/31/2015.During this study, a retrospective assessment of medical records was performed, followed by a prospective assessment of vital status and patient interviews 5 years after discharge from the hospital.The subjects of the study were 449 patients with ACS treated in a health care facility in one of the districts of Tashkent during the period from 01/01/2015 to 12/31/2015. Analysis of data from all patients with ACS during the study assumed compliance with the following conditions:
1. Patients must meet inclusion criteria; 2. Patient participation should not influence approaches to his therapy; 3. The inclusion of a patient in this study must be accompanied by his registration in the database with the filling out of a special “Card” for each patient individually.
In total, 449 patients with ACS were identified and hospitalized in the corresponding health care facilities in the experimental district of Tashkent. Of the entire sample of patients, 243 were male and 206 were female. The average age of the subjects was 58.40±8.12 years.
Inclusion Criteria
The study included patients aged 18 to 75 years hospitalized in appropriate hospitals for ACS.
ACS was diagnosed based on generally accepted criteria: 1. Typical pain syndrome 2. Dynamics of the ST segment and T wave on the ECG 3. Appearance of a new Q wave on the ECG 4. Dynamics of markers of myocardial damage (as tests are carried out).
Exclusion Criteria
Age under 18 and over 75 years of age. This study was carried out in two stages. The retrospective part of the study included all patients admitted to cardiology hospitals during the specified period of time - 449 patients. The prospective part included 431 patients discharged from the hospital. Below is a diagram of the study design. Through telephone interviews with the patients themselves or their relatives, outcomes 5 years after discharge from the hospital, ongoing rehabilitation, cardiovascular events, and heart surgery were determined. In case of death, the cause was determined through contact with relatives or other available documents (Table 1).
Assessment and Analysis of Patient Adherence (Compliance) to Treatment
During the study, the level of compliance or adherence of patients to treatment was assessed based on the analysis of anamnestic data on the groups of medications taken, described in the medical records. In this aspect, the following groups of drugs were analyzed:
1. Aspirin-containing drugs (ASA);
2. Beta-blockers (BBBs);
3. Inhibitors of the renin-angiotensin-aldosterone system
(ACEIs / ARBs);
4. Statins
5. Nitrates
6. Calcium Antagonists
In addition, in our work we calculated an indicator - the average number of medications taken per day, which was the average value of the “individual” amount of medications taken by the patient per day. The use of an international questionnaire scale to assess the level of compliance - the Morisky-Green scale - was not possible in our work due to the retrospective nature of the study.
Statistical Analysis of the Obtained Results
Statistical processing of the obtained data was performed on a Pentium-IV personal computer using the software package for statistical data processing Statistica 6.0. Descriptive statistics methods included assessment of the arithmetic mean (M) and standard deviation (SD).The significance of differences between the qualitative indicators of the compared groups was assessed using the χ2 test (chisquare) adjusted for Yates continuity; the critical level of significance of the null statistical hypothesis was taken equal to 0.05.Comparison between continuous values with a normal distribution was carried out using Student’s t-test.To assess the presence of connections between indicators, a correlation analysis was carried out with the calculation of the Pearson correlation coefficient.
Survival Analysis was Performed using the Kaplan–Meier Method
Univariate and multivariate analyzes of variance were performed to identify factors associated with poor outcome. One-factor analysis of variance was carried out on the basis of identifying groups of the studied characteristic according to one factor. Two-factor analysis of variance was carried out using the identification of groups of the studied characteristic according to two factors. Multivariate analysis of variance was carried out using the identification of groups of the studied characteristic according to three or more factors.Differences were considered statistically significant at p<0.05. Data are presented as M±SD.
