Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Matteo Maria Cati*
Received: March 12, 2024; Published: March 20, 2024
*Corresponding author: Matteo Maria Cati, University of Bologna 2 Scaravilli Square 40126 Bologna, Italy
DOI: 10.26717/BJSTR.2024.55.008735
This article introduces the Comprehensive Efficiency Index (CEI) as a tool for assessing and improving hospital performance across various domains. The CEI offers a holistic approach by integrating indicators of productivity, quality of care, economic efficiency, and patient satisfaction. Through targeted analysis and strategic interventions guided by the CEI, hospitals can optimize resource utilization, enhance patient outcomes, and deliver high-quality care. Additionally, the integration of clinical governance principles ensures alignment with clinical standards and patient safety, while project management methodologies facilitate efficient implementation of improvement initiatives. Moreover, risk management practices are essential in identifying and mitigating potential threats to hospital operations and patient care quality. By incorporating risk management strategies, hospitals can proactively address challenges and enhance organizational resilience. By incorporating clinical governance, project management, and risk management principles, hospitals can achieve comprehensive performance enhancement and sustainable efficiency gains.
Keywords: Efficiency Index; Quality of Care; Economic Efficiency; Patient Satisfaction; Project Management; Risk Management
In today’s rapidly evolving healthcare landscape, hospitals face unprecedented challenges exacerbated by the global COVID-19 pandemic. The pandemic has underscored the critical importance of efficient resource allocation, resilient healthcare systems, and patient- centered care delivery. As hospitals navigate the complexities of the post-COVID era, there is an urgent need for innovative approaches to assess and enhance hospital performance while ensuring the highest standards of patient care and safety. Against this backdrop, this article introduces the Comprehensive Efficiency Index (CEI) as a strategic tool for evaluating and improving hospital performance [1,2] in the post-COVID era. The CEI offers a multidimensional approach by integrating key performance indicators from diverse domains, providing stakeholders with a comprehensive view of hospital operations and identifying areas for improvement. The post-COVID era presents unique challenges and opportunities for hospitals worldwide. The pandemic has highlighted the importance of agility, resilience, and adaptability in healthcare delivery. Hospitals must navigate shifting patient needs, evolving regulatory requirements, and emerging healthcare trends while maintaining operational efficiency [3,4] and clinical excellence. At its core, the CEI framework encompasses indicators [5-7] related to productivity, quality of care, economic efficiency, and patient satisfaction.
By synthesizing data from these domains, the CEI enables hospitals to identify strengths, pinpoint areas of inefficiency, and prioritize improvement efforts based on evidence-based insights. Moreover, the integration of clinical governance principles ensures alignment with clinical standards and patient safety, fostering a culture of continuous quality improvement. By adhering to established clinical guidelines and best practices, hospitals can enhance patient outcomes and mitigate risks associated with clinical care. Furthermore, project management methodologies play a crucial role in the successful implementation of improvement initiatives guided by the CEI. Through effective project planning, execution, and monitoring, hospitals can ensure that improvement efforts are carried out efficiently and yield measurable results. Additionally, risk management practices are essential in identifying potential threats to hospital operations and patient care quality. By proactively assessing risks and implementing mitigation strategies, hospitals can enhance organizational resilience and safeguard against adverse events in the dynamic post-COVID environment. In summary, the CEI approach offers a strategic framework for hospitals to optimize performance, enhance patient care delivery, and achieve sustainable efficiency gains in the post-COVID era. By incorporating clinical governance, project management, and risk management principles, hospitals can navigate the complexities of healthcare delivery and deliver superior outcomes for patients and stakeholders alike, even in the face of unprecedented challenges.
This study proposes the Comprehensive Efficiency Index (CEI) as a novel tool for assessing and enhancing hospital performance across various domains. The CEI incorporates indicators informed by a comprehensive literature review [8-10] and intuitively chosen for their relevance to key aspects of hospital operations. The literature review encompassed academic publications, industry reports, and best practices guidelines to identify [11,12]
• Commonly used Hospital Performance Indicators: We
analyzed studies investigating hospital efficiency measurement,
such as the ones related to the Italian National Health System [13-
18] and identified frequently employed indicators across various
domains.
