Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Augustine Anyochukwu Onyeaghala1* and Mary Alaba Aderibigbe2,3
Received: January 11, 2024; Published: February 07, 2024
*Corresponding author: Augustine Onyeaghala, Department of Medical Laboratory Science, College of Basic Medical Sciences, Chrisland University, Abeokuta, Ogun State Nigeria
DOI: 10.26717/BJSTR.2024.54.008622
Background: Indiscriminate use of herbal products is a common practice in Nigeria, with commercial motor park workers being major consumers. Unfortunately, there is a dearth of reports on the use of predictive markers to track kidney and liver injuries in this population. This study aimed to determine the prevalence of kidney and liver toxicity among commercial motor park workers consuming herbal medicine using predictive markers of kidney and liver damage.
Methods: A cross-sectional study was conducted on 122 motor park workers aged 25-65 years. A prevalidated questionnaire was used to collect bio-data and history on the use of herbal medicine. Venous blood was collected from each participant into a heparin bottle. Plasma was used for initial screening and further testing. Subjects with plasma creatinine and liver enzymes higher than the reference values were excluded from further testing using predictive markers. KIM-1 and αGST were measured in 99 and 57 subjects, respectively. Statistical Package for Social Sciences software version 21.0 compatible software was used to analyze the data.
Results: A total of 91 (91.9%) respondents reported using herbal medicine, with 25 (27.5%), 18 (19.8%), and 48 (52.7%) reporting use for 1-5 years, 5-10 years, and more than 10 years, respectively. Prevalence of kidney (64.6%) and liver (64.9%) toxicities were high among the studied population. However, there was no significant association between KIM-1, αGST, and duration of use of herbal medicine. Subjects who consumed herbal medicine for more than 10 years had higher levels of KIM-1 (52.7%) and αGST (50%) than those in other groups. There was a significant difference between the mean values of KIM-1 and creatinine (P=0.000) and between the mean values of αGST and ALP, AST, and ALT (P=0.000). There was no significant correlation between KIM-1 and creatinine (P>0.05) or αGST and ALP, AST, and ALT (P>0.05).
Conclusion: This study showed a high prevalence of kidney and liver toxicities among commercial motor park workers who use herbal medicine. However, there was no significant association between the use of herbal medicine and kidney and liver toxicities. It is necessary to implement appropriate measures to curb the epidemics of kidney and liver damage in Nigeria. This study highlights the importance of using predictive markers in tracking kidney and liver injuries in populations that use herbal medicine.
Keywords: Herbal Medicine; Organ Dysfunction; Herbal-Based Products; Predictive Makers; Motor Park Workers
Abbreviations: CR: Plasma Creatinine; ALT: Alanine Transaminase; AST: Aspartate Transaminase; α-GST Alpha Glutathione Transferase; ELISA; Kidney Injury Molecule by Enzyme Linked Immunosorbentassay; HPR: Horseradish Peroxidase; NAFDAC: National Agency for Food, Drug Administration and Control; NGAL: Neutrophil Gelatinase-Associated Lipocalin; KIM: Kidney Injury Molecule
Herbal medicine, also known as botanical medicine or phytomedicine, is a type of healthcare that utilizes medicinal plants or plant extracts to prevent or treat diseases [1]. It is the oldest form of healthcare known to humans and has been used by all cultures throughout history [2,3]. Herbal medicine products can contain aerial or underground parts of plants, fresh juices, gums, fixed oils, essential oils, resins, and dry powders of herbs - leaves, bark, roots, rhizomes or other plant parts, either in the crude state or as plant preparations. Many of the drugs currently available to physicians have a long history of use as herbal remedies [4,5]. The World Health Organization estimates that 80 percent of the population of some Asian and African countries use herbal medicine for some aspect of primary healthcare [6]. Herbal medicine can be taken in various forms, but the most common one is in the form of liquid that is drunk either as herbal tea or diluted plant extract. The recent resurgence of public interest in herbal remedies has been attributed to several factors, including the preference of consumers to natural therapies, high cost and side effects of most modern drugs, and improvements in the quality, efficacy, drug reactions associated with the use of orthodox drugs, dissatisfaction with attitude of Physicians and safety of herbal medicines with improved development using science and technology [3,7].