Assessment of Adherence to Drug Therapy in Patients with ACS in Relation to Age and Gender Characteristics
From the anamnestic data, assessment of the level of compliance for the drug groups taken showed the following (Table 2). The average number of medications taken per day per patient was 2.27±1.63 units. As can be seen from Table 2, the most frequently taken groups of drugs were drugs containing ASA - 69%, BBBs - 48% and ACE inhibitors - 41%.A more detailed description of the quantitative component of drug therapy is presented in Table 2, from which it can be seen that most often patients used combinations of 3 or 4 drugs (20.7% and 18.3% of cases, respectively). Also noteworthy is the fact that ≈ 1/5 of those examined turned out to be absolutely NOT compliant with drug therapy; these patients did not take any medications at all. About 9% of those examined took 5 or more drugs per day (Table 2).When conducting a correlation analysis, it was revealed that with age, patients became more adherent to taking medications (p <0.0001), i.e. As age increased, compliance also increased (Figure 1). However, no relationship was found between gender and the level of adherence to drug therapy (p = 0.753). The average number of medications taken per day among men was 2.29±1.71 units. and among women – 2.25±1.54 units. (p=0.796). When considering men and women depending on the number of medications taken per day (Table 3), it was found that among men, those who did not take any medications at all predominated (21% vs 18%) or took 4 or more medications per day ( 29.7% vs 24.2%); all p>0.05. On the contrary, among women the number of non-adherent persons was 18%, and those taking a combination of three drugs was 23.8%, which was ≈ 1.5 (more precisely 1.3) times more than among men.
Note: ASA – acetylsalicylic acid; BBBs – beta-blockers; ACEIs – angiotensin- converting enzyme inhibitors; ARBs - angiotensin II receptor blockers; n – number of patients; 0 – did not take any drugs; 1,2,3,4 – taking 1,2,3 or 4 drugs per day; ≥ 5 – taking 5 or more drugs per day.
Note: 0 – did not take any medications; 1,2,3,4 – taking 1,2,3 or 4 drugs per day; ≥ 5 – taking 5 or more drugs per day.
The substantive aspect of conservative therapy is presented in Figure 2, from which it can be seen that both men and women had approximately the same proportions for the main groups of medications taken (all p>0.05). The difference was noted only for nitrates (p=0.225, χ2=1.471), which were taken 5.7% more often by men; calcium antagonists (p=0.041, χ2=4.178), which were used 2 times more often by women; and antiarrhythmic drugs (p=0.394, χ2=0.727), which were used 2.7% more often by men (Figure 2). A more in-depth analysis of the medications used revealed that among people taking only 1 medication, the priority drug was ASA (62%), while BBBs accounted for 12% and ACEIs accounted for 13.6% of patients. Among patients taking 2 drugs, in the greatest number of cases combinations of ASA+ BBBs were used - 37.3% and ASA+ACEi or ARBs - 33.3% of patients. Frequently used combinations of 3 drugs were ASA+BBBs+ACEIs – 46,4%; ASA+BBBs +nitrates – 16,5% и ASA+ACEIs+nitrates – 11,3% of patients.The combination of 4 drugs was presented in the largest quantity ASA+BBBs+ACEIs+nitrates – 71,4% of patients; The 5-component therapy was ASA+BBBs+ACEIs+nitrates+statins – 55,2% of patients. Thus, in the entire sample, compliance for the main groups of drugs (ASA-containing drugs, beta blockers and ACE inhibitors) was over 40%. Compliance was characterized by a direct correlation with age (p<0.0001), but not with gender. Among men, the number of patients who were NOT adherent or who took ≥ 5 drugs/day. was more than among women (p>0.05).
Assessment of Adherence to Drug Therapy in Relation to Certain Concomitant Diseases
Arterial Hypertension: In this aspect, 273 patients whose blood pressure was measured were analyzed. 2 main groups were identified: 1 gr. – 47 respondents without hypertension (control group) and 2 gr. – 226 people (with hypertension of varying severity) who, for convenience and reliability of the analysis, were divided into subgroups depending on the degree of hypertension.An assessment of therapy for patients with hypertension, regardless of its severity, showed that all patients in this category took an average of 2.4±1.6 medications/day, which turned out to be 2 times higher than in the control group (all p< 0.001). At the same time, such antihypertensive drugs as beta blockers and ACE inhibitors were used significantly more often among people with hypertension than in the control group (Table 4). Also, patients with hypertension were significantly more likely to take ASA-containing drugs. However, no relationship was found between the severity of hypertension and the quantitative component of the drug groups taken.Those. patients with ACS and concomitant hypertension, regardless of its severity, were more compliant with drug therapy than patients without hypertension.