• Relationships Between Indicators and Performance: We
reviewed literature exploring the impact of specific indicators on
overall hospital performance and patient outcomes.
• Indicator Weighting Approaches: We examined different
methodologies for assigning weights to indicators, considering
their relative importance and potential trade-offs.
Based on the findings from the literature review and intuitive understanding
of crucial performance aspects, we selected a set of core
indicators for each domain:
• Productivity: We chose indicators like number of patients
treated, surgeries performed, and bed occupancy rate, aligning
with findings that these reflect efficient resource utilization and
care delivery.
• Quality of Care: Indicators like mortality rate, infection
rate, and complication rate were included based on their established
link to patient safety and clinical quality.
• Economic Efficiency: Cost per patient, profit margin, and
average length of stay were selected as they capture financial performance
and resource utilization, as supported by the reviewed
literature.
• Patient Satisfaction: Patient satisfaction scores, number of
complaints, and waiting times for outpatient visits were chosen
based on their documented association with patient experience
and overall satisfaction.
While relying solely on literature [19-21] may not encompass all relevant aspects, it provided a strong foundation for indicator selection. Additionally, intuitive understanding further refined the chosen indicators to ensure they address real-world hospital priorities. Following indicator selection, we proceeded with the following steps:
1) Weighting: Weights were assigned to each indicator based
on their relative importance, informed by the literature review
and further adjusted based on expert consultation or internal
hospital priorities.
2) Data Collection: Hypothetical data for Hospital H was created
within industry averages and typical ranges for each indicator,
serving as a test case for demonstrating the CEI’s application.
3) Index Calculation: The CEI was calculated for Hospital H
using the defined formula and the assigned weights for each indicator.
4) Benchmarking: Benchmark values for individual indicators
and the overall CEI score were established based on industry
standards, national quality databases, and performance data from
peer hospitals.
5) Improvement Strategies: Areas for improvement were
identified by comparing Hospital H’s performance against the established
benchmarks, leading to the proposal of targeted interventions.
6) Evaluation: The effectiveness of the CEI and proposed interventions
was evaluated by simulating improvement in designated
areas and observing the subsequent change in the CEI score.
This methodology combines the strengths of a literature-based approach with intuitive understanding to create a robust and relevant set of indicators for the CEI. While further research is needed to refine the methodology and assess its effectiveness in diverse settings (the Italian scenario was first considered [22-27], this initial study demonstrates the potential of the CEI as a valuable tool for hospital performance improvement.
A systematic search was conducted across major healthcare databases including PubMed and Scopus, as well as Google Scholar Search to identify relevant studies on hospital performance measurement. The search strategy included a combination of keywords such as “hospital”, “performance”, “measurement”, “performance matrix”, “composite indicator”, “index”, “benchmark”, and “efficiency”.
Inclusion criteria comprised of:
• Peer-reviewed articles published over the past 10 years;
• Articles focusing on multi-domain hospital performance indicators;
• Studies involving development or validation of composite
performance indices/metrics.
The search yielded 194 articles, which were screened for eligibility
based on full text review. Over 31 highly relevant articles were
selected for in-depth review and analysis based on the inclusion criteria.
The benchmark CEI score and targets for individual metrics were established through analysis of Italian national databases and publications focused on hospital performance measurement, including:
• Standards and clinical benchmarks from the Italian Ministry
of Health (Ministero della Salute) as well as Italian regions’
healthcare agencies.
• Datasets from the Italian National Outcomes Program (Programma
Nazionale Esiti - PNE) by the National Agency for Regional
Healthcare Services (AGENAS).
• Recent academic publications benchmarking hospital performance
across Italian regions.
• Best performer data quantifying metrics for top-ranked Italian
hospitals recognized for excellence in healthcare delivery on
composite indices.
This localization of data sources, benchmarks and analytical adjustment helps ensure the CEI score interpretations and subsequent improvement priorities resonate with Italian hospitals’ operational contexts and quality improvement maturity. The benchmarks can be periodically refined through inclusion of newer national datasets.
