Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Vladimir A Mikhaylov1*, D V Mikhailov2, V O Gladyshev3 and E A Sharandin3
Received: March 20, 2024; Published: April 01, 2024
*Corresponding author: Vladimir A Mikhaylov, Eternity Medicine Institute, Dubai, UAE
DOI: 10.26717/BJSTR.2024.55.008768
Since 1988, we have been using various types of laser radiation in dealing with different diseases. Generally, several types of laser radiation are used in the treatment program, where the ones corresponding to the near-IR (850-910 nm) and the red region (630-640 nm). For a series of publications revealing the use of intravenous laser blood irradiation, an international award was received (Ming Chien Kao Awards). The obtained results forced us to reconsider the existing views on the work of the cardiovascular and nervous systems. Was discovered the new principle of the cardiovascular systems development and structure.The main range (850 -910 nm) is used for the treatment of pathology of internal organs. Initially were used, a power of 5-10 watts per pulse and a time from 5 to 20 minutes. By now, the power has increased up to 100 watts per pulse and the irradiation time has become several hours. This made it possible to improve the results of treatment. Especially with regard to oncology. We have not found studies how this wave range penetrates and how it is dispersed by various tissues and internal organs. Therefore, we conducted an experimental study on pig tissues to examine these factors. The main purpose of the experiment were to determine the scattering and absorption capacity of the main tissues and organs - skin of various thicknesses, adipose tissue, muscle tissue, liver, heart, lung, kidneys, cardiac septum, bones (flat and tubular). Based on these obtained results was created a computer program. This program, using ultrasound and MRI data, allows us to determine what dose reaches the affected target. This takes into account which tissues and the distance the laser beam passes through. This allows to use of multiple lasers, conducting training at different angles. Without damaging normal tissues, the necessary dose is applied to obtain the maximum therapeutic effect.
High effectiveness of laser radiation in treating various diseases has been proved in 35 years of its application in medicine. One of the problematic issues in the treatment of internal diseases consists in the inability to determine the most effective dose to treat various lesions of internal organs. In this field of application, laser is used in a near-infrared radiation range due to the greatest penetration depth into the human body. During the entire period of laser therapy use, studies on penetrating and reflective ability of biological tissues were carried out at a limited wavelength range. The purpose in conducting this study was to gain insights and to experimentally determine the penetrating and reflective capacity of various tissues. The experiment was carried out with the use of laser radiation at the operating wavelength equal to 860 nm of the Mustang-2000 laser therapeutic device. The results obtained made it possible to calculate the dose of laser radiation suited to the organs at different depths from the surface of the body to absorb it. This solves one of the main problems of laser therapy, dose determination of laser radiation required to treat various diseases. Since 1988, we have been using various types of laser radiation in dealing with different diseases [1]. As a rule, several types of laser radiation are used in the treatment program, where the ones corresponding to the near-IR (850-910 nm) and the red region (630-640 nm) of the visible wavelength range [2-4] are most frequently exploited. When using the red range of laser radiation (630-640 nm), the mechanisms of its effect on tissue and blood have been fully studied. Indications and contraindications for the use of the method have been compiled [2,5].
Moreover, the accumulated vast practical experience has made it possible to reconsider the existing views on the functioning of cardiovascular and nervous systems [6-13]. The experimental inquiry resulted in the international Award in Medicine in 2016 [14]. Due to its high penetrating ability, the use of the near-infrared range (850-890 ppm) has made it possible to effectively treat the pathology of many internal organs [15-25]. Overall, we can confirm that the most interesting results were evident in cancerous diseases treatment. We have studied the mechanisms of the impact this type of radiation has on the oncological process, and it helped us to further work out the basic principles of using this wavelength in the treatment of cancer [26-30]. Experimental studies were conducted on several models of oncological tissues (Walker's carcinosarcoma and breast cancer in rats and spontaneous breast cancer in mice). Along with testing and studying the most effective doses of laser radiation and its combination with various groups of chemotherapy drugs, the possibility of combination with photodynamic therapy has been also approached [31-34]. The application of this method in clinical practice began in 1988. Initially, laser therapy was used prior to surgery [1]. Then it was implemented both as an independent method and in combination with radiation and chemotherapy [35-50]. The results got in the treatment for mastopathy proved to be most interesting [51].
