Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Momin Shah1*, Abdulmajeed Alharbi1, Nahush Bansal1, Mohanad Qwaider1, Mohammed Abu-Rumaileh1, Shivani Patel1, Jama Hersi1, Hafsa Shah2, Omar Sajdeya3, Mohamad Alghothani3 and Ehab Eltahawy3
Received: June 24, 2024; Published: June 27, 2024
*Corresponding author: Momin Shah, University of Toledo College of Medicine and Life Sciences, Toledo, OH, USA., 2955 Kendale drive, Apartment 102, OH 43606, USA
DOI: 10.26717/BJSTR.2024.57.008974
Introduction: Atrial fibrillation (AF) is a common arrhythmia with increasing prevalence and significant
morbidity and mortality risks. Obesity is a known risk factor for AF, and its protective impact on clinical
outcomes, known as the obesity paradox, has garnered increased attention over the past decade.
Methods: Data from The National Inpatient Sample (NIS) were analyzed, identifying patients with AF based
on ICD10-CM coding. Patients were categorized by BMI, and outcomes including mortality, length of stay, cost,
and complications were measured. Statistical analyses included univariate and multivariate regression.
Results: Among 401,055 AF patients, higher BMI was associated with decreased inpatient mortality and
shorter length of stay compared to normal BMI. However, higher BMI correlated with increased odds of acute
heart failure but decreased odds of acute kidney injury. Hospitalization costs did not significantly differ based
on BMI.
Discussion: In this nationwide study, BMI’s impact on hospitalized atrial fibrillation (AF) patients was
assessed. Patients were grouped by BMI, with higher BMI correlating with decreased inpatient mortality and
shorter hospital stays. However, higher BMI was linked to increased risk of acute heart failure but decreased
likelihood of acute kidney injury. The obesity paradox, supported by previous studies, suggests that obese AF
patients benefit from comorbidity management and anti-inflammatory effects.
Conclusion: AF patients with higher BMI demonstrated improved inpatient outcomes despite increased
risk of acute heart failure. Prospective studies are warranted to better understand the relationship between
obesity and AF and improve management strategies.
Keywords: Atrial fibrillation; Obesity; Heart failure; Arrhythmia
Abbreviations: AF: Atrial Fibrillation; BMI: Body Mass Index; NIS: National Inpatient Sample; HCUP: Healthcare Cost and Utilization Project; AKI: Acute Kidney Injury; CCI: Charlson Comorbidity Index; NIS: National Inpatient Sample
In the clinical setting, atrial fibrillation [AF] is the most frequently diagnosed arrythmia. It affects about 1-1.5% of the general population, and this number is expected to increase in the near future. By 2030, it is anticipated that the number of individuals diagnosed with AF will surpass 12 million within the United States [1,2]. There are numerous risk factors which contribute to atrial fibrillation, including advanced age, hypertension, valvular disease, and obesity [3]. This condition poses significant risks of morbidity and mortality, with recent studies indicating a concerning trend of increasing cardiovascular death rates, particularly among younger adults [2].
Obesity stands as one of the most widespread health conditions globally, with estimates suggesting that its prevalence will reach 50% by 2030 within the United States [4]. Body Mass Index [BMI] is a numerical value derived from an individual’s height and weight, which is commonly employed to screen for obesity. A healthy BMI will fall in the 18.5-24.9 range, while BMI between 25.0 and 29.9 is categorized as overweight. An individual with a BMI above 30 is typically classified as obese [5].
Obesity is a well-known independent and modifiable risk factor for AF [6]. Despite the correlation between obesity and higher prevalence of AF, there appears to be a protective effect of obesity on clinical outcomes related to AF. This phenomenon, known as the obesity paradox, has sparked significant debate and garnered increased attention over the past decade [7]. This review seeks to further explore the relationship between the two by investigating the outcomes of patients with higher BMI levels hospitalized with atrial fibrillation. The aim of our study is to determine whether atrial fibrillation patients with higher BMI levels in the hospital have worsened or improved outcomes when compared to their lower BMI counterparts. The impact of BMI on various clinical outcomes in a large nationwide sample of hospitalized patients with AF will be assessed.
Data source
The data source for this study is The National Inpatient Sample (NIS), recognized as one of the largest and most comprehensive healthcare databases in the United States. We included data for the year 2020 in this study. NIS is a crucial component of the Healthcare Cost and Utilization Project (HCUP) family of databases and software tools. The NIS is a publicly available, all-payer inpatient healthcare database designed to produce estimates of inpatient utilization, access, cost, quality, and outcomes on both regional and national scales It consists of discharge data from 20% stratified sample of all discharges from U.S. community hospitals. Hospitalization records within the NIS consist of the International Classification of Diseases, Tenth Revision, Clinical Modification diagnosis, and procedure codes.