The CEI serves as a weighted composite measure, integrating
indicators [28-30] across four key domains: productivity, quality of
care, economic efficiency, and patient satisfaction. Each indicator is
assigned a weight reflecting its relative importance to hospital performance.
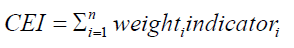
The formula for calculating the CEI is as follows:
By using the CEI, stakeholders can gain a complete picture of hospital efficiency and performance. This allows them to pinpoint strengths, target areas needing improvement, and monitor progress towards those goals.
1) Identify Areas of Improvement
Analyze the components of the CEI to identify areas where the
hospital’s performance falls below established benchmarks or industry
standards (such as for the emergency departments [31].
Focus on indicators with lower scores or significant deviations
from the benchmarks.
2) Develop Targeted Improvement Strategies
Based on the identified areas of improvement, develop targeted
improvement strategies and action plans. Engage key stakeholders,
including healthcare providers, administrators, and patients,
in the planning process to ensure buy-in and alignment with organizational
goals.
3) Implement Evidence-Based Interventions
Implement evidence-based interventions and best practices to
address the identified areas of improvement. This may include
process optimization, workflow redesign, staff training, and technology
adoption to enhance efficiency, quality, and patient satisfaction.
4) Monitor Progress and Adjust Strategies
Continuously monitor performance metrics and track progress
towards improvement goals. Use real-time data and feedback
mechanisms to assess the effectiveness of implemented interventions
and make adjustments as needed to ensure desired outcomes
are achieved.
5) Benchmarks for Individual Areas
Establishing benchmarks for individual areas within the CEI
framework allows hospitals to set realistic targets and guide improvement
efforts effectively.
For example:
a) Productivity: Compare patient throughput, surgeries performed,
and bed occupancy rates against industry benchmarks or
standards.
b) Quality of Care: Evaluate mortality rates, infection rates,
and complication rates against established benchmarks such as
national quality standards.
c) Economic Efficiency: Assess cost per patient, profit margins,
and average length of stay against financial benchmarks derived
from peer hospitals or industry averages.
d) Patient Satisfaction: Measure patient satisfaction scores,
number of complaints, and waiting times for outpatient visits
against benchmarks set by patient satisfaction surveys or leading
hospitals known for exceptional patient experience.
Example: Hospital H
Consider Hospital H, a large urban hospital, with the following hypothetical data:
- Productivity: 12,000 patients treated annually
- Quality of Care:
- Mortality rate of 1.8%
- Infection rate of 2.2%
- Complication rate of 2.5%
- Economic Efficiency:
- Cost per patient of $1,400
- Profit margin of 7%
- Average length of stay of 5 days
- Patient Satisfaction:
- Overall satisfaction score of 82%
- 25 patient complaints annually
- Waiting time for outpatient visits of 60 minutes
Using the CEI framework, Hospital H can systematically identify areas for improvement, develop targeted strategies, and monitor progress towards achieving its performance goals.
CEI Calculation for Hospital H
Assuming that the weights assigned to each indicator are the following:
Productivity: weight1 = 0.3
- Quality of Care: weight2 = 0.25
- Economic Efficiency: weight3 = 0.2
- Patient Satisfaction: weight4 = 0.25
We can calculate the CEI for Hospital H using the provided data
and the CEI formula:
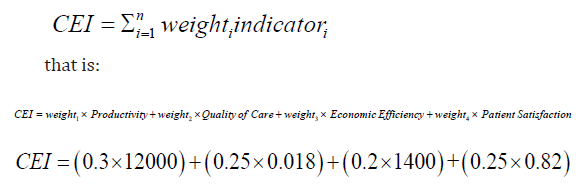
For Hospital H, the benchmark CEI could be established based on industry standards or the performance of peer hospitals with similar characteristics. Let’s assume the benchmark CEI for Hospital H is 4000. By comparing the calculated CEI (3880.209) with the benchmark (4000), Hospital H can identify areas where it falls short and focus its improvement efforts accordingly. In the example of Hospital H, potential areas of improvement can be identified by examining the components of the Comprehensive Efficiency Index (CEI) and comparing them to the assumed benchmark. Here are some areas where Hospital H may focus its improvement efforts:
1) Productivity
• Increasing the number of patients treated annually from
12,000 to meet or exceed industry standards.
