Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Gray Olvera Kevin Daniel1, Gilberto Cruz Arteaga2*, Olivia Guadalupe Villanueva Martinez2, Cristian Mercado Esquivel2, Janet Fabiola Perez Medina2, Infante Miranda Miriam Idalith2, Daniela Leticia Castañón Sánchez2, Hilda Sara Camarena Velázquez2, Alejandra Rojo Coca2, Carlos Juárez Valdés2, Mirna Edith Jimenez Nuñez2, Katya Barrera Espinoza2, Claudia Moreno Garcia2, Erandy Alejandra Lopez Toledo2, Gutierrez Cruz Raul2, Mario Alberto Huerta Manzano2, María Cristina Rodríguez Espinosa2, Wendy Yoloxochitl Castro Espinosa2, Pineda Gutierrez Monica Adriana2, Jorge Alberto Cruz Vázquez2 Molina López José Mauricio2, Arturo Andrade Sanchez3, Ismael Hernandez Javier2 and Gaspar Nava Ramirez2
Received: June 24, 2024; Published: July 03, 2024
*Corresponding author: Gilberto Cruz Arteaga, Resident physician specializing in Family Medicine, Family Medicine Unit No. 20, Calzada Vallejo 675, Col. Nueva Vallejo, CP 07750, Gustavo A Madero Delegation, Mexico
DOI: 10.26717/BJSTR.2024.57.008991
Essential systemic arterial hypertension (SAH) is a chronic-degenerative pathology with high worldwide prevalence, just as depression is one of the most frequent and disabling mood disorders. The pathophysiological mechanisms that establish a relationship between the two are not fully understood at present, which is why hypotheses have been developed, including factors such as stress and hyperactivity of the sympathetic nervous system, referring to the coexistence of both diseases simultaneously in the same patient, altering each other’s control. The objective was to associate the level of depression and the degree of essential systemic arterial hypertension in patients assigned to the Family Medicine Unit No. 20 “Vallejo”. Material and methods: An observational, analytical, prolective, cross-sectional study was carried out in 1108 beneficiaries with a diagnosis of essential SAH, blood pressure, weight and height were taken, personal data were questioned, applying Beck’s depression instrument, performing bivariate and multivariate analysis between SAH and depression and depression and demographic factors, with bivariate analysis, chi-square statistics and multivariate analysis were used, using SPSS version 26.0. Results: There was an association of grade 1 systemic arterial hypertension (BP 140-159/90-99 mmHg) in 92.2% (n=678) with minimal depression and 79.6% (n=168) with mild depression, p = 0.000, CI 95 % 0.000-0.003; In multivariate analysis, grade 1 SAH presented 6.2% risk p=0.001, women 1.7 times risk p=0.002; grade I obesity 44% risk, p=0.04; singles 68.9% risk and moderate physical activity level 70.1% risk, both with p=0.05.
Keywords: Systemic Arterial Hypertension; Depression
Systemic arterial hypertension (SAH) is a disease diagnosed with a blood pressure (BP) >140/90 mmHg, as recommended by the European Society of Hypertension (ESH) [1], classified as grade 1 (140- 159/90-99 mmHg), grade 2 (160-179/100-109 mmHg) and grade 3 (180/110 mmHg) [2], performing an average of 2 to 3 measurements on more than one occasion to classify a patient as “hypertensive” [3] . It is estimated that the global prevalence of SAH is about 1.4 billion people, approximately 31.1% of the population [4]. In Mexico, by 2022, 30 million people will have SAH, a quarter of the national population [5]. Hypertension is classified as primary and secondary. Primary or essential SAH is of multifactorial origin, caused by both predisposing and triggering factors, classified as biological and psychological [6]. Within the psychological category is the disorder of depression, which is a pathological alteration of mood with a decrease in mood in which affective, cognitive, volitional and somatic symptoms predominate [7]. For its diagnosis, the presence for 2 consecutive weeks of 5 of 9 criteria is required, part of the mentioned symptoms, according to the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) [8].