Study Population
The patient sample was identified using the International Classification of Diseases, tenth Revision, Clinical Modification (ICD10-CM) coding system. We identified ICD10-CM codes for primary diagnosis of Atrial fibrillation (I48.91, I48.0, I48.1x, I48.2x). We also determined ICD10-CM codes for secondary outcomes included in the study including acute kidney injury (N17.0, N17.2, N17.8, N17.9, N19), acute heart failure (I50.21, I50, I50.2) and cardiogenic shock (R57.0). Patients were categorized into 5 groups based on their Body Mass Index (BMI), which included Underweight (BMI less than 18.5), Normal weight (BMI between 18.5 and 24.9), Overweight (BMI between 25 and 29.9), Class 1 obesity and Class 2 obesity (BMI between 30 and 39.9), and Class 3 obesity (BMI 40 or greater), also known as morbid obesity.
Outcomes Measured
The objective of the study is to investigate the inpatient outcomes for patients admitted with atrial fibrillation based on their body mass index. Primary outcomes of interest included inpatient mortality, length of stay, and hospital cost, while secondary outcomes encompassed acute kidney injury (AKI), cardiogenic shock, and acute heart failure. The independent variable of interest was BMI, and potential confounders that were adjusted for included age in years, sex, Charlson Comorbidity Index (CCI), hospital bed size, hospital teaching status, primary expected payer, and hospital location.
Statistical Analysis
In line with the Healthcare Cost and Utilization Project data use agreement, we omitted reporting variables with a small number of observations (≤10) to uphold patient privacy and prevent identification risks. Statistical analyses were executed using STATA version 17.0 software. We presented categorical variables as percentages and continuous variables as mean ± SD. Student’s t-test compared continuous variables, while chi-square tests assessed categorical variables. Our analysis initiated with univariate regression analysis to compute unadjusted odds ratios and means for primary and secondary outcomes. Subsequently, multivariate regression analysis, including significant variables identified from univariable regression, was performed, repeating this process for each subgroup.
Baseline Characteristics
A total of 401,055 patients with a primary diagnosis of atrial fibrillation were included in this study. The distribution of BMI among patients was as follows: 7% had a BMI less than 19, 4.4% had a BMI between 20 and 24.9, 8.3% had a BMI between 25 and 29.9, 56.5% had a BMI between 30 and 39.9, and 23.6% had a BMI equal to or above 40. Female patients represented approximately 45% of all patients across all BMI groups, except for individuals with a BMI less than 19 and those with a BMI above 40, where females comprised 63% and 55% respectively of these subgroups. The predominant race was Caucasian, accounting for approximately 80% of the atrial fibrillation population (P ≤ 0.001). Around 70% of hospital stays with atrial fibrillation were covered by Medicare insurance (P ≤ 0.001), and most cases were treated in large urban teaching hospitals (P ≤ 0.001). The most common comorbidity was hypertension, affecting around 50% of the patient population (P ≤ 0.001), followed by coronary artery disease (approximately 32%, P ≤ 0.001), and chronic pulmonary disease (more than 27%, P ≤ 0.001) (Table 1). illustrates the baseline demographic and characteristics of patients admitted for atrial fibrillation divided among different BMI groups.
Table 1: Baseline Demographic and Characteristics of patient who admitted for Atrial fibrillation and divided among different BMI groups.