Note: n – number of patients; AH – arterial hypertension of 1-3 degrees; BBBs – beta-blockers; ACEIs – angiotensin-converting enzyme inhibitors; ARBs - angiotensin II receptor blockers; ASA – acetylsalicylic acid; * - significance of differences in comparison with the control group at p < 0.05; ** - significance of differences compared to the control group at p<0.001.
Diabetes Mellitus: To resolve this issue, 2 groups of patients were identified: 1 gr. – 207 respondents without diabetes (control group) and 2 gr. – 159 people with diabetes. The average number of medications taken per day in patients with diabetes was 2.40±1.61 units, which is 0.16 units higher. was greater than in the comparison group (p>0.05). Despite the comparability of the compared groups in terms of medications taken (all p>0.05), patients with diabetes were still more adherent to treatment. As can be seen from Table 2, in group 2 of patients the percentages of medications taken were higher than in group 1 (Table 5). Perhaps comorbidity with such a serious pathology as diabetes encouraged patients to follow medical recommendations and take the necessary pharmacological medications, which, in turn, ensured a higher level of compliance.
Table 5: Comparative characteristics of adherence to therapy depending on the presence/absence of diabetes mellitus.
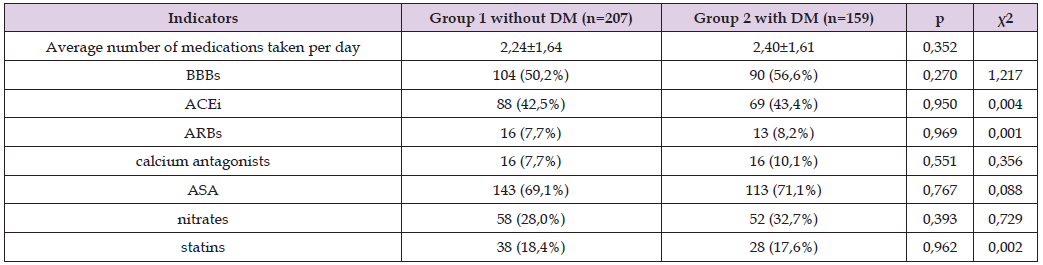
Note: n-number of patients; DM-diabetes mellitus; BBBs- beta-blockers; ACEIs-angiotensin-converting enzyme inhibitors; ARBs - angiotensin II receptor blockers; ASA – acetylsalicylic acid; * - significance of differences in comparison with the control group at p < 0.05; ** - significance of differences compared to the control group at p<0.001.
Anemia: Measurement of blood hemoglobin (Hb) levels was carried out in 362 subjects, of which 122 (33.7%) had anemia of varying severity (1 gr. - main); in 240 (66.3%) the blood Hb level was within the normative values (2 gr. – control).The average blood Hb level is 1 g. = 101.01±13.03 g/l and in 2 g. – 122.21±8.51 g/l (p<0.0001). In 1 g. presence of anemia - 1 degree. occurred in 106 (86.9% of 122 people with anemia); anemia - 2 degrees – 10 (8.2%) and anemia - 3 degrees. – in 6 (4.9%) patients. Reference blood Hb values in each of the selected subgroups were 105.14±4.43 g/l; 84.80±6.73 g/l and 55.00±13.65 g/l, respectively. A comparative analysis of anamnestic data on the drug groups taken, depending on the presence or absence of anemia, is presented in Figure 3. As is clearly presented in Figure 3, there were no significant differences in the nature of drug therapy in the analyzed groups (all p>0.05). However, it should be noted that ACS-patients with anemia took relatively more drugs containing ASA (the difference was 4.2%); BBBs (difference = 6.2%) and ACEIs (difference 7.7%). However, the average amount of medications taken per day in both groups was comparable: 1g. – 2.34±1.50 units. and in 2 g. – 2.33±1.68 units. (p>0.05). That is, patients with ACS and concomitant anemia turned out to be more adherent to taking the main groups of cardiovascular drugs (ASA, beta blockers and ACE inhibitors), although the quantitative level of compliance did not differ from that of the control group.
