Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Zuojun Cai1*, Patricio Mendoza Gálvez2, Gabriel Vargas Duarte3 and Karla Rubio Téllez4
Received: March 06, 2024; Published: March 20, 2024
*Corresponding author: Zuojun Cai, Pediatrics Resident, Multicenter Program of Medical Specialties ITESM-SSNL, Tecnológico de Monterrey, School of Medicine, and Health Sciences, México
DOI: 10.26717/BJSTR.2024.55.008737
Avoidant/Restrictive Food Intake Disorder (ARFID) is a recently recognized feeding disorder in the DSM-5. It involves the avoidance or restriction of food intake due to a lack of interest or aversion to certain or all foods, unrelated to body image perception or a desire to lose weight. This disorder can lead to significant weight loss and nutritional deficiency. We present the case of a 5-year-old male diagnosed with ARFID, intending to illustrate the diagnostic approach, offering gastrostomy as part of the multidisciplinary treatment. The patient had previously been diagnosed with autism spectrum disorder, meeting DSM-5 criteria. Referral from outpatient care to hospitalization occurred due to moderate dehydration and constitutional symptoms. Multidisciplinary assessment ruled out infectious, oncological, endocrine, gastrointestinal, and neurological pathologies. Gastrostomy was chosen as the nutritional intervention due to the patient’s absolute refusal to try any food, along with occupational therapy focusing on feeding. ARFID is a psychiatric disorder with a challenging diagnostic and therapeutic approach, requiring a multidisciplinary team and exclusion of organic pathologies before meeting DSM-5 criteria.
Keywords: ARFID; Feeding Disorder; Weight Loss; Restrictive Intake; Gastrostomy; Autism Spectrum Disorder
Avoidant/Restrictive Food Intake Disorder (ARFID) is a feeding disorder recently recognized in the DSM-5. It is characterized by the avoidance or restriction of food intake due to a lack of interest or aversion, unrelated to body image alteration or a desire to lose weight, leading to significant weight loss and nutritional deficiency. We present a case of a 5-year-old with ARFID admitted for moderate dehydration and significant weight loss. This review aims to present a multidisciplinary therapeutic approach to weight loss associated with this disorder.
A 5-year-old male, referred from the pediatric outpatient clinic, was hospitalized for moderate dehydration and constitutional symptoms. According to the mother, the child is the product of the fifth gestation, with a history of 2 previous cesarean sections and 2 miscarriages. Prenatal care was uneventful. The patient received exclusive breastfeeding for 3 months, followed by formula feeding. Introduction of solid foods started at 6 months, but the child showed reluctance to new foods, making integration into family meals challenging. Regular occupational therapy for the past 4 months aimed to expand food variety with minimal improvement. The patient’s diet mainly consisted of water, rice cakes, and vegetable chips. Neurodevelopmental milestones were achieved within expected timelines, except for partial toilet training at 4 years, currently using diapers during sleep. Motor and language development were appropriate for age. Allergies to amoxicillin-clavulanic acid were reported. The patient presented with general discomfort, lethargy, anorexia, and a significant weight loss of 12.3% over the last three weeks. Alterations in behavior, including lack of interaction with peers and increased food restriction, were noted. The physical examination revealed an ectomorphic phenotype, pale skin, bilateral sunken eyes, dry oral mucosa, decreased abdominal skin turgor, and a capillary refill of 3-4 seconds. Height was 113 cm (32nd percentile), weight was 17.1 kg (7th percentile), and BMI was 13.4 kg/m2 (2nd percentile).
Emergency blood glucose measured 47 mg/dl. Hospitalization included intravenous rehydration and a multidisciplinary approach: complete blood count, acute phase reactants, urinalysis, and chest X-ray showed no abnormalities, ruling out infectious causes. Oncological evaluation, including various tests, ruled out malignancy. Endocrinology monitored glucose levels and investigated hormonal imbalances, identifying central hypothyroidism secondary to malnutrition. Diabetes mellitus and adrenal insufficiency were excluded. Neurological evaluation, including MRI and EEG, revealed no abnormalities. Child abuse and other digestive disorders causing oral aversion were also ruled out. Considering the recent diagnosis of autism spectrum disorder and the patient’s selective oral intake, a neurodevelopmental evaluation integrated the diagnoses of autism spectrum disorder and ARFID, meeting DSM-5 criteria. Due to the patient’s nutritional status, gastrostomy placement was agreed upon to ensure feeding therapy, alongside occupational therapy focusing on feeding (Figure 1).
The diagnosis of Avoidant/Restrictive Food Intake Disorder (ARFID) is established in the DSM-5 in 2013. The diagnostic criteria for this syndrome are based on specific eating behaviors, specifically food selectivity, lack of appetite, and fear of feeding due to aversive consequences (more common with 36.92%, as reported in the analysis by Medina-Tepal et al) [1,2]. The patient exhibits food selectivity with a preference for crunchy textures, persistent anorexia despite occupational treatment focusing on introducing new foods, and rejection of the same. Medina-Tepal et al, through a literature review analyzing 41 articles following PRISMA and CARE guidelines, find that this syndrome is more frequent in males, with 53.85% in the 10 to 13 age group and 29.23%, but it’s noteworthy that 15.38% of cases analyzed were in the age range of 20 to 56 years [2]. The etiology remains unknown and is currently under study. A multifactorial origin is proposed, involving biological, psychological, and environmental factors [3]. Biological factors include hormonal and appetite-regulating peptide alterations, prematurity, and taste sensory disturbances. In the present case, sensory alterations became evident, such as reporting dysgeusia (a metallic taste in food) and rejecting milk upon discovering that his mother administered medications in it. Psychological factors include affective alterations and traumatic events during development, while environmental factors encompass lack of exposure to certain flavors and textures, forced feeding, or lack of exposure to new foods. Diagnosis of this pathology should be done carefully, ruling out organic pathologies before integrating elements recently established in DSM-5. Katzman et al, in a study with Canadian pediatricians, found that about 63% of specialists in their pilot study were unfamiliar with ARFID.