Herbal medicine is widely used globally, especially in rural areas where access to modern medicine is limited. The benefits of herbal medicine include accessibility, low cost, and a desire for natural remedies. However, certain concerns on the use of herbal-based products have been raised and these include- presence of multiple plant constituents which can interact negatively with each other and with the body, lack of disclosure and documentation when using herbal remedies with conventional drugs, insidious toxic effects, dosage concerns, and quality and standardization issues [1,7]. Regulation of herbal remedies differs from country to country. In the United States, herbs and botanicals are classified as dietary supplements and do not require approval from the FDA before they are sold [7,8]. In Canada, herbal medicines are regulated as drugs, and the same standards required for the regulations of investigational products apply, including labeling and other requirements as set out in the Food and Drugs Act and Regulations [9].
In Nigeria, regulation of herbal medicine is the responsibility of the National Agency for Food, Drug Administration and Control (NAFDAC). NAFDAC grants listing registration status and full registration status, with the latter requiring clinical trials to evaluate safety and efficacy [8]. A duly registered herbal medicine is one in which the therapeutic/medicinal claims have been evaluated by NAFDAC while listed herbal medicines are those whose therapeutic/medicinal claims have not been evaluated using clinical trials. The motor-park industry is an essential component of Nigeria's transportation system, providing employment for thousands of people across the country. Sale of unregulated herbal products within motor parks is a regular practice in Nigeria and consumption of herbal-based products is a common practice among motor park workers. Many motor-park workers use herbal-based products as remedies for various ailments and health conditions. These products are often obtained from traditional healers and vendors, and their composition is largely unknown. Currently, there are no regulation prohibiting uncontrolled sale of herbal-based products across motor parks in Nigeria. Consumption of poorly evaluated herbal products among commercial motor park workers has been a public health issue. Several studies have reported heavy metal and toxin contamination in herbal-based products marketed in Nigeria.
A study by Iwegbue [10] reported elevated levels of heavy metals, such as lead, cadmium, and mercury in some herbal-based products sold in Nigeria. Similarly, a study by Ibitoye [11] reported high levels of aflatoxins in some herbal-based products consumed in Nigeria. These studies highlight the potential health risks associated with the consumption of unvalidated herbal-based products sold in Nigeria. Herbal-based products contain several nephrotoxic and hepatotoxic agents that can lead to renal and hepatic injuries. For instance, a study by (Anim, et al. [9]) reported that some herbal-based products contained aristolochic acid, a potent nephrotoxin associated with kidney injuries. Similarly, a study by Birgit [12] reported that several herbal-based products contained pyrrolizidine alkaloids, which are hepatotoxic and are associated with liver injuries. The liver filters toxins and waste products from the blood, while the kidneys help regulate fluid balance and remove waste products from the body. When these organs are damaged, the body's ability to remove toxins and waste products is compromised, leading to various health problems which might include mortality in some cases. Liver and kidney injuries are a significant health concern globally, and the prevalence of these conditions is on the rise [13]. In Nigeria, liver and kidney diseases are becoming more common, with herbal-based products consumption being a major contributing factor [13].
The use of herbal-based products for medicinal purposes is a common practice in Nigeria, and many people believe that these products have little or no side effects. However, many herbal-based products have been shown to contain toxic substances that could damage the liver and kidneys [9,12]. Kidney and liver injuries are significant health issues that can lead to severe morbidity and mortality. These disorders have been reported to affect a large proportion of individuals worldwide [13]. These conditions can be caused by various factors such as infections, drugs, toxins, and metabolic disorders. Early detection and diagnosis of kidney and liver injuries are critical in improving patient’s outcome and preventing complications. Traditionally, serum creatinine, bilirubin and liver enzymes have been used as biomarkers for the detection of kidney and liver injuries respectively. However, these biomarkers have limitations in predicting kidney and liver disorders as they are more diagnostic and prognostic in application. Application of the biomarkers may not be able to detect subtle changes in kidney or liver functions especially among individuals who are at the sub-clinical level of liver and kidney disorders. A study has shown that over 34.6 million Nigerians have been reported to be suffering silently of one form of renal disease or the other [14].
