Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Chikkalur P*, Simons A, Jain M and McBride T
Received: April 08, 2024; Published: April 15, 2024
*Corresponding author: Chikkalur P, The Royal Wolverhampton NHS Trust, Wolverhampton, United Kingdom
DOI: 10.26717/BJSTR.2024.56.008798
Background: The Signature One planning system from Zimmer Biomet offers significant flexibility in glenoid baseplate placement for shoulder replacement surgeries yet lacks a specific accompanying protocol. To address this gap, we devised a method aimed at ensuring consistent glenoid component positioning within the 3D planning software. We evaluated the intra and inter-observer reproducibility of this protocol.
Methods: Twenty patients scheduled for reverse shoulder arthroplasty underwent CT scans following Zimmer-Biomet Protocol. Three orthopedic surgeons conducted 3D templating twice over a 4-week interval, varying the patient order. Measurements included 6 degrees of freedom for glenoid positioning (A-P and superior-inferior, version, inclination, rotation, and reaming depth), as well as central screw length. Intra Class Correlation (ICC) was employed to assess agreement.
Results: Our protocol demonstrated excellent reproducibility, with ICC ranging between 0.81 and 0.96 for inferior tilt, rotation, and screw length, and substantial agreement for reaming depth (ICC 0.79). Moderate agreement was observed for the original baseplate placement (ICC 0.66), with similar results in intra-observer trials after a four-week interval (ICC 0.97-0.64). Post-augmentation, mean implant-to-bone contact was 91.38%.
Conclusion: Our established protocol for CT-based 3D templating ensures reliable sizing and alignment of components in reverse shoulder arthroplasty. This standardized approach offers considerable benefits by promoting consistency and reproducibility among users of the software, thereby enhancing surgical planning outcomes.
Abbreviations: ICC: Intra Class Correlation; RSA: Reverse Shoulder Arthroplasty; 3D: Three-Dimensional; CT: Computed Tomography
Reverse Shoulder Arthroplasty (RSA) has seen a significant increase in utilization worldwide in the past several years as it can offer excellent function to patients with a gamut of glenohumeral pathology including rotator cuff tear arthropathy, glenohumeral arthritis with severe glenoid bone loss [1,2], acute and delayed treatment of proximal humerus fractures [3], failed anatomic shoulder arthroplasty, chronic shoulder dislocations [4], massive irreparable rotator cuff tears, and rheumatoid arthritis. RSA use is likely to continue to increase due to the aging population, expanding indications, and increased surgeon experience with the prosthesis. Long term outcomes have been encouraging, with overall survivorship of 91–93% at minimum 10-year follow up and persistently improved outcome scores [5,6]. Improving glenoid implant survivorship over time is one of the more crucial elements of research relating to shoulder arthroplasty. Over the past ten years, much attention has been paid to improving the accuracy of glenoid implant positioning. The shoulder is a highly mobile joint, and stability of this joint is a delicate combination of multiple factors, including bone orientation, ligamentous restraints, and periarticular muscle balance [7]. Inferior placement of the glenoid baseplate allows inferior overhang of the glenosphere which reduces notching of the glenoid neck. Superior tilt is associated with instability and should be avoided. Inferior tilt reduces sheer stress and notching [8]. Removal of excess bone inferiorly increases micromotion and reduces mechanical stability of the implant [9].
Finally increased central screw length improves baseplate compression against bone and improves stability [10,11] Three-Dimensional (3D) reconstruction of the scapula and 3D measurements of glenoid retroversion, inclination, and humeral head subluxation are increasingly recognized as necessary references during the preoperative planning and decision-making process for total shoulder arthroplasty [12]. Three-Dimensional planning software for shoulder replacements has been introduced by several manufacturers over the past few years. The software allows accurate visualization of the 3-D topography of the glenoid, and aids decisions as to where to place the glenoid implant, correcting superior/inferior tilt, and retro/anteversion [13]. While the effect of three-dimensional (3D) planning for total shoulder 3 arthroplasty (TSA) on component positioning and patient outcomes has been increasingly studied, the effect of 3D planning on surgeon decision making has not been well studied [14]. The Signature One planning system from Zimmer Biomet does not have any specific protocol accompanying it, allowing surgeons a wide freedom to place the glenoid baseplate. Taking the above principles into account, and attempting to maximize bone preservation in the glenoid, we have developed a method for use of the software which we believe gives consistent placement of the glenoid components. This will be of advantage to less experienced shoulder surgeons, and new users of the planning software. We then tested this protocol for both intra and inter user variability.
A total of 20 patients who needed reverse total shoulder arthroplasty were added to this prospective study. All had been listed for a reverse shoulder arthroplasty by their treating surgeon. A CT scan of shoulder was done according to Zimmer Biomet Protocol. (Slice thickness: 1mm x 1mm or less, constant throughout acquisition with scan spacing of 1mm or less (equal to slice thickness). The CT scan once done was reconstructed into 3D by the company and uploaded onto signature one planning software. This was assessed by 3 independent shoulder surgeons, 2 with good volume of arthroplasty caseload and a fellow in shoulder surgery. Each case was planned by the surgeon and then planned again at a minimum of 4-week interval. The measurements for each planning round were kept separate thereby blinding the surgeons from their first results. The results of the study were independently collated and analyzed by another surgeon.