There are shared pathophysiological mechanisms between SAH and depression, such as hyperactivity of the Sympathetic Nervous System (SNS) and reduction in the activity of the Parasympathetic Nervous System (PNS) (Lechin, et. al. [9]) Another mechanism is chronic stress, which has a psychological component, which produces the release of cortisol, generating an increase in heart rate and BP [9] Finally, in 2009, García-Fabela et. to the study in the Mexican population the phenomenon of vascular depression, where microvascular lesions are generated with structural damage and cognitive effects [10] There have been various studies that in one way or another have studied the relationship between both pathologies, such as the study by García Batista, et al. [11] in the Dominican population, the presence of affective comorbidity in hypertensive patients was studied, confirming the association and predominance of somatic symptoms [11,12] did a similar study in patients in a Pakistani hospital, 39% of patients who presented hypertension also had depression, 8% were classified as mild, 14% moderate and 17% severe [12,13] described the risk factors that associated both diseases were low educational level, history of smoking, widowhood and older age [13] ; while Ashock, [14] refers to additional factors such as being a woman, low socioeconomic status, family history, uncontrolled BP, not having pharmacological treatment, and presence of comorbidities [14] Finally, Wang L, [15] described the presence of uncontrolled SAH in 1,653 patients (89.1%), with a prevalence of depression of 14.5% in uncontrolled patients and 7.4% in controlled SAH [15].
For the diagnosis of depression, there are various instruments for its evaluation, such as the Hamilton Depression Scale (HDS or HAM-D), with a Cronbach’s α of 0.789, Cohen’s κ coefficient 0.81. [16,17]; the Patient Health Questionnaire (PHQ-9) with a sensitivity of 90.4% and specificity of 81.7%, as well as a Cronbach’s α of 0.89 [18,19] ; the Composite International Diagnostic Interview (CIDI), a self-administered interview designed by the World Health Organization (WHO), with a Cohen’s κ coefficient 0.7-0.8 [20,21] ; and the Beck Depression Inventory (BDI), classifying depression with scores obtained as minimal, mild, moderate and severe, with a Cronbach’s α of 0.89, Cohen’s κ coefficient 0.31-0.61, variance of 1.58-5.00 [22] and total explained variance of 8,03-30,06% [23] and with a version translated into Spanish tested in the Mexican population, it has been shown to have an adequate internal consistency value (αs=0.87-0.92), currently being a useful tool to evaluate depression with optimal psychometric characteristics in the Mexican population [24] Therefore, the general objective is to associate the level of depression and the degree of essential systemic arterial hypertension in patients assigned to the Family Medicine Unit No. 20 “Vallejo”.
The present study is a non-experimental, transversal, observational, analytical, ambispective, prolective, and homodemic design, which had a total sample of 1,108 people. The study was carried out in the Family Medicine Unit (UMF) No. 20 “Vallejo” of the Mexican Social Security Institute (IMSS), which is a first-level medical unit providing care to the beneficiaries of the Institute. The UMF belongs to the Northwest 1 Delegation of Mexico City of the IMSS, in the period between August and December 2023.
With the acceptance of the patient’s informed consent to participate in the study and considered according to the following inclusion criteria: patients assigned to the UMF 20 “Vallejo”, patients of both sexes (man and woman), be between 18 and 65 years of age, have a history of diagnosis of essential systemic arterial hypertension; with exclusion criteria: Patients already diagnosed with a mood disorder other than depression (anxiety disorder and its variants, and bipolar disorder), patients being treated with antidepressant drugs, and pregnant patients; with elimination criteria: patients who did not completely fill out the informed consent letter, patients who did not completely respond to all the research instruments, and patients who decided to be withdrawn from the study.