Arodiwe and colleagues [14] reported that of over 22.8% mortality documented in Enugu, South East Nigeria, from 1995-2010, Kidney and liver diseases accounted for 12.3 and 7.0 % of the reported mortality respectively [14]. Most patients with kidney and liver diseases are asymptomatic, thus regular screening becomes essential. Increased mortality associated with kidney and liver diseases have been linked to poor predictive nature of current tests in use for the detection of these diseases [14]. Evaluation and domestication of many predictive markers of liver and kidney diseases could go a long way in predicting diseases on time, initiating appropriate intervention(s), treatment and management thereby improving prognosis and reducing mortality. Predictive biomarkers have emerged as a promising tool for identifying individuals who are at risk of developing kidney and liver injuries. These biomolecules can help predict to high precision individuals who are at risk of developing renal and liver diseases especially in the future.
In recent years, numerous predictive markers have been discovered, evaluated and deployed for testing to identify individuals who are likely at risk of developing liver and kidney diseases. These biomarkers include Neutrophil Gelatinase-Associated Lipocalin (NGAL), alpha-glutathione transferase (αGST), liver-type fatty acid-binding protein (L-FABP), and kidney injury molecule-1 (KIM-1). The evaluation of these predictive markers has shown promising results in the early detection and prognosis of kidney and liver injuries [15-19]. In Ado-Ekiti, the capital city of Ekiti State, Nigeria, motor-park workers frequently consume herbal-based products for various ailments, but assessment of kidney and liver function among this population using predictive markers is deplete. Premised on this, the study is aimed to evaluate Kidney Injury Molecule-1 (KIM-1) and Alpha Glutathione Transferase (αGST) as predictors of kidney and liver diseases among selected motor park workers consuming herbal-based products. The study will explore the association between predictive markers of liver and kidney injuries and the consumption of herbal-based products among the selected population. With reported rising trends in kidney and liver diseases [13-14] coupled with limited health systems and capacity to manage any epidemic from kidney and liver diseases within the country, the need to generate evidence-based data which will help to curtail the trend becomes imperative. The finding from this study will possibly provide evidence-based data which could help formulate policies on the sale of herbal-based products in motor parks across Nigeria and institute regulation to protect the health of this significant economic sector in Nigeria economy.
Study Design
This was a cross sectional study.
Study Population
All the motor parks within Ado Ekiti metropolis were identified and stratified. A total of 122 motor park workers who met the inclusion criteria were then randomly selected within the stratified groups.
Inclusion Criteria
• Commercial motor park workers who consume herbal-based medicine.
• Age from 25 – 65years
• No elevated blood pressure (Blood pressure ≤ 130/≤80mmHg)
• No previous history of kidney and liver disease
• Individuals whose serum creatinine is lower than 1.1Mg/dL, AST and ALT levels not higher than 12IU/L and ALP not higher than 35IU/L. These were based on the established reference values documented for the kit used for the study.
Exclusion Criteria
• Motor park workers who do not take herbal medicines
• Those with elevated blood pressure
• History of kidney and liver disease
• Level of plasma creatinine higher than ≥0 Mg/dL
• Level of AST and ALT higher than 40IU/lL level of ALP higher than 120IU/L.
Sample Size Determination
The formula for calculating sample size for cross sectional study with laboratory quantitative components as described by Jaykaran and Biswas [20].
