Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ekene Agatha Emeka1,2, Akabuogu Uchechi Williams2, Akwiwu-Uzoma Chodozie Valentine2, Esther Ngozi Umeadi3, Sylvia Tochukwu Echendu2, Chika Ifeoma Ofiaeli1,2, Arinze Anthony Onwuegbuna4, Hyacinth Tochukwu Eze5, Onyeka Chukwudalu Ekwebene6, Ngozichukwu Gertrude Uzoewulu7, Emeka Stephen Edokwe3, Chidinma Theresa Ezidiegwu8, Kingsley Chidiebere Nwaogu9, Johnbosco Emmanuel Mamah10 and George Uchenna Eleje11*
Received: April 30, 2024; Published: May 14, 2024
*Corresponding author: George Uchenna Eleje, Effective Care Research Unit, Department of Obstetrics and Gynaecology, Nnamdi Azikiwe University, Nigeria
DOI: 10.26717/BJSTR.2024.56.008872
Background: Respiratory illnesses are a major cause of morbidity and mortality especially in developing
countries like Nigeria where healthcare services are largely inaccessible.
Objectives: This study was done to ascertain the prevalence and outcomes of infants treated for respiratory
tract infections.
Methods: This study was conducted in the Children’s Emergency Room (CHER) of Nnamdi Azikiwe University
Teaching Hospital, Nnewi, Nigeria over a 2-year (January 2021 to December 2022) period. We retrieved clinical
records of infants. A proforma was used in extracting the required information. Data was analyzed using
SPSS version 25. Ethical clearance was obtained from Nnamdi Azikiwe University Teaching Hospital Ethics
Committee.
Results: Out of a total of 694 infants were admitted over the specified period, 142 (20.5%) had ARTI. The
age range of patients was between 0 to 12 months, mean age was 5.79 (±3.51) months. More males were
affected (55.6%) than females 44.4%. The highest number of cases recorded was in November (22.5%), while
the least was in January (0.7%). The most common diagnosis was bronchopneumonia occurring in (83.8%) of
patients while the least recorded diagnosis was tonsillitis occurring in (2%) of patients. Most patients (75.4%)
were discharged, and (4.2%) were discharged against medical advice, while 20.4% died. Most of the deaths were
attributed to bronchopneumonia complicated with sepsis (75.8%).
Conclusion: The prevalence of ARI in this study was 20.5%. There was an increased prevalence during the early
period of wet and dry season. Sepsis with bronchopneumonia was the most common cause of mortality.
Keywords: Respiratory Illnesses; Healthcare Services; Clinical Records; Bronchopneumonia And Tonsillitis
Keywords: Ultrastructure; Mitochondria; Membrane; Respiratory Ensembles
Respiratory tract infections (RTIs) refer to any infectious illness affecting the upper, lower, or both respiratory tracts. Upper respiratory tract infections (URTIs) encompass conditions like laryngitis, the common cold, pharyngitis, acute rhinitis, tonsillitis, acute rhinosinusitis, and otitis media [1]. Lower respiratory tract infections (LRTIs) include acute bronchiolitis, bronchitis, tracheitis, and pneumonia. In 2017, approximately 5.4 million children under the age of five died globally, with about half of these deaths occurring in sub-Saharan Africa [2]. Acute Respiratory Tract infections were the leading cause of mortality among this demographic [2].
Acute respiratory infection refers to an infectious condition that can disrupt normal breathing patterns. It may specifically target either the upper respiratory tract, encompassing the area from the sinuses to the vocal cords, or the lower respiratory system, extending from the vocal cords to the lungs. This ailment poses significant risks, especially to children, older individuals, and those with compromised immune systems [3-6]. Symptoms vary depending on whether the upper or lower respiratory tract is affected, and can include congestion in the nasal sinuses or lungs, a runny nose, coughing, sore throat, body aches, and fatigue [3].