• Optimizing resource allocation and scheduling to enhance
patient throughput without compromising quality of care.
2) Quality of Care
• Addressing the relatively high mortality rate (1.8%) by implementing
evidence-based clinical protocols, enhancing staff
training, and improving coordination among healthcare teams.
• Implementing infection control measures to reduce the infection
rate (2.2%) and complication rate (2.5%) to meet or exceed
national quality standards.
3) Economic Efficiency
• Identifying opportunities to reduce the cost per patient
($1,400) through strategic procurement, resource utilization, and
operational efficiency initiatives.
• Exploring revenue enhancement strategies and cost-saving
measures to improve the profit margin (7%) and financial sustainability.
4) Patient Satisfaction
• Addressing patient complaints (25 annually) by improving
communication, responsiveness to patient needs, and overall care
experience.
• Reducing waiting times for outpatient visits (60 minutes)
through streamlined processes, appointment scheduling optimization,
and utilization of technology for patient access.
By focusing on these areas of improvement, Hospital H can enhance its overall efficiency, quality of care, financial performance, and patient satisfaction levels. Continuous monitoring, evaluation, and adjustment of improvement strategies will be essential to sustain progress and achieve desired outcomes in alignment with industry benchmarks and best practices.
The Comprehensive Efficiency Index (CEI) enables quantitative evaluation of hospital efficiency for clinical governance. Targeted projects can address underperformance revealed by CEI trends. The following graph 1 (see Appendix for the Python code) has been obtained generating randomly hypothetical data on the trend of the CEI index in the years 2021 – 2024. The CEI dip in 2021 indicates worsening performance, triggering root cause analysis by hospital leadership. A Focused Improvement Project is launched to address high infection rates contributing to the CEI decline. The cross-functional team designs targeted interventions leveraging PDSA (Plan-Do- Study-Act) rapid improvement cycles:
- Plan - Hypothesis that increased hand hygiene compliance
will reduce infection rates
- Do - Implement hand hygiene monitoring pilot in one unit
- Study - Collect infection rate data to determine pilot efficacy
- Act - Expand pilot or reassess based on evidence
Appendix
The Python Code for the paragraph Demonstrating CEI - driven Performance Improvement is the following:
Multiple ideas like enhanced disinfection protocols and isolation procedures are tested via PDSA sprints to drive gains. Progress is monitored through CEI trends, which recover to benchmarks by 2023 - showcasing effectiveness of the CEI-linked governance and structured project approach. In summary, CEI data-driven governance combined with rapid-iteration project implementation enables hospital ecosystem enhancement.
The CEI offers a comprehensive and objective approach to assessing hospital performance and guiding improvement efforts. By leveraging the CEI framework and establishing benchmarks for individual areas, hospitals can identify strengths, pinpoint areas for improvement, and implement evidence-based interventions to optimize performance and enhance patient care delivery.
Further research is needed to refine the CEI methodology, explore its applicability across diverse healthcare settings, and investigate its correlation with other measures of hospital performance. By advancing the CEI framework, researchers and healthcare professionals can contribute to ongoing efforts to enhance hospital efficiency and quality of care. While this article introduces the foundational CEI methodology and an illustrative example application, further research should evaluate its utility through pilot testing in real hospital environments across diverse settings. By partnering with hospitals to collect performance data and implement the CEI in practice, future studies can validate its feasibility, refine parameter weightings based on field insights, and quantify the impact on improvement outcomes - establishing an evidence base for broader adoption. Specifically, the CEI methodology developed here can be pilot tested by collaborating hospitals through initial small-scale implementation focused on a limited performance domain or department. Researchers can provide analytical support while hospital quality teams manage the application, allowing rigorous joint evaluation. Establishing such academia-practice partnerships can accelerate practical enhancement and testing of the CEI, unlocking its full, evidence-backed potential to drive hospital transformations through data-driven improvements.