N = Z2SD2 / d2
N = Number of samples needed for the study
SD = Standard deviation from previous studies
d = Error margin or precision
Applying the formula,
SD = 9.1 [21]
Z= 1.96
d: 2% error margin (increasing the analytical precision to 98%)
N= 79
Considering 10% subject drop out = 7.9
Minimum number of participants required for the study is 87. The total number of participants that will be used for the study will be 101.
Data Collection
A total of 122 Motorpark workers were randomly selected from various motor garages within Ado-Ekiti metropolis after administering informed consent process and obtaining their consent Data was collected using a structured questionnaire and it included questions on demographic characteristics, lifestyle habits, and the consumption of herbal-based products.
Blood Sample Selection
Ten milliliter (10mLs) of venous blood was collected into heparin bottle. This was spun and plasma stored at -20oC until ready for use.
Screening of Sample for Testing of Predictive Markers: The plasma sample was used measure plasma creatinine (Cr), Alanine Transaminase (ALT), Aspartate Transaminase (AST) and Alkaline Phosphatase (ALP). This was performed to screen and identify individuals whose plasma level of conventional markers were higher than the reference values quoted in the kit literatures. These individuals were identified and excluded based on the defined inclusion/exclusion criteria established for the study. After the screening, 23 subjects had their plasma creatinine level higher than the reference value established for the kit and 63 subjects had their liver enzymes (AST, ALT and ALP) levels greater than the reference value established for the kit. These individuals were excluded for further testing for predictive markers of kidney and liver diseases. After the screening, 99 and 57 subjects were found eligible for further testing for predictive markers of kidney using Kidney Injury Molecule 1 (KIM-1) and liver using Alpha Glutathione transferase (α-GST) The details of number recruited, those excluded and number tested for predictive markers of kidney and liver diseases are shown in the study flow chart detailed below (Figure 1).
Alpha GST Assay Procedure [22]
Principle: The Glutathione-S-Transferase Assay utilizes 1-Chloro-2, 4-dinitrobenzene(CDNB) as the substrate. Upon conjugation of the thiol group of glutathione of the CDNB substrate, there is an increase in the absorbance at 340nM.
KIM 1 (Kidney Injury Molecule by Enzyme Linked Immunosorbentassay (ELISA) Method [23]
Test Principle: This method uses the Sandwich- ELISA principle. The micro ELISA plate provided in this kit has been pre-coated with an antibody specific to Human KIM -1. Standards or samples are added to the micro ELISA plate wells and combined with the specific antibody. Then a biotinylated detection antibody specific for human KIM -1 and Aridin- Horseradish Peroxidase (HRP) conjugate are added successfully to each microplate well and incubated. Free components are washed away. The substrate solution is added to each well. Only those wells that contain Human KIM-1, Biotinylated detection antibody and Avidin-HRP conjugate will appear blue in colour. The enzyme –substrate reaction is terminated by the addition of stop solution and the colour turns yellow. The absorbance is measured spectrophotometrically at a wavelength of 450nm. The OD value is proportional to the concentration of Human KIM-1. The concentration of Human KIM-1 in the sample is calculated by comparing the OD of the samples to the standard curve.
Creatinine (Colorimetric Method (With Deproteinization) [24]
Principle: Creatinine in alkaline solution reacts with picrate to form a colored complex. The colour formed is measured spectrophotometrically at 520nm.
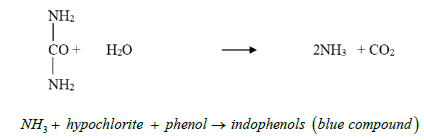
Plasma Urea (Urease – Berthelot Method) Colorimetric [25]
Principle: Urea in serum is hydrolyzed to ammonia in the presence of urease. The ammonia is then measured photo metrically by Berthelot’s reaction. The colour produced is read at 540 nm
Alkaline Phosphatase (Phenolphthalein Monophosphate Substrate [26]
Principle: Serum alkaline phosphate hydrolyses a colourless substrate o phenolphthalein monophosphate giving rise to phosphoric acid and phenolphtalein which, at alkaline pH values, turns into a pink coluor that can be photometrically determined.at 520nm.