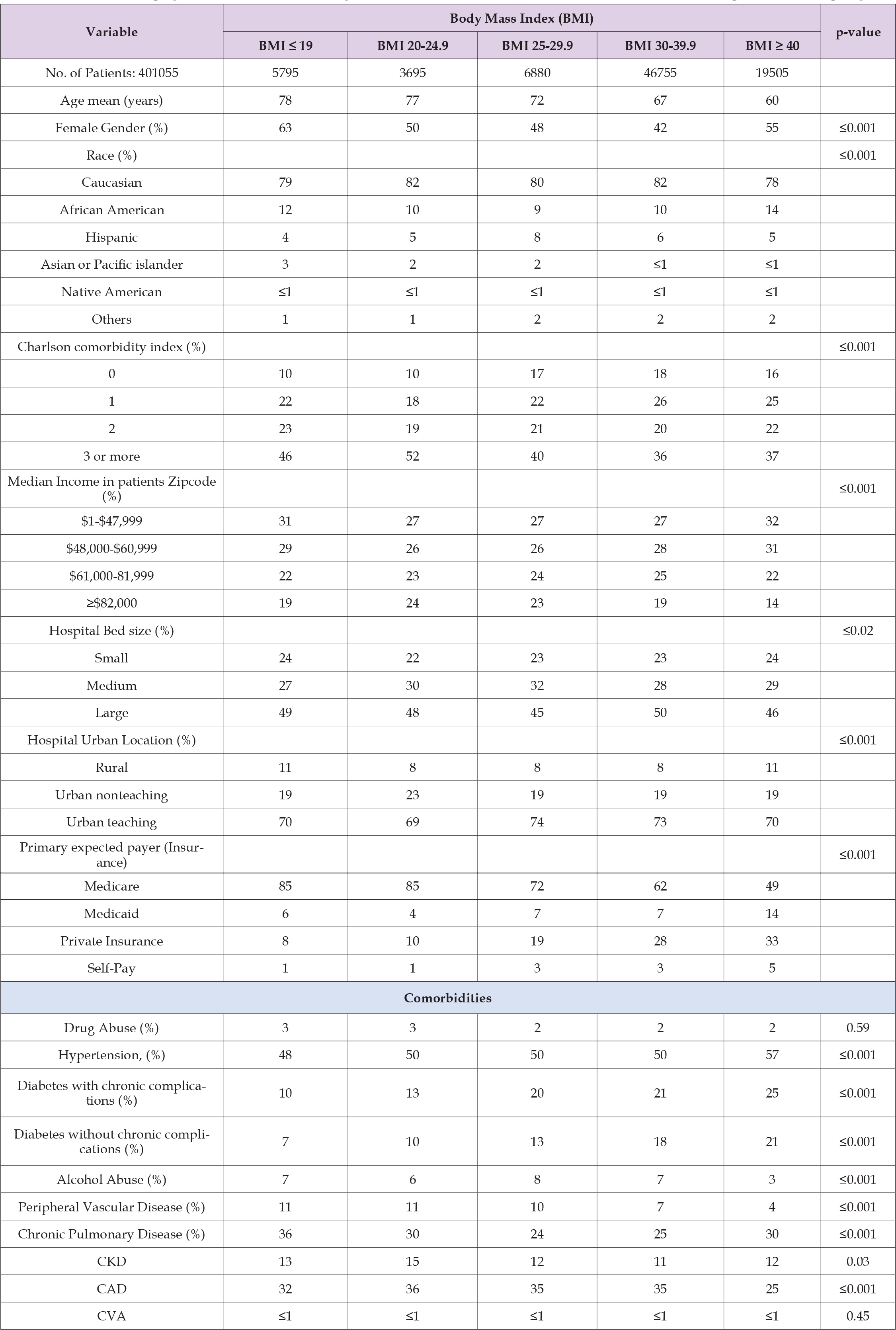
Note: P-value ≤ 0.05 indicates significance.
In-Hospital Mortality, Length of Stay, and Hospitalization Cost
In comparison to the standard BMI range of 20 to 24.9, higher BMI group patients i.e. BMI of 25 or higher had decreased inpatient mortality as revealed for BMI 25-29.9 group [adjusted odds ratio 0.43, 95% CI 0.21-0.87] and BMI 30-39.9 group [adjusted odds ratio 0.25, 95% CI 0.14-0.49] with p-values of 0.02 and <0.001 respectively (Table 2). Individuals with a BMI of 25 or higher exhibited a statistically significant reduction in the length of stay compared to those with a normal BMI, with the mean ranging from -1.04 days to -1.81 days (P value: ≤0.001). There was no difference in the length of stay between underweight patients with a BMI of 19 or less and those with a normal BMI. [adjusted odds ratio -0.25, 95% CI -1.06-0.57, p-value 0.55] (Table 2) Compared to the normal BMI range of 20 to 24.9, there was no significant difference in hospitalization costs across all other BMI groups.
Table 2: Primary outcomes among patients admitted for Atrial fibrillation and divided among different BMI groups.
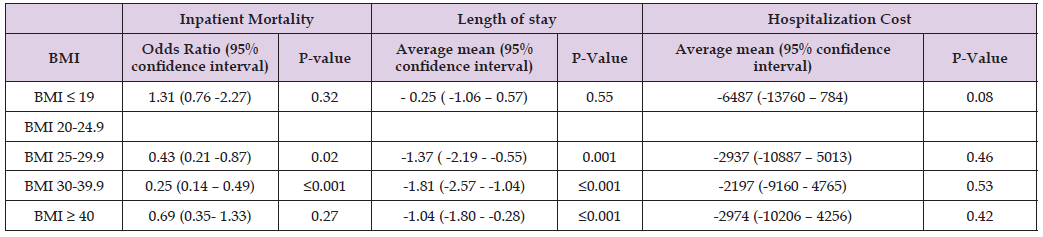
Note: P-value ≤ 0.05 indicates significance.