Planning Protocol
In the signature One planning system, the initial placement of the glenoid baseplate is done by a non-medically trained software technician and is not meant to provide any guidance for the surgeon. However, this initial placement was retained as a consistent starting point for all three surgeons (Figure 1).
• Step 1: The mini baseplate can be adjusted in an AP direction, and a superior/inferior direction until the surgeon is comfortable with the fit of the baseplate on the inferior aspect of the glenoid. Movement from the initial placement position was recorded in terms of mouse clicks (0.5 mm). Movement inferiorly, and or anteriorly from starting position were recorded as positive number and movement superiorly or posteriorly recorded as negative number.
• Step 2: There is little evidence that a small degree of anteversion or retroversion makes a significant difference in reverse shoulder arthroplasty. We adjusted anteversion/retroversion of the implant to give the best fit and best length for the central screw, still allowing for cortical fixation at the anterior aspect of the glenoid vault. The degree of anteversion correction done were recorded.
• Step 3: The inferior tilt of glenoid was set at -10 degree and any changes made to reduce the tilt if the screw penetrates the supraspinous fossa were recorded (Figure 2).
• Step 4: The surgical technique for the glenoid augments states that initial reamer is advanced until there is 50% contact between the reamer and bone. We mimicked this in virtual space within the planning software by selecting the mini baseplate and initially set the depth so that there was just contact at one point between the baseplate and the most prominent part of the glenoid. We then advanced the virtual baseplate medially until there was 50% or greater contact between it and the bone. This is the minimum reaming depth consistent with placement of the augmented glenoid baseplate. The depth tool in the software was used to record the initial reaming depth (Figure 3).
• Step 5: Almost all glenoid showed asymmetric wear and the formation of a neo glenoid. This wear was usually superior, but there was often posterior wear too, giving a more complex pattern that is appreciated with 2-d planning. The reaming already done shows a “horizon line”, and the mini baseplate was rotated so that the superior hole was positioned perpendicular to this horizon. The horizon was usually visible in the two lateral screw holes, and the position could be fine-tuned by ensuring that the amount of reamed bone (yellow) and the non reamed bone (Beige) was equal in the two lateral screw holes. The amount of rotation required was recorded (Figure 4).
• Step 6: Without further advancing the baseplate into the bone, a small augment, then a medium augment, then a large augment was tried, until bone contact of over 90% was achieved (Figure 6).
• Step 7: The central screw length was then adjusted to give penetration of both the anterior threads and the screw tip through the cortex of the anterior glenoid vault (Figure 5).
• Step 8: Each surgeon then made a subjective assessment as to whether they felt a Patient specific guide was required to achieve the planned position, or if they felt the planned position could be achieved using the pin guides provided on the instrument tray.
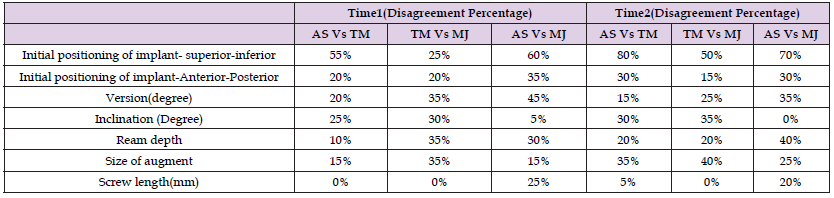
A professional statistician carried out the statistical analysis using SAS 9.4 (SAS Institute 109 Inc., Cary, NC, USA).The inter-observer and intra-observer reliability, was carried out to assess the reliability of positioning of the mini base plate in antero-posterior and super-inferior plane on glenoid, the version and inclination of glenoid and depth of reaming (3dimensional positioning with 6 degrees of freedom) the percent agreement and Intraclass Correlation Coefficient (ICC )were evaluated. ICC also was used to investigate reliabilities of the rotation of base plate needed to achieve maximal bone contact and the screw length. For inter-observer trials, the agreement rate and ICC were calculated for each unique pair of the three observers, the average of these values was recorded as the overall value and compared as in the intra-observer trials. An ICC of < 0.20 is slight agreement, 0.21 – 0.40 is fair agreement, 0.41 – 0.60 is moderate agreement, 0.61 – 0.80 is substantial agreement, and >0.80 is almost perfect agreement [15] (Table 1).
Table 1: Describes the descriptive statistics assessment of each independent orthopedic surgeons in both time points.
Interobserver Reliability
The mean ICC for the initial positioning of the mini baseplate was found to be in moderate agreement (ICC Super- inferior-0.69, antero-posterior-0.58). The mean version of the implant was found to be 2 degree of retroversion and the mean ICC was in moderate agreement (ICC-0.66) The mean ICC for inclination was found to be in almost perfect agreement (ICC-0.81) with the mean value found to be 9.4 degree of inferior tilt. The mean ICC for depth of reaming was found to be in substantial agreement (ICC-0.79) and the mean depth of reaming was found to be 7. 1mm.The mean ICC for rotation of the base plate was found to be in almost perfect agreement (ICC-0.96) and was done to a mean of 1.75 degree posteriorly. The length of central screw mean was found to be 33.5 mm and the ICC was found be in almost perfect agreement (ICC-0.85).The mean bone contact between the implant and glenoid was found to be extent of 91.38% after use of augments and most commonly a medium size augment was used.