Aspartate Aminotransferase (AST) [27]
Principle:
AST is measured by monitoring the concentration of oxaloacetate hydrazone formed with 2,4 – dinitrophenylhydrazine.
Alanine Aminotransferase (ALT) [27]
Principle:
Alanine Aminotransferase is measured by monitoring the concentration of pyruvate hydraxone formed with 2,4-dinitophenylhydrazine.
Ethical approval was obtained from the State Ministry of Health, Ekiti State. Population entry was achieved following a letter received from the state Chairman, National Union of Road Transport Workers. All the basic ethical principles for conducting medical research were adhered to strictly.
Data analysis was performed using descriptive statistics, including means, standard deviations, frequencies, and percentages. Inferential statistics, including chi-square tests, Student t- test, chi square test, ANOVA and logistic regression analysis were used to determine the association between the consumption of herbal-based products and the risk of liver and kidney injuries. Statistical package for social sciences software version 21.0 compatible software was used for the analysis of data. and correlation tests were for companism of variables. All significant level for variables was set at P<0.05.
Description of Demography of Respondents
The demographic characteristics of all respondents are shown in Table 1. In all, there were 99 respondents whose age ranged between 25 to 65 years. 9 (9.1%) were between the ages of 25 to 34 years; 36 (36.4%) were between 35 to 44 years, 42 (42.4%) of the respondents were between the ages of 45 to 54 years and 12 (12.1%) were above 55 years of age. Assessing the BMI of the respondents, 59 (59.6%) of the respodents had normal BMI, 33 (33.3%) had obesity while 7 (7.1%) had grade II obesity. The blood pressure of all respondents were within the normal range. Fifty four (55%) had BP of 120mmHg/70mmHg and 45 (45%) of the respondents had blood pressure reading of 130mmHg/80mmHg. Majority of the respondents were males. Ninety five (96%) of them were married, 2 (2%) single, 1 (1%) was divorced and 1(1%) was separated. Seventy four (77.9%) had one wife, 14 (14.7%) had two wives and 7(7.4%) were married to three wives. Thirty four (.34.3%) had between 1-3 children, 55 (55,6%) had 4-7 children, 8 (8.1%) had 8-10 children and 2(2%) gave no response. Majority of the respondents were Christians. Eighteen (18.2%) were Islam, 79 (79.8%) were Christians and 2 (2%) were traditionalists. Ninety seven (98%) were Yorubas and 2 (2%) were Ibos. Regarding education, 2 (2%) had no formal education, 26 (26.3%) had primary school certificate, 62 (62.6%) had secondary school certificate and 9 (9.1) had tertiary education.
Use of Herbal Medicine
Use of herbal medicine among respondents are detailed in Table 2. Majority of the respondents reported they used herbal medicine. Ninety one (91.9%) of respondents reported that they had used herbal medicine, while 8 (8.1) reported that they had not. Many who reported that they had used herbal medicine have consumed various types namely: Opa eyin (low back pain) 23 (25 .3%), Agbo jedijedi (pile) 40 (44.0%) and Agbo iba (fever) 28 (30.8%). They have used herbal medicine for various reason namely: treatment of health issues 49(53.9%); for alertness 17(18.7%), strength improvement 17 (18.7) and sexual performance 8 (8.8%). Indication that prompted them to use herbal drugs were: Malaria 32 (35.2%); Typhoid 11 (12.9%) and pile 48 (52.7%). Many of the respondents have used herbal medicine for various durations. Twenty five (27.5%), 18 (19.8) and 48 (52.7) have used herbal medicine for 1-5 years, 5-10 years and more than 10 years respectively. While 43 (43.4%) were aware that herbal medicine could cause various toxicities to their health, 56 (56.6%) of the respondents were not aware. Among those who used herbal medicine, 69 (69.7%) used it in combination with other non-steroidal anti-inflammatory drugs. Such as Alabukun (a form of salicylic acid), Panadol extra as against 30 (30.3) who did not. Majority 93 (93.9%) of the respondents had not reported any complication following the use of herbal-based products.