BMI is compared to the normal BMI 20-24.9
Acute Heart Failure, Acute Kidney Injury (AKI) and Cardiogenic Shock
Patients with a BMI of 30 or higher had higher odds of developing acute heart failure compared to those with a normal BMI (adjusted odds ratio 1.56, 95% CI 1.24-2.95, P value: ≤0.001 for BMI 30-39.9 and adjusted odds ratio 1.95, 95% CI 1.52-2.48, p-value ≤0.001 for BMI more than 40 group). Patients with a BMI of 19 or less showed no difference in acute heart failure risk compared to those with a normal BMI. (adjusted odds ratio 0.88, 95% CI 0.67-1.16, p-value 0.38) (Table 3) Within the BMI range of 25 to 39.9, patients demonstrated reduced odds of developing Acute Kidney Injury (AKI) in comparison to those with a normal BMI (P value < .05). Patients with a BMI below 19 or above 40 showed no difference in AKI risk when compared to those with a normal BMI. There was no statistically significant difference in the incidence of cardiogenic shock among patients with atrial fibrillation in different BMI groups compared to those with normal BMI.
Table 3: Secondary outcomes among patients admitted for Atrial fibrillation and divided among different BMI groups.
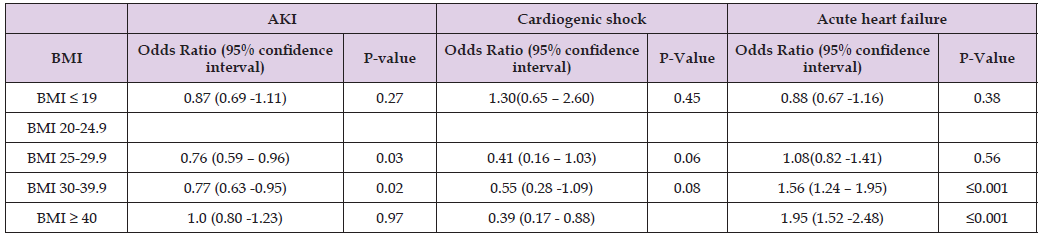
Note: P-value ≤ 0.05 indicates significance.
BMI is compared to the normal BMI 20-24.9.
In our study, we included 401,055 patients with primary diagnosis of atrial fibrillation in our analysis and investigated the impact of BMI on different variables like in-hospital mortality, length of stay, cost of hospitalization, and development of complications like acute kidney injury or acute heart failure. Our study demonstrates that first, patients with higher BMI i.e. BMI of 25 or higher were associated with decreased inpatient mortality in comparison to patients with normal BMI (20-24.9). Second, patients with BMI of 25 or higher exhibited a statistically significant modest reduction in the length of stay compared to those with a normal BMI. Third, patients with higher BMI demonstrated reduced odds of developing Acute Kidney Injury (AKI) and higher odds of developing acute heart failure compared to those with normal BMI.
In this nationwide observational study, we aim to evaluate the impact of BMI on the outcomes of patients admitted to the hospital with atrial fibrillation. For this purpose, patients were segregated into five BMI groups, with reference group taken as the normal BMI of 20- 24.9. Findings of the study showed that first, higher BMI groups i.e. patients with BMI more than 25, had significantly decreased inpatient mortality when compared to patients in the reference group. Second, compared to atrial fibrillation patients with normal BMI, patients with BMI more than 25 had a shorter length of stay in the hospital. Third, patients with higher BMI (BMI 30 and higher) had a significantly higher risk of developing acute heart failure when compared to patients with normal BMI. Fourth, atrial fibrillation patients with BMI 25 and above exhibited a decreased likelihood of developing acute kidney injury when compared to patients with normal BMI.