Intra-Observer Reliability
The mean ICC was found to be almost perfect agreement in rotation of baseplate (ICC-0.976), reaming depth (ICC-0.892), inclination (ICC-0.846). It was found to be in substantial agreement with the initial positioning of mini baseplate (ICC-0.708 and 0.647 in super-inferior and antero-posterior planes respectively), version (ICC-0.647). Overall, the results indicate favorable reliability in both inter-observer and intra-observer assessments, suggesting consistent and reproducible outcomes in the positioning of the mini base plate and related parameters during shoulder arthroplasty procedures (Table 2).
Reverse Shoulder Arthroplasty (RSA) has become increasingly popular for addressing various shoulder pathologies due to its ability to restore function and alleviate pain with promising long-term outcomes and improving survivorship rates, RSA has become a preferred option for many patients. Central to the success of RSA is the accurate positioning of glenoid implants, which plays a critical role in achieving stability and longevity of the prosthesis. Glenosphere positioning plays a pivotal role in determining the outcomes of reverse shoulder arthroplasty (RSA), as it directly influences the center of rotation and biomechanical characteristics of the reconstructed joint. Mispositioning of the glenosphere can lead to various complications such as dislocation, scapular notching, decreased range of motion, and component loosening. Studies have highlighted the significance of accurate glenosphere placement to mitigate these risks [16,17]. Several factors contribute to the challenges of achieving optimal glenosphere positioning, including inaccurate assessment of pathologic anatomy, improper choice of implant, and execution errors during surgery. Verboort et al reported significant errors in glenosphere inclination and version when using standard instrumentation, emphasizing the need for improved techniques and technologies to enhance accuracy [18]. Preoperative advanced imaging, particularly Computed Tomography (CT) with three-dimensional (3D) reconstruction, has emerged as a valuable tool for understanding pathologic anatomy and facilitating precise planning.
Scalise et al demonstrated that 3D CT reconstructions improve inter-rater reliability among experienced shoulder surgeons, enabling better assessment of glenoid version, inclination, and bone loss [19]. The advent of 3D planning software has revolutionized preoperative planning for RSA by allowing virtual implantation and simulation of surgical procedures. Cadaveric studies have shown that such software can significantly reduce deviations in postoperative glenoid positioning from the planned parameters, ensuring greater accuracy and reproducibility [20,21]. In this study, we introduced a method for utilizing 3D planning software, specifically the Signature One planning system from Zimmer Biomet, to achieve consistent and optimal placement of glenoid components. By integrating principles aimed at maximizing bone preservation and stability, we developed a protocol that offers guidance to less experienced shoulder surgeons and new users of the planning software. Our study aimed to assess the reliability and efficacy of this protocol through intra- and inter-user variability analysis. The results of our study demonstrate promising findings regarding the reliability and consistency of our planning protocol. Through inter-observer and intra-observer reliability assessments, we observed moderate to almost perfect agreement in various parameters related to glenoid implant positioning, including super-inferior and antero-posterior placement, version, inclination, reaming depth, rotation of the baseplate, and screw length.
These findings suggest that our protocol can yield reproducible results across different surgeons and repeated assessments. Our protocol addresses several key aspects of glenoid implant placement, including adjusting the baseplate position to minimize notching and optimize stability, correcting anteversion/retroversion for optimal fit and screw length, setting inferior tilt to reduce sheer stress, mimicking surgical techniques for reaming depth, and fine-tuning augment selection for maximal bone contact. By incorporating these steps into the planning process, we aim to enhance the precision and predictability of glenoid implant placement, ultimately leading to improved surgical outcomes and patient satisfaction. One limitation of our study is the relatively small sample size, which may limit the generalizability of our findings. Future studies with larger cohorts are warranted to validate the effectiveness of our protocol across diverse patient populations and surgical settings. Additionally, long-term follow-up is needed to evaluate the clinical outcomes and survivorship of RSA procedures planned to use our protocol.
Standardized protocols for glenosphere positioning in RSA are critical for achieving optimal surgical outcomes and minimizing complications. Preoperative advanced imaging and 3D planning software offer valuable tools to enhance accuracy and precision in surgical planning, ultimately improving patient outcomes and satisfaction. Our study introduces a novel method for utilizing 3D planning software to achieve consistent and optimal placement of glenoid components in RSA. By providing a standardized protocol based on principles of bone preservation and stability, we aim to assist surgeons in improving surgical precision and enhancing patient outcomes. Further research is needed to validate the efficacy and long-term benefits of our protocol in clinical practice. Future research directions may include investigating the clinical impact of preoperative planning on range of motion, functional outcomes, and implant survival.