The variables studied in the research are sociodemographic characteristics; age, defined as the time elapsed for a person from their date of birth to a specific point in time, obtained as years completed on an interval scale in age groups such as 18-29 years, 30-39 years, 40-49 years , or 50-65 years; sex, defined as the biological characteristics based on which people are classified as males or females of the human species at birth, obtained on a dichotomous nominal scale such as female or male; civil (marital) status, defined as the condition of a person in relation to their marriage, which is recorded in the Civil Registry, obtained on a dichotomous nominal scale such as single or married; ethylism/alcohol consumption, defined as the syndrome of dependence or addiction to ethyl alcohol, obtained with alcohol consumption obtained on a dichotomous nominal scale such as yes or no; occupation, defined as work, employment or trade, obtained on a dichotomous nominal scale as Manual if this type of activity predominates (workers, farmers, cleaning jobs, cooks, carpenters, mechanics, etc.) or as Intellectual if reasoning predominates (doctor, architect, chemist, teacher, office job, etc.); level of schooling, defined as the highest degree of study approved by the population at any of the levels of the National Educational System (SEN), obtained on an ordinal scale and indicated as None, Basic (preschool, primary or secondary), Preparatory Baccalaureate , Bachelor’s degree or engineering, or Postgraduate studies (specialty, master’s or doctorate); comorbidities, defined as the presence of two or more disorders in the same individual, obtained on a dichotomous nominal scale as yes or no; physical activity, defined as any body movement produced by skeletal muscles and resulting in energy expenditure, obtained by scoring and classification through the application of the international physical activity questionnaire in its short version (IPAQ-s) and obtained on an ordinal scale such as high physical activity level, moderate physical activity level, or low physical activity level; Body Mass Index (BMI), defined as the ratio between weight (kg) and height (m), measured with a standardized technique, being a diagnostic criterion for overweight and obesity, it is obtained by dividing the weight in kilograms by the height in meters, squared, obtained on an ordinal scale and classified as Underweight (<18.5), Normal (18.5-24.9), Overweight (25-29.9), Obesity grade I (30-34.9), Obesity grade II (35-39.9 ) or Grade III obesity (>40); Systemic arterial hypertension, obtained by measuring BP using an aneroid baumanometer and stethoscope with a standardized technique, obtained on an ordinal scale and classified as Grade 1 (BP 140-159/90-99 mmHg), Grade 2 (BP 160-179 /100-109 mmHg), or Grade 3 (BP >180/110 mmHg), as defined by the ESH1 [2]; Antihypertensive pharmacological treatment, defined as drugs that reduce blood pressure, such as ACEIs, ARBs, calcium antagonists, alpha-blockers, beta-blockers, and diuretics (furosemide, spironolactone), obtained on a nominal scale as 1 drug (single therapy), 2 medications (double therapy), 3 or more medications (triple or greater therapy), or no drug treatment; the dependent variable was depression, defined according to the DSM-58, whose classification was obtained according to the instrument applied to the Beck Depression Inventory (BDI-II) patient, obtained on an ordinal scale.
The main research instrument used was the Spanish-translated version of the BDI-II, whose original version was published in 1996 by Aaron T. Beck, it is one of the most used self-assessments of depressive symptoms, based on the diagnostic criteria of the DSM- IV, which recognizes the wide range of depressive symptoms, classifying them as somatic, affective and cognitive, corresponds to a printed instrument answered with a pen, consisting of 21 questions in the form of statements that were answered according to the patient’s feelings in the last two weeks, being answered through a Likert system, which ranges from a score of 0 to 3, adding the points and classifying them as minimal (0 to 13 points), mild (14 to 19), moderate (20 to 28) and severe (29 or more points).
The study was included in a registry approved by the health research and ethics committee.