Chronic Kidney Disease: The CKD-EPI formula was used to determine the presence and stage of chronic kidney disease (CKD). In total, GFR calculations were performed in 82 patients (whose tests included creatinine determination). Of these, 4 people had a GFR level ≥ 90 ml/min/1.73 m2, which corresponded to CKD stage 1 (normal); in 37 patients the GFR level was 89-60 ml/min/1.73 m2 (CKD stage 2); in 30 patients, GFR = 59-30 ml/min/1.73 m2 (CKD – stage 3); in 7 respondents GFR = 29-15 ml/min/1.73 m2 (CKD stage 4) and in 3 patients GFR < 15 ml/min/1.73 m2 (CKD stage 5). As is known, stages 3-5 of CKD, in which GFR decreases <60 ml/min/1.73 m2, correspond to the definition of “chronic renal failure” (CRF).To conduct a comparative analysis, patients were divided into 2 groups: 1 g. – 41 patients with relatively preserved renal function (GFR level ≥ 60 ml/min/1.73 m2, i.e. patients with CKD stages 1-2) and 2 g. – 41 patients with impaired renal function (GFR level <60 ml/min/1.73 m2, i.e. patients with CKD stages 3-5). A comparative analysis of anamnestic data on the drug groups taken among the subjects showed (Figure 4) that drugs ASA-containing by 14.6%; BBBs – by 7.1%; ARBs – by 9.7%; statins – by 9.8% – were more often taken by patients 2 g. On the contrary, the intake of ACE inhibitors and nitrates was 4.9% and 2.5% less frequent than in the comparison group (all p>0.05). The average number of medications taken per day in 1 g. amounted to 2.39±1.84 units and in 2 g. – 2.93±1.66 units. (p>0.05). That is, patients with ACS in combination with renal dysfunction were characterized by an increased level of compliance with drug therapy, but the identified trends did not reach the level of significance (all p>0.05).Thus, this fragment of the study established that the presence of any concomitant pathology contributed to an increase in the level of compliance in patients with ACS.
Short-Term Prognosis (Hospitalization Outcome) in Patients with ACS in Relation to Compliance: Of the entire sample of patients (449 patients), death occurred in 18 (4.0%) cases during hospitalization. The average age of the deceased was 62.28±7.83 years. The male/female ratio was 10/8 (p=0.739, χ2=0.111). The average age of deceased men = 58.80±8.11 years and of deceased women – 66.62±5.04 years (p=0.030). Analysis of anamnestic data on the level of compliance among the deceased showed that the average number of medications taken per day was = 2.22 ± 1.63 units, while in men this figure was 1.90 ± 1.59 and in women – 2 .62±1.68 (p>0.05), i.e. deceased women were more adherent to therapy than deceased men. An assessment of the influence of the level of compliance on the short-term prognosis of the subjects showed that low adherence to therapy correlated with death. Namely, an inverse relationship was established between the level of compliance and the outcome of hospitalization (p<0.05), i.e. The higher the level of compliance, the greater the body’s endurance to cardiac stress, and in this situation, specifically to ACS (Figure 5). Direct analysis of the time interval from the moment of hospitalization until the death of patients (t - the period of hospital stay) found that in men this indicator was less than in women (for men t = 0.67 ± 1.0 days and for women t = 2.57±2.94 days; p=0.073). There was a direct correlation between the level of patient compliance (n=18) and the t indicator, which, however, did not reach the level of significance (p=0.772; t=0.294; r=0.078).Thus, the low level of adherence to drug therapy was characterized by an inverse correlation with the immediate (hospital) prognosis (p <0.05), in which the mortality rate was 4.0%. In deceased women who had relatively higher compliance, the body’s endurance to acute cardiac pathology was higher, which had a direct relationship with the period of hospital stay (p>0.05), which was slightly longer (difference 1.9 days) than in dead men.