Prevalence of Kidney and Liver Disease Among Herbal Medicine Users
The prevalence of kidney and liver toxicities among the studied population using predictive markers is shown in Table 3. There were high level of users of herbal-based products who had elevated level of KIM-1 64 (64.6%) and elevated level of αGST 57 (64.9%) among the studied population.
Table 3: Prevalence of Predictive Kidney and Liver toxicities among motor park workers consuming herbal medicine.

Association Between Predictive Markers and the Duration of Use of Herbal-Based Preparation Among Studied Population
The association between predictive markers and duration of use of herbal-based preparations is shown in Table 4. Although there was no significant association between predictive marker of kidney (KIM 1) and duration of use of herbal medicine (P> 0.05), but individuals who have consumed herbal products for more than 10 years had higher level of KIM 1 48 (52.7%) than those in other groups. In the same vein, there was also no significant association between predictive marker of liver toxicity (αGST ) and duration of use of herbal medicine (P> 0.05), but individuals who have consumed herbal medicine for more than 10 years also had higher level of αGST 27 (50%) than those in other groups.
Table 4: Association between predictive markers and the duration of use of Herbal-based drugs among motor park workers.
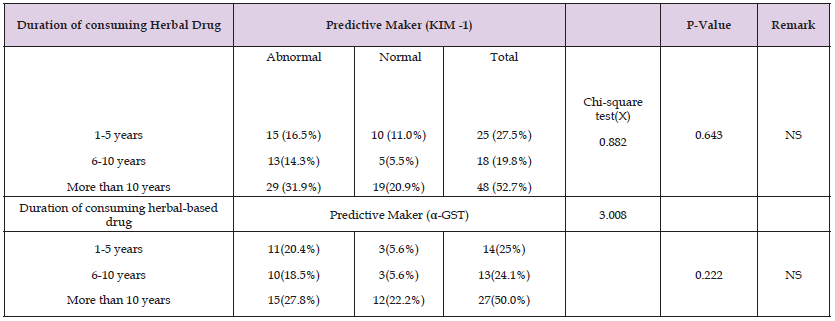
Note: NS: Non-Significant.
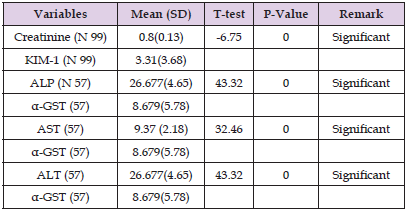
Comparative Analysis of Predictive Markers of Kidney and Liver with Conventional Markers of Kidney and Liver Disease Among Motor Park Workers Consuming Herba Medicine
There was a significant difference when the mean of predictive marker for kidney disease KIM1 (3.31 ±3.68) was compared with the mean of conventional marker creatinine (0.8±0.13), P= 0.000. In the same vein, there were significant differences when the mean of predictive maker αGST; (8.679±5.78) was compared with the means of different conventional makers ALP (26.677±4.65 IU/L) AST (9.37± 2.18 IU/L) and ALT (26.677 ±4.65 IU/L) of liver disease, P=0.000 (Table 5).
Table 5: Comparative Analysis of Predictive Markers of Kidney and Liver with Conventional Markers of Kidney and Liver Disease among motor park workers consuming herbal medicine.
Correlation between Predictive Markers of Kidney and liver with Conventional Markers of Kidney and Liver Diseases Among Motor Park Workers Consuming Herbal Medicine
Although, some level of positive and negative relationship exist between predictive markers of both kidney and liver disease and conventional markers, but there was no significant correlation between predictive and conventional markers of kidney disease (P>0.05); and predictive and conventional markers of liver disease P>0.05 (Table 6).
Table 6: Correlation between Predictive Markers of Kidney and Liver with Conventional Markers of Kidney and Liver Diseases among motor park workers consuming herbal Medicine.