On a global scale, respiratory diseases stand as the leading cause of illness and death, particularly affecting infants and young children [4]. Pneumonia continues to represent a significant contributor to childhood mortality, resulting in nearly 1.3 million deaths annually, a substantial portion of which could be prevented. Paediatric tuberculosis accounts for as much as 20% of the total tuberculosis burden in countries with high incidence rates [5,7-9]. Despite advancements in modern medicine, Acute Respiratory Infections (ARIs) persist as the most prevalent type of infectious disease, even in many developed nations such as the USA. ARIs, collectively comprising a range of diseases and symptoms, rank among the primary causes of morbidity and mortality in pediatric populations across sub-Saharan Africa, where more than 10% of children succumb before their fifth birthday [10- 13]. In Nigeria alone, the World Health Organization (WHO) estimated that 868,000 children under the age of five died from pneumonia in 2010. With an annual toll surpassing 140,000 children, Nigeria holds the highest ARI-related childhood mortality rate in Africa and the second-highest globally [14,15].
ARIs are affected by socio-demographic and socio-cultural risk factors, which can be modified with simple strategies. It is recommended that control programs for ARIs should be multifaceted with a strong political will [16].
Acute respiratory tract infection in children remains a killer disease in both low and middle-income countries and high-income countries. Infants are highly susceptible to these infections because of their low immune system and dependence on adults who may end up transmitting the infectious agent to them [17]. In the present study, we aimed to assess the prevalence and outcome of ARIs among infants in a Nigerian tertiary health care institution.
Study Area
The study was done in the Children Emergency Room of Nnamdi Azikiwe University Teaching Hospital, Nnewi, south-east Nigeria.
Study Design
This study is a 2-year retrospective cross sectional study of the prevalence and outcome of respiratory tract infection in infants.
Study Population
The study included infants, who visited the children’s emergency room in NAUTH, Nnewi to access care from January 2021 through December 2022.
Inclusion Criteria
Children, less than a year were managed for ARIs in CHER, NAUTH, Nnewi.
Exclusion Criteria
Children greater than one year. Children less than a year who accessed care in the children’s emergency room, NAUTH Nnewi, whose data could not be obtained from the Nursing register.
Sample Size Determination
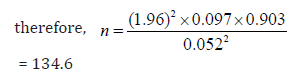
This was calculated using the Cochrane formula, which is given as;
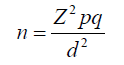
Where n is the minimum sample size
Z is standard normal deviate = 1.96
P is the population proportion = 9.7 percent.47
q=(1-p); 100-9.7= 90.3 percent
d is the degree of precision = 0.05
Sampling Technique
A convenience sampling technique was used to obtain data of infants who met the inclusion criteria from the nursing register, and from the records department of NAUTH, Nnewi.
Study Instruments
A proforma was designed to record the patients’ profile which included: age, sex, diagnosis, year, season of diagnosis, and outcome of the diagnosis.
Data Analysis
All available data were analyzed using a statistical package for social sciences (SPSS Version 25.0). Variables analyzed included age, (which is continuous data), sex, season, and year of diagnosis of the disease. Categorical variables were analyzed using percentages and proportions while continuous variables were analyzed using mean and standard deviation and the association between categorical variables was analyzed using the chi-square test. The level of significance was set at p< 0.005.
Ethical Considerations
This research work was done with approval from the Nnamdi Azikiwe University Ethics Committee with approval number of NAU/ HREC/28/02/12/2023/05. Permission was also gotten from Records Department of Nnamdi Azilkiwe University Teaching Hospital, Nnewi. Information obtained from case notes was used only for this project and the patient’s identity was kept strictly confidential.
The data used for analysis was obtained from records of patients admitted at CHER. The mean age and SD were calculated as 5.79 ± 3.51 months. The majority were under 4 months (42.3%). There were more males (55.6%) than females (44.4%) as shown in Table 1. Table 2 shows the prevalence of acute respiratory infection. A total of six hundred and ninety four infants were admitted during the period of study. Among these, one hundred and forty-two infants had acute respiratory infections. The prevalence of acute respiratory infection was therefore determined as 20.5%. Table 3 shows the distribution of cases according to year and month, while Figure 1 shows the graphical presentation of Case distribution according to month and year. A higher occurrence of ARI was recorded in the year 2022 (70.4%) when compared to that of 2021 (29.6%). In 2022, the prevalence of ARI was higher in November (27.0%) and December (24.0). But in 2021, ARI was recorded higher in March (23.8%) and June (26.2%). Table 4 shows the distribution of acute respiratory tract infection according to specific diagnosis. Bronchopneumonia ranked highest amongst ARIs seen in these children while tonsillitis was the least. The majority of the infants were discharged (75.4%). It was noted that 4.2% were discharged against medical advice.