One of the important practical outcomes of the study is differential choice of the absorbed dose for various organs according to the formula 1 :
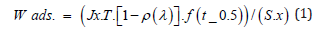
W- Absorbed dose of energy, ,
X - Depth of the target for irradiation, cm
Jx- Power of irradiation on the ‘X’ depth (W); determined according to special tables.
T – Exposure time, sec
ρ(λ)- Reflection coefficient (for skin approximately -0.38)
F - Pulse repetition frequency, Hz
t0.5 - Duration of laser impulse (70x 10-8 sec.).
S -Area of impact on the surface of biological tissue, cm.
1-ρ(λ)– since a mirror emitter was applied, it can be taken as 1
In synthesizing the data obtained, the most interesting results were evident in cancer treatment. The mechanisms of the effect this type of radiation has on oncological process were studied and the basic principles of using this wave range in the treatment of cancer have been formed [26-30]. During the research our team carried out experimental studies on several models (Walker's carcinosarcoma and mammary cancer in rats and spontaneous mammary cancer in mice) to examine and choose the most effective doses of laser radiation and its combination with various groups of chemotherapeutic drugs. We also approached the possibility of combination of the method with photodynamic [31-34]. The use of this method in clinical practice began in 1988. Initially, laser therapy was used prior to surgery [1]. It was then implemented both as an independent method and in combination with radiation and chemotherapy [35-50]. The results got in the treatment for mastopathy proved to be interesting [51]. We found the results of the treatment satisfactory. They demonstrated the high effectiveness of this type of radiation for the treatment of cancer in patients. Therefore, this absorbed dose calculation formula has been in use for quite a long period of time [52]. During accumulation of clinical experience and practical application of the method , it turned clear that this calculation method does not take many factors that affect the absorbed dose into account.
Such factors as blood supply to organs [53,54] and alveoli oxygenation were not considered. Compared to a power of 5-10 W per pulse and a time of 5 to 20 minutes used in 1988, current indicator for a power of up to 100 W per pulse is used and the irradiation time is several hours. These observations demonstrated the need for research to consider the spectral features of all tissues through which laser radiation passes and the dose which reaches the pathological focus.
Purpose and Objectives of the Study
The purpose of this study was to learn how various pig tissues and organs absorb and scatter laser radiation (860nm). According to their histological structure, they are most like human tissues. All the studies were carried out based on the Faculty of Basic Sciences at Bauman Moscow State Technical University. The objectives of the experiment were to determine the scattering and absorption capacity of the main tissues and organs - skin of various thicknesses, adipose tissue, muscle tissue, liver, heart, lung, kidneys, cardiac septum, bones (flat and tubular). It was necessary to create a special stand, which was supposed to consist of a laser diode of a certain wavelength (860nm), a device for fixing tissue through which laser radiation was supposed to pass, and a device for recording the radiation was to pass through the tissue. The results obtained after processing made it possible to calculate the reflective and absorptive capacity of various tissues.
Laser radiation of different wavelengths penetrates biological tissues differently. Experiments revealed that near-infrared range (IR) of wavelength has the most penetrating capacity (sure 1). During the experiment, we found out the following: when laser radiation passes through biological tissue, change in radiation intensity is observed, and further gets decomposed into three components - reflected, absorbed, and transmitted ones (Figure 2). Under normal incidence of a collimated laser beam along the z axis on biological tissue, because of reflection from its surface, scattering and absorption by tissue, a change in radiation intensity is observed in accordance with an exponential law,
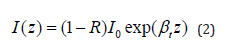
where :
I0- Intensity of the incoming irradiation on the tissue
R- Coefficient of Fresnel reflection at normal incidence
βt- Elimination (attenuation) coefficient
Elimination rate is the sum of absorption βa and dissipation βs coefficients.
Attenuation coefficient is equal to the sum of absorption βaaand scattering βs coefficients.

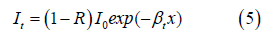
The link between the normally oriented intensity of irradiation is expresses as follows:

Where:
Ir= IrR Intensity of reflected radiation,
Ia –Change in intensity at propagation through a sample of biological tissue,
It - the intensity of radiation transmitted through the tissue.
For sample of tissue with the thickness x
Then , from equations (3) and (4) it follows.
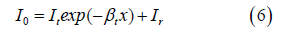
For two tissue samples we can write a system of equations
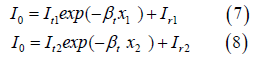
When measurements for two identical (Ir1=Ir2) tissue samples of different thicknesses are carried out, attenuation coefficient and reflection coefficient are found
Thus, the passage of laser radiation through biological tissue is characterized by significant scattering by inhomogeneities (in inhomogeneous media). The scattered radiation pattern usually has a uniform angular intensity distribution.