To calculate the sample, the finite sample formula was used (n=(N*Zα2*p*q)/(e2*(N-1)+ Zα2*p*q)), where N is equal to 7,258 (hypertensive patients assigned to the UMF 20 with date of 01/25/2023 reported by the Medical Information and Medical Archive Area (ARIMAC)) , Zα2 of 2.17 (having a Confidence Level of 97%), with an estimated error of 3%, p of 50%, and q of 50%; Obtaining after the calculation an n value of 1108.42, closed to a study sample of 1108 research subjects. (book reference). The type of sampling used was probabilistic by conglomerates or clusters. To perform the descriptive univariate analysis, percentages were performed for qualitative variables (depression, essential SAH, antihypertensive pharmacological treatment, age, sex, physical activity, marital status, alcoholism, smoking, occupation, level of education, comorbidities and BMI). For the bivariate analysis, a value of p<0.05 was used as statistical significance, with a 95% confidence interval (95% CI). The IBM SPSS V.26 program was used to establish the association between variables, using Pearson’s Chi-square (x2) for qualitative variables (depression, essential SAH, antihypertensive pharmacological treatment, age, sex, physical activity, marital status, alcoholism, smoking, occupation, educational level, comorbidities and BMI). For the multivariate analysis, a main effects multimodal logistic regression model was used, taking depression and essential SAH with the significant variables obtained in the bivariate analysis for the significance model. The graphical representation of the results was carried out through data tables and bar graphs.