Mortality was seen in 20.4% of cases. Figure 2 shows the association of outcome with some variables while Table 5 shows the association of treatment outcome with some variables. The relationship between treatment outcome and variables (age, sex, gender and year) is presented in Table 5. The outcome of treatment showed a significant association with age (X2 = 13.836; p = 0.006). The number of patients discharged was significantly higher among the 0-4 months age category. Mortality was recorded highest among the 9-12 months age group. Treatment outcome showed no significant association with sex and year (p > 0.05 in these cases). Table 6 shows the distribution according to comorbidities and causes of Mortality. Sepsis with Bronchopneumonia was the highest cause of mortality among infants with ARIs, contributing about 75.8%. There is also a significant relationship between mortality and protein energy malnutrition.
The aim of this study was to determine how common acute respiratory infections (ARIs) are among infants at a tertiary healthcare facility and what outcomes result from them. Analysis of the data revealed that out of 694 infants admitted during the study period, 142 were diagnosed with ARIs, indicating a prevalence rate of 20.5%. This underscores the substantial burden of ARIs within this age group, emphasizing the urgency for prompt interventions to reduce the associated illness and mortality rates. The prevalence identified in this study (20.5%) aligns closely with findings from Memeli et al, whose study on preschool children showed a prevalence of 24.9% [21]. Similarly, it corresponds well with Eberechukwu et al’s study at the University of Port-Harcourt, Nigeria, which documented a prevalence of 27.1% [18]. However, Abayneh et al and Kumar et al, in India, recorded higher prevalence rates of 40.7% [19] and 59.1% [20], respectively. These variations in prevalence may stem from differences in sampling techniques; while our study employed a retrospective approach, Kumar et al conducted a cross-sectional prospective study [21]. Additionally, the significant overcrowding in India, recognized as a risk factor for acute respiratory infections (ARIs), likely contributes to the elevated prevalence observed in their research [21]. Conversely, Ofaeli et al’s study at NAUTH, Nnewi, Nigeria reported a lower incidence of 14.45%, possibly influenced by their inclusion of patients spanning ages 0-17 years, making it challenging to determine the exact prevalence among infants [22].
Bronchopneumonia stands out as the primary culprit behind acute respiratory infections (ARIs) in infants, constituting 83.5% of cases, with bronchiolitis trailing behind at 9.5%. This finding echoes Rashmi et al’s findings, where bronchopneumonia accounted for 72.5% of ARIs among children [23]. The heightened prevalence of ARIs raises significant public health concerns, as it imposes strains on healthcare systems, depletes medical resources, and raises the risk of potential outbreaks. Given the ease with which ARIs can spread, particularly among vulnerable populations like children, effective prevention and management strategies are essential for curbing hospitalizations, averting complications, and mitigating overall healthcare expenditures. In our investigation, we delved into the impact of monthly and seasonal fluctuations on the prevalence of acute respiratory infections (ARIs) among infants. Out of the total 142 ARI cases examined, 81 occurred notably between November and March (dry/ harmattan season), while 61 were recorded between April and October (rainy season).
Noteworthy increases in ARI incidence were observed in June (19%), November (32%), and December (28%), coinciding with the onset of the rainy and dry seasons. This phenomenon could be attributed to the observed weakening of the immune system during seasonal transitions. These findings align with Abayneh et al’s study, which similarly highlighted peaks in ARI prevalence among under- fives in June (23.8%), November (15.9%), and December (14.7%) [24]. The public health implication of these trends is significant: during the onset of the rainy season, increased indoor activities may facilitate disease transmission, while the early dry season’s dry air may exacerbate respiratory tract irritation, heightening susceptibility to severe forms of ARIs. The study observed a slightly higher prevalence of acute respiratory infections (ARIs) among males (55.6%) compared to females (44.4%), consistent with findings by Ujunwa et al, who reported a male prevalence of 51% and female prevalence of 49% [9]. This trend also aligns with research conducted by Gabriel et al, which found a prevalence of 50.2% in males and 49.8% in females [24].