The choice of the working wavelength corresponds to the parameters of the pulse emitting head of the certified laser therapeutic device “Mustang 2000” (Company “Tekhnika”), the characteristics of this device were taken as input radiation parameters. All the work was done based on the Bauman Faculty of Basic Sciences on personal initiative (Head - Prof. Gladyshev V.O.) To carry out the research, a special stand was developed (Gladyshev V.O., Sharandin E.A.), which made it possible to calculate the incident and transmit radiation power.
The Stand Consisted of the Following Components
A. A photodetector with a wide dynamic range. An Avesta ASP-100MF spectrometer was used as a photodetector with a wide dynamic range.
B. A special device in which the materials being studied were recorded.
C. Laser diode (Figure 3).
Due to the rotating mechanism the stand allows for measuring the radiation patterns passed through the sample in the region from -90 to +90 degrees. Various pig tissues and organs were used for the research. Since they are like human ones in their structure and optical properties. The experimental material was obtained at stages 3-5 hours after killing the animal. To preserve the biological structure of the tissues as much as possible during transportation, a special medical container was used. All samples were brought to the same size (2x2cm) and thickness (0.1−1 cm). They were rigidly fixed in the device, which made it possible to minimize the change in the thickness of the tissue across the cross-section and its deformation during the measurement process. The following animal tissues were studied: pieces of skin of various thicknesses, adipose tissue, muscle tissue, liver, heart, lung, kidneys, cardiac septum, bones (flat and tubular). An example of organ fixation is shown in Figure 4. After this, the material was inserted into a special device and fixed rigidly (Figure 5). Laser radiation passed through the tissue and was recorded in a spectrometer (Figure 6). We used at least two samples of different thicknesses, which made it possible to determine absorption and reflection coefficients for axial radiation beams by using formulas (8) and (9). The radiation at the input to the photodetector is recorded in relative units of measurement. The results were monitored by measuring laser radiation intensity distribution through a reference matte plate with a scattering pattern close to the Lambert distribution.