In the present study, 1,108 patients with a diagnosis of arterial hypertension from Family Medicine Unit Number 20 were analyzed, demographic characteristics with a significant association with depression, sex (p=0.041) was found in women with minimal depression in 54.6% (n=401), with mild depression in 64.9% (n=137); married patients (p=0.022) have more depression vs. single, with 65.3% in minimal depression (n=480), and 74.4% mild (n=157); antihypertensive pharmacological treatment (p=0.029) was 40.4% (n=297) in patients with minimal depression and 34.1% (n=72) mild depression, patients without any treatment were the most affected by this disease; 53.1% (n=390) of the sample with minimal depression and 60.2% (n=127) with mild depression, there were patients with a low level of physical activity (p=0.007); overweight patients (p=0.004) were the most affected BMI group, with 40.7% (n=299) with minimal depression and 43.1% (n=91) with mild depression. (Table 1) The association of the degree of systemic arterial hypertension with the degree of depression, a greater number of depressed patients was obtained in those with grade 1 hypertension (BP 140-159/90-99 mmHg) in 92.2% (n=678) with minimal depression and 79.6 % (n=168) mild degree, presenting a p value of 0.000 with a 95% confidence interval 0.000- 0.003 (Table 2).
Table 1: Demographic Characteristics Associated with the Degree of Depression of Patients with Systemic Arterial Hypertension at UMF No.20 “Vallejo”.
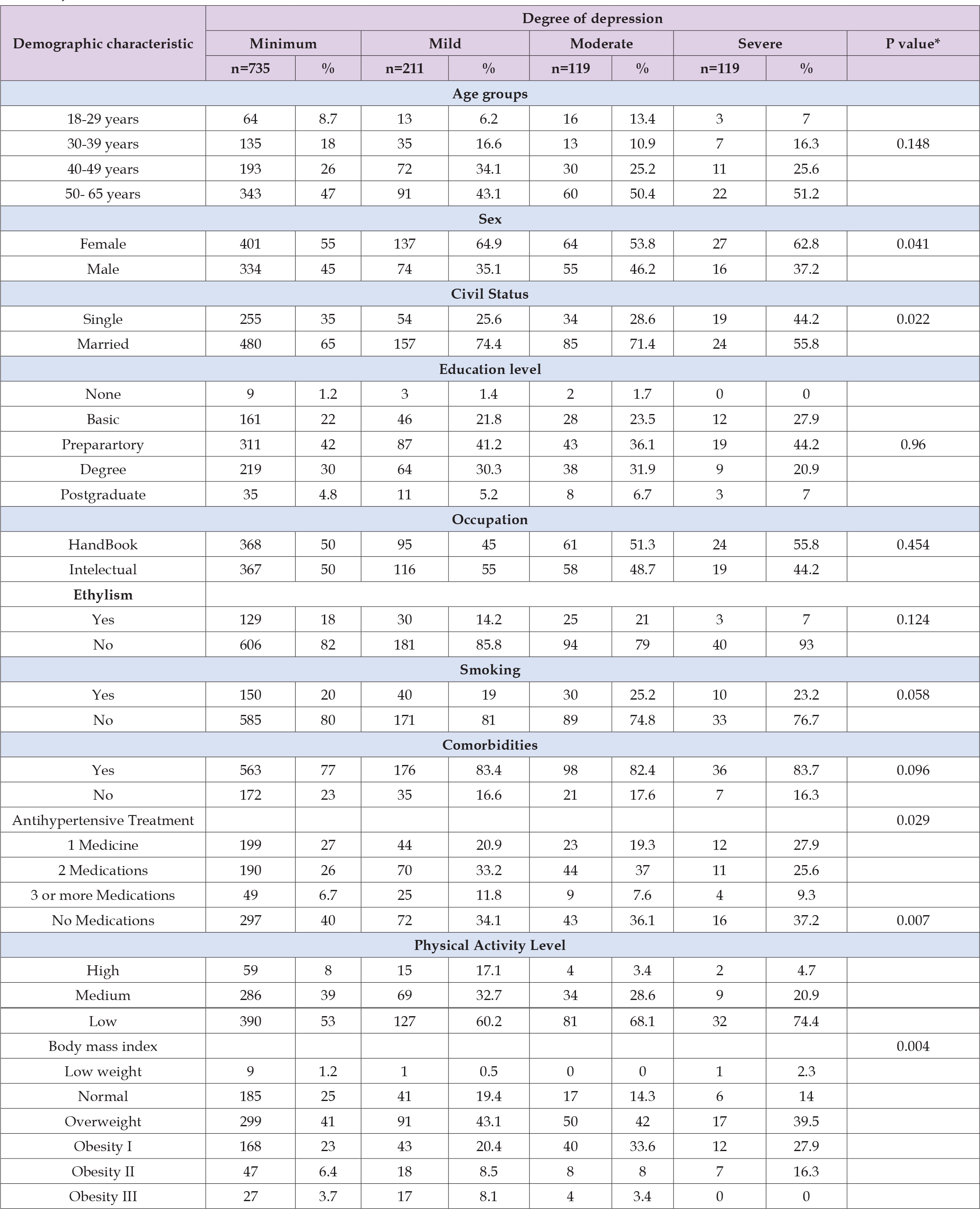
Note: * p < 0.05 Pearson’s Chi-square test.
Table 2: Association of Systemic Arterial Hypertension with Depression in patients of the UMF No. 20 “Vallejo”.
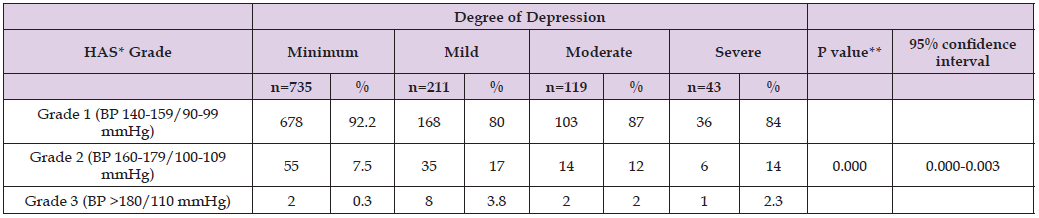
Note: * Systemic Arterial Hypertension,• p <005 Pearson’s Chi-square Test.