5-year Prognosis of Patients with ACS from the Perspective of Assessing the Level of Compliance: This stage of the study included 431 patients (later 100%), since, as described above, 18 people died during the first hospitalization. Over the 5-year period, an additional 23 (5.3%) respondents died; It was not possible to collect information about 28 (6.5%) patients (they changed their place of residence and their contacts were lost); the remaining 380 (88.2%) people were alive. The reference values for the level of compliance among the deceased were 1.52±0.68 drugs/day. Correlation analysis established that in deceased women compliance was slightly higher than in deceased men, but the differences did not reach the level of significance (p = 0.568; t = -0.578; r = -0.125). The average number of drugs taken per day in deceased women was 1.78±0.79 units. and in deceased men – 1.36±0.65 units. (p=0.198). Figure 6 shows the Kaplan- Meier survival curves: the solid line is the group of those who died and the dotted line is the group of survivors (p<0.0001).From the telephone message, it was possible to find out that of the total number of survivors, 136 (35.8%) received outpatient treatment in family clinics at their place of residence and never (over a 5-year period) went to the hospital. In contrast, 244 (64.2%) respondents were hospitalized (sometimes more than once) in the hospital. At the same time, attention is drawn to the fact that among persons receiving outpatient treatment, the level of compliance was 0.13 units. higher (2.32±1.51 units vs. 2.19±1.68 units; p > 0.05) than in the comparison group. In addition, in general, among surviving respondents the level of compliance was 2.24 ± 1.62, which was ≈ 1.5 (more precisely 1.47) times higher than among the deceased. Among persons receiving inpatient treatment, the average number of hospitalizations over a 5-year period was 2.84±1.35 (from 1 to 10) times. Thus, over a 5-year period, the mortality rate was 5.3%. Among the deceased, the level of compliance was ≈ 1.5 times lower than among survivors, while in deceased women compliance was slightly higher than in deceased men (p>0.05). Among survivors, 64.2% of respondents received inpatient treatment and 35.8% received outpatient treatment, while the latter had a comparatively higher level of compliance than those who received inpatient treatment.
Thus, in the entire sample, compliance for the main groups of drugs (ASA-containing drugs, beta blockers and ACE inhibitors) was over 40%. Compliance was characterized by a direct correlation with age (p<0.0001), but not with gender. Among men, the number of patients who were NOT adherent or who took ≥ 5 drugs/day was more than among women (p>0.05).The presence of any concomitant pathology contributed to an increase in the level of compliance in patients with ACS.The low level of adherence to drug therapy was characterized by an inverse correlation with the immediate (hospital) prognosis (p <0.05), in which the mortality rate was 4.0%. In deceased women who had relatively higher compliance, the body’s endurance to acute cardiac pathology was higher, which had a direct relationship with the period of hospital stay (p>0.05), which was slightly longer (difference 1.9 days) than in dead men.Over the 5-year period, the mortality rate was 5.3%. Among those who died over a 5-year period, the level of compliance was ≈ 1.5 times lower than among survivors, while in deceased women compliance was slightly higher than in deceased men (p>0.05). Among survivors, 64.2% of respondents received inpatient treatment and 35.8% received only outpatient treatment, while the latter had a comparatively higher level of compliance than those who received inpatient treatment.