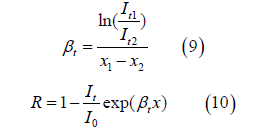
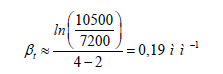
The results obtained were tabulated for further data processing and program development (Table 1).
Table 1: Results of measurements of the passage of laser radiation (at all angles of direction) through various tissues.
Tissue Absorption Coefficient Calculation
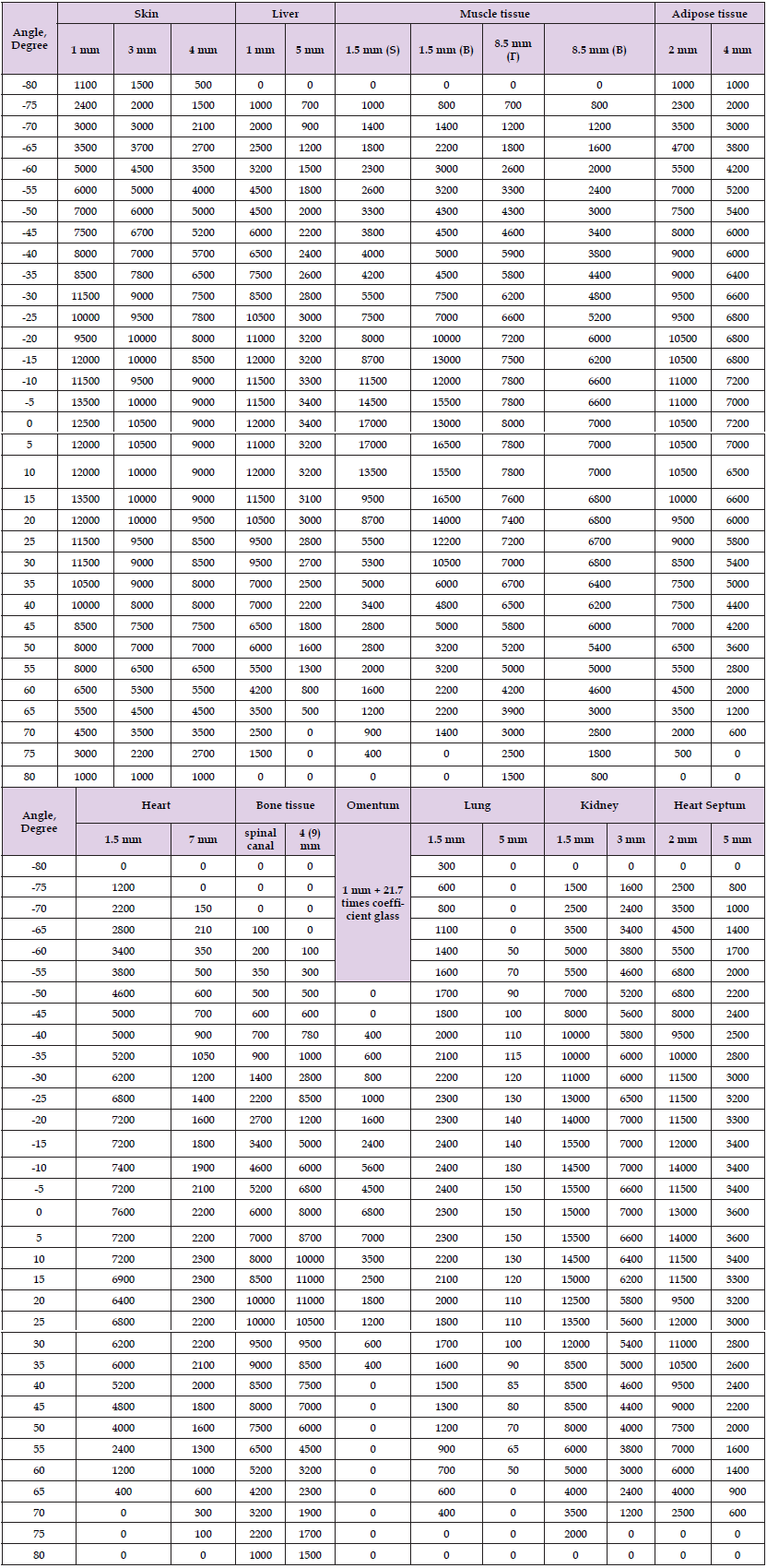
Calculation of Fat Absorption Coefficient: The results of the normal measurement of the radiation intensity through 2 and 4mm fat tissue and the estimated absorption coefficient are presented in Table 2. Substituting values in formulas (9) and (10), we get:
Absorption coefficient value for adipose tissue is 1 millimeter (for working wavelength, 860nm) Similarly, we calculate absorption coefficients for other tissues:
βt skin − 0.13 mm−1
βt liver − 0.23 mm−1
βt muscle tissue − 0.22 mm−1
βt fat − 0.19 mm−1
βt heart − 0.32 mm−1
βt bone tissue − 0.5 mm−1
βt lung − 0.79 mm−1
βt kidney − 0.53 mm−1
βt of the cardiac septum − 0.44 mm−1
Below are the maximum angular intensity distributions (scattering diagrams) of collimated laser radiation passed through tissue samples with a wavelength of 860 nm. The sample radiation directional data in the range of -90 to +90 degrees (Table 1) are used to draw laser dissipation diagrams for each type of tissue.
Skin Tissue
Skin tissue, pieces of various thicknesses (1 and 3 mm) were used for the study. Skin scatter diagram (Figure 7). The graph shows that the main radiation dose (more than 50%) falls on a wide angle of exposure (±50O..60O). It is very important to note the good transmittance of the skin (up to 80% or more) for this type of radiation.
Liver Tissue
Diagram of radiation scattering in liver tissue (Figure 8).
Muscle
Diagram of radiation scattering in muscle tissue (Figure 9).
Adipose Tissue
Diagram of radiation scattering in adipose tissue (Figure 10).
Heart Tissue
Diagram of radiation scattering in cardiac tissue (Figure 11).
Heart Septum Tissue
Scatter diagram of cardiac septum (Figure 12).
Bone Tissue of the Spinal Canal
Radiation scattering diagram in the spinal canal (Figure 13).
Bone
Diagram of radiation scattering in bone tissue (Figure 14).
Lung Tissue
Diagram of radiation scattering in lung tissue (Figure 15).
Kidney Tissue
Diagram of radiation scattering in kidney tissue (Figure 16).