It is important to note that while higher BMI groups exhibit decreased inpatient mortality and reduced risk of AKI, this trend does not apply to individuals with a BMI over 40. The influence of BMI on atrial fibrillation is extremely significant, with Mendelian randomization studies showing a causal relationship between obesity and atrial fibrillation [8]. Obesity is a certainly a well-known risk factor for development of atrial fibrillation, and higher BMI, as suggested by our study may be associated with decreased in-hospital mortality and length of stay in AF patients. This finding is consistent with the ‘obesity paradox’ which has been demonstrated in studies previously. In an observational study conducted by Sandhu et al. namely the ARISTOTLE trial involving 17,913 patients [9], patients were categorized as normal (BMI 18.5 to <25 kg/m2), overweight (BMI 25 to <30 kg/ m2), and obese (BMI ≥30 kg/m2). Higher BMI groups had a lower all-cause mortality and a lower occurrence of a composite end point which included stroke, systemic embolism, and myocardial infarction. Similarly, among 21,028 patients segregated into six BMI groups in the ENGAGE AF-TIMI 48 trial, higher BMI was independently associated with a lower risk of stroke, systemic embolization, and better survival [10]. Certain independent observational studies demonstrated no significant difference in mortality outcomes with BMI in atrial fibrillation patients. Among these studies was the FANTASIIA registry report, which showed that higher BMI among AF patients did not correlate with increased mortality or adverse outcomes when compared to non-obese AF patients [11].
Several hypotheses can be suggested to explain the phenomenon of obesity paradox observed in atrial fibrillation. Higher BMI is an established risk factor for various comorbidities, which means that these patients tend to be prescribed effective medications affecting cardiovascular morbidity and mortality including beta blockers, statins, RAAS blocking agents etc. [11]. Evidence supporting this idea arises from the fact that obese patients with pre-existing chronic conditions show even more favorable outcomes compared to those without known comorbidities [12]. A recent study linked atrial fibrillation with elevation in the multiple inflammatory markers, with a nidus of inflammation probably related to the pulmonary veins [13]. High metabolic reserves in obese patients likely help to counter the catabolic effects of this inflammatory state, rendering a protective effect in higher BMI groups. Furthermore, obese patients also benefit from various anti-inflammatory adipokines including soluble tumor necrosis factor-alpha receptor and higher levels of lipoproteins, which assist in neutralizing inflammatory pathways and endotoxins [13]. Obesity and cardiovascular diseases are associated with poor quality of life and functional impairment [14], which may lead to these patients getting early medical evaluation. Thus, better outcomes seen in obese patients with atrial fibrillation could be attributed to survival bias. As opposed to obese patients, underweight AF patients have been shown to have worse outcomes [10,15].
Inadequate reserves and body resources secondary to poor nutrition exacerbate cardiac cachexia, resulting in a poorer prognosis. Our study showed an increased risk of development of acute heart failure in admitted AF patients with higher BMI compared to patients with normal BMI. Obesity is a predisposing factor for development of heart failure as it causes structural and functional changes in the left ventricle and has adverse effects on hemodynamics including increase in the total blood volumes and resulting LV remodeling [16]. Furthermore, the concept of obesity paradox extends beyond atrial fibrillation, as seen in our study, and is even more pronounced in heart failure [13]. When interpreting the results of this study, it is important to acknowledge several limitations. Firstly, the reliance on a database for data collection introduces the possibility of documentation and coding errors, which could have affected the accuracy of the analyzed data. Such inaccuracies may influence the study’s results and subsequent conclusions. Secondly, the lack of longitudinal tracking of patient outcomes within the database may result in underreporting of adverse events, especially mortality rates. Thirdly, the database records hospitalizations as separate entries, without considering repeated hospitalizations of the same patient, potentially influencing outcome analyses.
In conclusion, our study showed that AF patients with higher BMI had decreased inpatient mortality and shorter length of stay, when compared to patients with normal BMI. Also, when compared to the reference group, patients with higher BMI had a greater likelihood of developing acute heart failure but a lower probability of experiencing acute kidney injury. Our findings underscore the need for further prospective studies to evaluate the link between obesity and AF, which should aid in preventing and effectively managing patients with atrial fibrillation.
Declaration of Generative AI and AI-Assisted Technologies in the Writing Process
During the preparation of this work the authors used ChatGPT to enhance grammar and writing, ensuring accuracy and clarity throughout the article. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
The authors declared no conflict of interest.
None.
All authors drafted the manuscript, critically revised the manuscript and reviewed the literature. All authors read and approved the final manuscript.
• All authors have participated in the work and have reviewed
and agree with the content of the article.
• None of the article contents are under consideration for
publication in any other journal or have been published in any
journal.
• No portion of the text has been copied from other material
in the literature (unless in quotation marks, with citation).
• I am aware that it is the authors responsibility to obtain permission
for any figures or tables reproduced from any prior publications,
and to cover fully any costs involved. Such permission
must be obtained prior to final acceptance.
This study was deemed exempt by the Institutional Review Board of the University of Toledo, as it was a database study that included de-identified patient information.
The authors declare that all the data supporting the findings of this study are available within the manuscript.