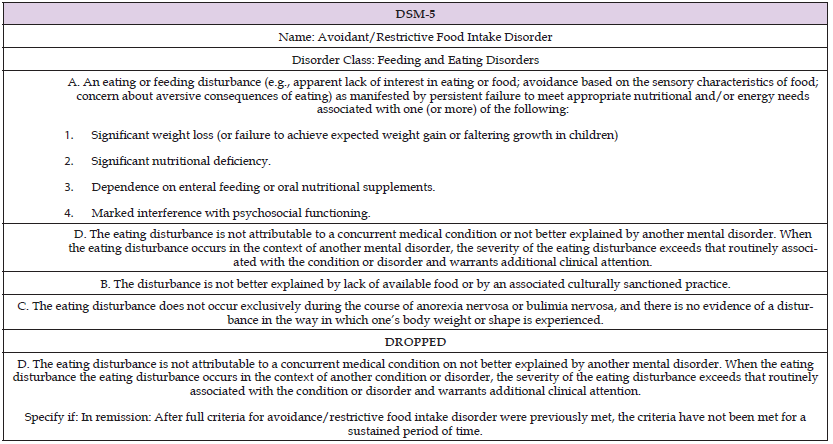
Diagnosis relies on clinical questioning (obtaining a thorough dietary history), DSM-5 criteria (Appendix Table 1), and suggestive signs and symptoms. The Eating Disturbances in Youth-Questionnaire (EDY-Q) is a useful diagnostic tool consisting of 12 questions and can be a simple tool for physicians less familiar with ARFID [4]. Regarding laboratory studies, blood analyses are particularly useful to assess the characteristics and degree of malnutrition, especially to review deficiencies in vitamins and minerals. ARFID is also associated with various psychiatric pathologies. Medina-Tepal et al report that in 26.15% of cases, no primary psychiatric disorder was reported in patients diagnosed with ARFID. However, some patients reported the presence of two or more disorders in addition to ARFID, with anxiety disorders being the most common at 38.46%. Selective eating, specifically in terms of type, texture, or presentation, is the most common eating disorder in patients with autism spectrum disorder (ASD). This could be one of the first symptoms manifested in undiagnosed children with ASD. These patients may also reject foods, exhibit disruptive eating behaviors, and prefer unhealthy foods (as seen in our patient’s food repertoire) or inadequate portions. Fruits and vegetables are generally rejected by most patients. De Toro et al suggest that, although its prevalence is not precisely known, previous studies suggest that 46- 89% of children with ASD present atypical eating habits [1]. Norris et al mention that most patients diagnosed with ARFID experienced significant weight loss or a deficit in adequate weight gain. Avoidance of foods due to their texture or smell, or a general aversion to food, were the most frequently reported eating symptoms.
Appendix Table 1: Diagnostic criteria for Avoidant/Restrictive Food Intake Disorder (ARFID) according to DSM-5. (9).
Lack of appetite and total food rejection were also commonly mentioned symptoms. Other reported symptoms include abdominal pain, fear of vomiting, anxiety when eating, complaints of satiety, nausea, and unpleasant sensory experiences when eating [5]. In the present case, the patient experienced dysgeusia and unpleasant experiences with food intake upon discovering that his parents used them to administer medications, as mentioned earlier. Regarding treatment, Medina-Tepal et al establish that hospitalization is the most common treatment modality at 46.34%, followed by outpatient treatment at 41.46%. Therapeutic conductive therapy is essential in management and mainly focuses on reducing restrictive eating practices, selective eating, and recovering associated signs and symptoms such as low weight. On the other hand, Family Therapy aims to motivate and empower family members to support the patient’s recovery using different strategies. Among the most used medications are antipsychotics, primarily olanzapine [1].
In the present case, cognitive-behavioral therapy was implemented for a period of 3 months before the episode that led to the hospital admission. A total of 16 sessions were conducted with the aim of introducing foods and addressing issues related to their selection and refusal to ingest unselected textures. Despite efforts in therapy, no significant improvements in intake were observed, leading to a critical state of malnutrition. This was evidenced by clinical signs such as sunken eyes, dry skin, positive skin turgor with a dry fold, and dry mucosa. Additionally, frequent and severe episodes of hypoglycemia were documented during hospitalization. Given the described circumstances, the indication for gastrostomy became indispensable in the treatment. Gastrostomy provides a safe and stable route for administering necessary nutrition, preventing the patient’s selective denial of food. This intervention will allow the patient to receive essential nutrients to improve his nutritional status and address the deficiencies that have led to malnutrition. It is important to emphasize that the decision to perform a gastrostomy has been made after carefully considering all available options and evaluating the associated risks and benefits. The lack of response to cognitive-behavioral therapy and the urgent need to address malnutrition and its negative consequences for the patient’s health have been considered [7-9].
ARFID is a psychiatric disorder challenging to diagnose and manage, requiring a multidisciplinary approach and reliance on new diagnostic tools. Comprehensive patient care, education, and family support are essential.
The authors thank the patient’s family for their cooperation, the nursing and medical teams involved in the patient’s care, and the institutions supporting this study.
The authors declare no conflict of interest.
This study received no external funding.
Ethical approval was obtained from the Institutional Review Board at Tecnológico de Monterrey, School of Medicine and Health Sciences.
Informed consent was obtained from the patient’s legal guardians.