The study allows us to calculate the radiation dose to obtain the necessary therapeutic effect in the affected organ. Knowing the reflectivity of radiation from the skin and the absorption coefficients of all tissue types under study, it became possible to calculate the radiation dose that a certain area should receive. For this purpose, a program that allows to calculate an algorithm for using laser therapy to treat various pathologies was compiled. The input parameters for calculating the program are:
1. Radiation power.
2. Power level.
3. Pulse frequency.
4. Irradiation time.
5. Radiation angle,
6. Thickness of fabrics.
The total energy exposureis calculated according to the formula:

Where:
P- radiation power (W),
τ- unit pulse duration (s),
t- Radiation exposure time (c),
S- laser impact area (cm2),
F- pulse frequency (Hz).
The laser impact area for the Mustang 2000 device is selected according to the parameters of the laser head beam, 5 mm in diameter. The formula provides for [11], finding out energy exposure at the output of the laser head. To obtain the final exposure, it is necessary to consider the radiation lost because of reflection and absorption in tissues. When carrying out calculations, radiation absorption was found for each layer independently. The number, type and thickness of each layer were specified as initial data. Loss of laser radiation energy due to reflection, with the assumption of similar refractive indices of different types of tissue, was calculated only for the first layer - skin. Processing of experimental data made it possible to establish that about 45% of the radiation is reflected from the skin tissue sample. Such a high value can be explained by a combination of the processes of both reflection and backscattering of radiation in the samples. The reflectance value directly depends on the degree of pigmentation and wrinkling of the skin, the presence of fat and moisture, and, most importantly, the wavelength of the emitter. According to the data given in [55-57], the reflectance of human skin in the IR range can vary from 10 to 55%. Calculation of the dose of radiation that has sequentially passed through various biological tissues may serve as an example. The formula for finding the total energy exposure of radiation with a wavelength of 850nm passing through skin, muscle and fat tissue is following:
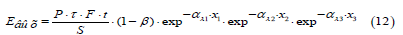
where α _λ1,α _λ 2 and α _λ3 are the absorption coefficients of skin, muscle and adipose tissue, respectively, and , and are thickness.
Considering the outcomes we may claim that the study made it possible to determine the radiation dose at different angles of incidence. Moreover, reflection and absorption parameters of all tissues studied have been determined. This made it possible to determine the total absorption dose of laser radiation at passing through all tissues from the surface of the skin to the pathological focus. Based on these results, a program was developed making it possible to determine the dose of laser radiation that the target organ and the tissues around receive. The program allows to calculate the total energy exposure of laser radiation passed through various types of biological tissues, starting from the skin and to the required irradiation zone (Figure 16). The program window for calculating the absorbed dose by the organs under study for a wave of 850mn (Figure. 17).
The program allows to calculate the total energy exposure of laser radiation passing through various types of biological tissues, starting from the skin and to the required irradiation zone (Figure 17).
Pig tissues were used as an experimental model. Of all experimental models available, pig tissues are most similar to human tissue. Analyzing the results obtained, it can be assumed that similar human tissues have similar absorption capacity. At least it proved possible to reliably estimate the radiation dose to various tissues and organs when exposed to laser radiation with a wavelength of 860 nm. For this purpose, a special program was created (Gladyshev V.O., Sharandin E.A.). It made it possible to calculate the absorbed dose based on the total absorption coefficient of the organs the laser beam is supposed to pass thought. Of course, the absorption capacity of the organs being studied differs from the normal state of the tissues of a living organism. In the samples studied, there was no sufficient volume of blood that could be found in the tissue of a living organism. At lungs testing, besides the absence of blood, there was no air in the alveoli and bronchi. Therefore, absorption and reflection coefficients in organs under study are, of course, different from living tissues. In further research, we are to consider the reflective and absorptive ability of all blood components for a wavelength of 860 nm. In those organs where blood volume was not considered, these coefficients should be approximately equal. In lungs such differences will be significant. Since blood supply and the volume of lungs filled with air were not considered, it is possible to calculate the absorbed dose in different segments of lungs only approximately. In organs such as bones, tendons, ligaments, where blood supply is lower than in parenchymal organs, these coefficients are almost equal.
It follows from what has been discussed that it was the first time the way different tissues influence the passage of laser radiation with a wavelength of 860 nm was approached in a study . Absorption coefficients and scattering diagrams have been experimentally worked out for major types of biological tissues. A program to determine the radiation dose most optimal to obtain the maximum effect in treatment for various pathologies of internal organs has been developed. The developed methodology will serve subsequent in-depth study of the effect IR radiation has on the human body and is going to be of good use for further improvement and development of laser therapy and laser medicine in general.