This disparity may stem from the greater activity levels of male infants, leading to increased environmental exposure. The slight male predominance in ARI prevalence holds potential public health implications, suggesting possible physiological differences between the sexes in susceptibility to respiratory infections. Tailored public health strategies might be necessary to address these differences, including enhancing healthcare access for male infants and educating caregivers on infection prevention. Further research is warranted to delve deeper into the underlying factors and to develop effective interventions. The study also examined the discharge outcomes of acute respiratory infections (ARIs) among infants. Out of the total 142 cases analyzed, 75% were discharged, while mortality accounted for 20.4%, and 4% were discharged against medical advice. This finding contrasts with a similar study conducted by Alok et al, which reported a lower mortality rate of 9% [25].
The variance could be attributed to the inclusion of both in-patients and outpatients in their study, whereas our research focused solely on in-patients in the emergency room, where mortality rates tend to be higher. The elevated mortality rate from ARIs in infants raises significant public health concerns due to its impact on a vulnerable population, imposing substantial economic burdens and potentially leading to long-term health implications. Implementing preventive measures and interventions is imperative for reducing this mortality rate and promoting the overall health and well-being of infants. The primary cause of mortality observed in this study was sepsis accompanied by bronchopneumonia, accounting for 75.3% of cases, followed by sepsis with bronchiolitis and acute respiratory infections (ARIs) with protein energy malnutrition, each contributing to 10.3% of mortality cases. Consequently, sepsis alone was responsible for the mortality of 86.6% of infants admitted to the Children’s emergency ward. These findings align with research conducted by Trenton et al, which similarly found that sepsis alone accounted for approximately 80% of mortality cases [26].
Sepsis presents a critical public health concern due to its potential to lead to high mortality rates among infants. Timely and appropriate medical care, along with preventive measures, are essential to address this issue and safeguard the well-being of infants. The major strength of this study lies in the currency of its findings and its exclusive focus on infant data. However, there are several limitations to our study. First, due to the small sample size, we cannot conclude significant differences in the association between various sociodemographic variables and cute respiratory infections. Due to the retrospective cross-sectional design, we lacked information regarding causality in relation to mortality [27-31].
Acute respiratory infections (ARIs) pose a significant burden in our community, evident by a prevalence of 20.5% among infants admitted to a tertiary healthcare facility. This raises concerns and underscores the need for additional interventions to alleviate the impact of this disease on the population. Seasonal variations also influence the prevalence of ARIs, with notable increases observed during the peak of both the rainy and dry seasons. Males exhibit a slightly higher susceptibility to ARIs compared to females. Bronchopneumonia remains the most common cause of ARIs among infants in our study, with most mortality cases complicated by sepsis. Given that respiratory tract infections in children are highly preventable, it is essential to implement measures to mitigate the rising incidence and associated complications. Recommendations include ongoing training and retraining of healthcare personnel by hospital management to recognize early signs of sepsis, aiming to prevent mortality. Additionally, healthcare staff should prioritize the early diagnosis of congenital anomalies and promptly refer affected infants to specialists for appropriate management. Ensuring timely diagnosis and effective management of respiratory illnesses is crucial to prevent the development of life-threatening complications.
Conflict of Interest Statement
The authors report no conflicts of interest concerning this work.
Funding Statement
There is no special funding. This work was self-funded by the Researchers.
Ethical Statement
Ethical approval was obtained from the Nnamdi Azikiwe University Ethics Committee with approval number of NAU/ HREC/2S/02/12/2023/05. This study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We are grateful to the Medical record department and department of Paediatrics for their cooperation during this study.
Author Contributions
Design: EAE, AUW, ACV and ENU. Analyses: AUW and STE. Writing: CIO, AAO, THE, OCE, NGU, and ESE. Supervision: EAE, GUE and JEM. CIO, AAO, THE, OCE, NGU, AUW, ACV, STE, CTE, KCN and GUE contributed to the interpretation of the analyses and writing of the manuscript. All authors approved the final manuscript.


