Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Adrián P Hunis*
Received: July 01, 2024; Published: July 11, 2024
*Corresponding author: Adrián P Hunis, School of Medicine, Universidad de Buenos Aires, Emeritus Member of ASCO, Emeritus Member of ESMO, Honorary Member of AMA, Argentina
DOI: 10.26717/BJSTR.2024.57.009013
Artificial intelligence (AI) has made significant strides in various fields, and oncology is one of the prime beneficiaries. This article delves into how AI is revolutionizing cancer diagnosis, treatment, and patient management. By analyzing current advancements and potential future applications, we aim to provide a comprehensive overview of AI’s transformative role in oncology. Additionally, we present legal and ethical considerations relevant to the adoption of AI in clinical practice.
Cancer remains a leading cause of death worldwide, necessitating innovative approaches for early diagnosis, accurate treatment, and effective patient management. Artificial intelligence (AI), with its ability to analyze vast datasets and identify patterns, offers promising solutions in these aspects of oncology.
AI in Cancer Diagnosis
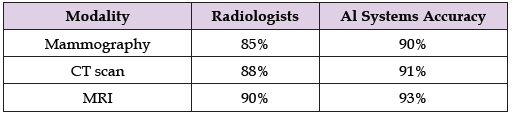
Imaging Techniques: AI algorithms, particularly deep learning, have enhanced the accuracy of imaging techniques such as MRI, CT scans, and mammograms. These improvements contribute to earlier and more accurate detection of tumors. Studies have shown that AI systems can match or even surpass the performance of human radiologists in image interpretation [1] (Table 1 & Figure 1).
Table 1: Accuracy Comparison of Radiologists vs. AI Systems in Imaging Analysis (Hypothetical Data).
Pathology: AI assists pathologists in analyzing biopsy samples with high precision, reducing human error and increasing diagnostic speed. Convolutional Neural Networks (CNNs) have been used to identify cancerous cells in histopathological images with high accuracy [2] (Figure 2). Liquid Biopsies: AI algorithms analyze circulating tumor DNA (ctDNA) from blood samples, predicting cancer mutations more efficiently than traditional biopsy methods. Liquid biopsies can provide insights into tumor dynamics and treatment response with minimal invasiveness [3].
AI in Cancer Treatment
Personalized Treatment Plans: AI systems analyze vast amounts of genetic and clinical data to recommend bespoke treatment plans for cancer patients. By integrating multi-omics data (genomic, transcriptomic, proteomic), AI can predict individual responses to therapies [3].
Case Study: Personalized Treatment for Metastatic Breast Cancer (Hypothetical Data): Two patients with metastatic breast cancer received treatment recommendations based on AI analysis of their genetic profiles. The AI-recommended treatment provided a 15% higher response rate compared to standard therapy (Figure 3). Drug Development: Machine learning models expedite drug discovery by predicting the efficacy and toxicity of new compounds. AI optimizes clinical trial designs by identifying optimal patient populations and endpoints [4] (Figure 4).
Radiation Therapy: AI optimizes radiation doses to target tumor cells while sparing healthy tissue. Dose optimization algorithms, such as those based on reinforcement learning, customize treatment plans for individual patients [5] (Table 2).
AI in Patient Management
Prognostication: AI predicts patient outcomes by analyzing historical data and current health status. Prognostic models help in identifying high-risk patients and tailoring follow-up care [5] (Figure 5).
Remote Monitoring: Wearable devices, coupled with AI, track patients’ vital signs and alert healthcare providers to any anomalies. This continuous monitoring provides real-time insights into patient health [1] (Figure 6).
Patient Adherence: AI-powered mobile apps remind patients to take medications, attend appointments, and adhere to treatment regimens. These apps can analyze patient behavior and provide personalized nudges to enhance adherence [3] (Figure 7).
Legal and Ethical Considerations
The integration of AI in oncology not only holds promising potential but also raises significant legal and ethical questions. Key considerations include accountability, patient privacy, and the regulatory landscape (Figure 8).
Accountability: When an AI system errs in diagnosis or treatment, determining liability is complex. Traditionally, physicians are responsible for patient care, but the introduction of AI complicates accountability. To address this, a clear delineation of responsibilities is necessary.
Who is Responsible?
• Physicians: They oversee AI tools and make final clinical decisions.
However, their dependency on AI advice necessitates
a deeper understanding of the system’s limitations and errors.
• AI Developers: Companies and developers who create AI
tools may bear responsibility if the error stems from the
design, coding deficiencies, or inadequate training of the AI
system.
• Healthcare Institutions: Hospitals and clinics using AI systems
should ensure proper training and integration into clinical
workflows to minimize errors.
Regulation and Standards: Establishing standardized regulations for AI in healthcare is crucial to ensure patient safety and system reliability. This involves:
• Developing Guidelines: Regulatory bodies like the FDA (Food and Drug Administration) and EMA (European Medicines Agency) must create comprehensive guidelines specifically for AI-based diagnostic and therapeutic tools.Patient Privacy and Consent: AI systems process vast amounts of sensitive patient data, raising concerns about data privacy and security. Measures to mitigate these concerns include:
• Data Encryption: Ensuring that all patient data is encrypted and stored securely.The integration of AI in oncology heralds a new era in cancer diagnosis, treatment, and patient care. While the benefits are substantial, the implementation of AI solutions must be accompanied by rigorous validation, ethical considerations, and standardized regulations to ensure efficacy and safety. Addressing legal and ethical aspects is crucial for the responsible adoption of AI in clinical practice.