Compliance is adherence to treatment or the degree of correspondence between the patient’s behavior and the recommendations received from the doctor. In an extensive study, Keenan J [13] described the complex nature of commitment. There is an interaction between patient factors, disease factors, illness perceptions, influence of the prescriber and health care system, and factors related to beliefs about medications. A synonym for the concept of “compliance” is the term “commitment”. In recent years, in most scientific sources from around the world, scientists more often use the term “compliance” to denote adherence, which means the patient’s exact compliance with all medical recommendations for taking pharmacotherapy. However, according to the WHO definition, the term “compliance” includes a more complex understanding, in particular “the degree to which a patient’s behavior in relation to the use of a medicine, compliance with nutritional recommendations or lifestyle changes corresponds to the prescriptions of the attending physician” [14,15]. In addition to the basic concept of compliance, in recent years the concept of “insufficient compliance” or “NOT compliance” has appeared in scientific terminology. Unfortunately, this phenomenon turned out to be characteristic of many countries, including highly developed economic countries of the far abroad. Thus, in a meta-analysis, which included 569 studies over 50 years, a weighted average patient compliance rate was determined to be 76%, and significant variations were observed depending on the nosology and presentation of the disease [16,17]. According to many experts, patients with mental disorders often have difficulties in following doctor’s recommendations, and these patients spontaneously stop taking medications prescribed to them in an average of 50% of cases [18]. Another study found that in the primary treatment of hypertension, patients discontinued their prescribed therapy after six months in 20% of cases, and after a year in another 29% [19].
Some sources presented available data on patient adherence to secondary prevention methods after ACS. Despite advances in the treatment of CVD after ACS, which have improved outcomes in this disease [20-22], there is a gap between evidence-based recommendations and the use of secondary prevention drugs after ACS. Typically, patients are prescribed 1 or more drug groups included in the core list, and adherence data are usually divided by drug class and/ or combination of drug classes. The usual range of adherence was found to be 60% to 70% 90 days after discharge and 50% to 60% 1 year after discharge [20]. In our study, compliance for the main drug groups was over 40%. When multiple drug regimens were included in the analysis, treatment adherence was higher in patients taking ≥2 tablets compared to those taking one tablet per day [20-22]. The results of our work showed that this fact was due to the presence of comorbidity. Namely, the presence of any concomitant pathology contributed to an increase in the level of compliance in patients with ACS. When analyzing the time profile of adherence, the data showed a sustained decline in adherence beginning immediately after hospital discharge and a marked decline in compliance after 1 year [23]. Our work revealed that a decrease in the level of adherence to drug therapy inversely correlated with both the immediate (in-hospital) and long-term (5-year) prognosis in patients with ACS.
The SECURE (Secondary Prevention of Cardiovascular Disease in the Elderly) trial [24] assessed the effectiveness of a multipill strategy compared with usual care on MACE outcomes in older patients with recent AMI. The study found high levels of adherence in the polypill group compared with usual care at both 6 months (70.6% vs. 62.7%) and 24 months (74.1% vs. 63.2%). The reduction in the risk of the primary endpoint observed in the polypill group may be partly explained by increased adherence to treatment. Additionally, a systematic review of the literature [25] found that patients’ views on secondary preventive therapy and disease states may differ depending on their beliefs about medications and diseases, and that personalized interventions may be beneficial for patients after AMI. These recent additional studies reflect and highlight the complex nature of adherence during the immediate high-risk period following ACS..
The reviewed evidence indicates the need to introduce multifaceted complex interventions in order to increase the adherence of patients with ACS to medical recommendations and drug treatment, starting from the first days after discharge from the hospital and including early follow-up visits and constant attention from the medical staff of clinics and outpatient clinics, as well as the creation on their bases of special schools to train patients in the correct use of drugs, compliance with the recommended regimen and health-improving and preventive measures, which will improve the quality of life of these patients, as well as save possible financial, economic and logistical costs in the event of their relapse. Increasing the level of compliance in medical practice is an integral part of modern CVD prevention.