Significant associations of demographic characteristics with systemic arterial hypertension and depression were reported in the age group 50-65 years (p=0.005), with a predominance in grade 1, 94.2% (n=323) of patients with minimal depression and 80.2% (n=73) mild depression; in the sex characteristic, men predominated (p=0.002) with grade 1 hypertension vs. women 91% (n=304) with minimal depression and 73% (n=54) with mild; marital status, married (p=0.002) predominance in SAH grade 1, 91.9% (n=414) with minimal depression and 79.6% (n=125) with mild; patients without antihypertensive pharmacological treatment (p=0.04) with grade 1 SAH, 94.8% (n=282) of the sample with minimal depression and 93.1% (n=67) with mild; physical activity, patients with SAH grade 1 (p=0.002) with 93.3% (n=364) with minimal depression and 78.87% (n=100) with mild; In patients with BMI grade II obesity (p=0.016), 91.5% (n=43) had grade 1 SAH with the presence of minimal depression and 50% (n=9) mild depression (Table 3, Figures 1 & 2). In the multivariate analysis with a multimodal logistic regression model with parameter estimation of the association of the degree of mild depression with the degree of systemic arterial hypertension and demographic characteristics; grade 1 SAH presented a statistically significant level (p=0.001), with a 6.2% risk (B =-2.785); the age group 40-49 years did not present a statistically significant difference (p=0.077); women presented a statistically significant difference (p=0.002) with a risk 1.7 times (B = 0.533); single patients with p=0.05 and 68.9% risk (B = -0.373); antihypertensive treatment did not present a statistically significant difference (p=0.098); the moderate level of physical activity presented p=0.05, with a 70.1% risk (B = -0.356); the BMI of patients with grade I obesity presented a statistically significant difference (p=0.04) with a 44% risk (B = -0.776) (Table 4).
Table 3: Association of Demographic Characteristics with Systemetic Arterial Hypertension and Depression in Patients of the UMF No.20 “Vallejo”.

Note: Systemetic Arterial Hypetension;** p<0.05 Pearson’s Chi-square Test.
Table 4: Multimodal Logistic Regression Model with Parameter Estimation of the degree of Association of Depression with the Degree of Systemic Arterial Hypertension and Sociodemographic Characteristics in Patients from the UMF 20.

Note: *p < 0.05
In the present study of 1,108 patients from UMF No. 20 with a diagnosis of SAH, a total of 629 were women (56.8%) and 479 were men (43.2%); 96 patients (8.7%) were 18 to 29 years old at the time of the study, 190 (17.1%), 30 to 39 years old, 306 (27.6%) between 40 to 49 years old and 516 (46.6%) 50 to 65 years old. The prevalence of depression in married subjects compared to those who were single, where more than two thirds of the sample was in a marital union, thus having a greater probability of finding depressed patients in this area. According to Asmare, [25] since, according to various studies and sources of information, there is a lower risk of depression in married people due to the opportunity to share healthy lifestyles with their partner, as well as support each other with different aspects. daily life stressors [25] Ashok, et al. [14], report an age of presentation for depression with medium degree as the most frequent, an OR of 2.06 95% CI (1.114 -3.821) greater risk in women than in men, in our study an association of 1.7 times higher risk 95% CI (1.217- 2.386 Medium depression has a significant association with grade 1 systemic arterial hypertension in 6% 95% CI (0.013-0.305) in our study; highlighting the significant demographic factors of our study, it is presented as reported by Deng X, et al. [26] to mean depression in cerebrovascular diseases with an OR of 1.43 95% CI (1-08-1.90). Odame, et al. [27] reports in multivariable logistic regression models the inclusion of depression, hypertension and demographic factors, referring to similarities in risk in relation to age over 40 years, obesity, contrasting in marital status, where it refers to married people with 73% IC risk at 95% (0.69, 0.79) and in our study in singles with 68% risk CI at 95% (0.49, 0.99) [27].
In this research, the main objective was met, consisting of associating the level of depression with the level of essential systemic arterial hypertension in the beneficiaries of the UMF 20 “Vallejo”, where a significant inverse association was observed between both pathologies, given that most of the patients with depression and the highest degree of severity were those with a lower degree of SAH. The results of this study can contribute to improving the identification and comprehensive management of patients diagnosed with SAH and depression, considered diseases of high global prevalence, which affect different groups with different demographic characteristics. Early detection of depression in hypertensive patients is suggested, from the level of low BP numbers, considering the associated demographic factors, with subsequent follow-up by mental health services for those cases that are diagnosed with a depressive disorder.
To the management staff of the OOAD DF Norte, director of the UMF 20, to the medical staff who contributed to making this article a reality for the benefit of the users of the I.M.S.S.
The researchers of this article declare that there is no financial interest or conflict of interest.