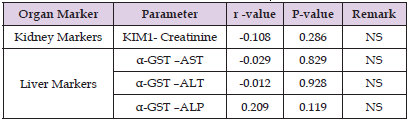
Note: NS: Not significant.
Herbal medicine has become a component of global health. Herbs and its components are regularly consumed across different continents. The data from this study showed that 91% of the studied population reported that they consumed herbal medicine to manage different ailments. This is consistent with the report of WHO [7] which showed that about 80% of individuals from developing countries used herbal medicine as source of primary healthcare. Increased consumption of herbal medicine in Nigeria has been attributed to inefficiency of the healthcare system, high cost of modern drugs, high cost of health care services, poor accessibility of few available healthcare facilities and accessibility of herbal mixtures across various locations [28,29]. Data showed that respondents used herbal medicine to treat different ailments; and this included typhoid, pile, sexual performance, malaria among others. This finding is consistent with the report of Ehrlish [2] and (Anim, et al. [9]). These authors reported that consumers of herbal medicine used same to manage various health disorder. This could imply that herbal medicine is preferred to orthodox medicine among the studied population. The belief that herbals are safe and natural could be responsible for its use to treat various mentioned ailments among the studied population.
While herbal medicine has become a popular component of global health, it is important to note that the use of unvalidated herbal remedies can be injurious to health. Unstandardized herbal products may contain toxic substances that could cause harm to major organs of the body, such as the liver and kidneys. Prolonged use of herbal medicine could lead to organ dysfunction and potentially cause sub-clinical renal and liver diseases, which can ultimately lead to acute or chronic organ damage. Many of respondents have used herbal medicine for different years in combination with modern drugs such as paracetamol and Alabukun (a type of aspirin). However, a good percentage (52.7%) of the respondents have used herbal medicine for more than 10 years. Previous report has shown that long use of unstandardized herbal products could predispose users to both kidney and liver toxicities [8].
Data from this study showed that a good number (56.6%) of respondents were unaware that herbal remedies could be injurious to their health. This finding is consistent with the report of Ehrlich [2] which reported that many users of herbal medicine lacked adequate knowledge that the use of herbal-based products could be injurious to their health. Knowledge and attitude have significant roles to curtailing public health diseases. Perception has an effect on how individuals respond to issues regarding their health. Poor knowledge with understanding regarding the adverse effects of unstandardized herbal products could exaggerate the pathological effects of excessive use of herbal medicine. While it is noteworthy that 93% of the respondents had not report any form of side effects following the use of herbal medicine, this does not negate the fact that unvalidated herbal products are completely safe for consumption. While many individuals may believe that herbal remedies are safe and natural, this is not always the case. Lack of knowledge and understanding regarding the adverse effects of unstandardized herbal products could exaggerate the pathological effects of excessive use of herbal medicine. The finding from this study showed that 64.6 % and 64.9 % of the studied population had elevated levels of KIM-1 and α-GST respectively.
This implies that the prevalence of kidney and liver disease among the studied population using predictive markers is high. Predictive markers such as KIM-1 and α-GST have been shown to be effective tools for diagnostic and prognostic assessment of renal and liver toxicities. These markers can detect sub-clinical organ dysfunction before it progresses to acute or chronic organ damage, allowing for early diagnosis and better patient outcomes. It is worthy to note that the values obtained for conventional markers to assess organ function among the studied population were all within the acceptable reference values. This data suggests that majority of the studied population are more likely predisposed to liver and kidney diseases. Although, 93% of the respondents reported no form of side effects following the use of herbal medicine, data from this study have evidenced they are likely predisposed to sub-clinical liver and kidney dysfunction. Sub –clinical organ dysfunction has been reported to be associated with excessive use of unstandardized herbal remedies; and accounted for 30-35% cases of acute renal failure [30,31].
The American College of Gastroenterology has also reported that Drug–induced liver injury, which is a form of liver disease has been on increase premised on the increase in the use of herbal and dietary supplement across the globe [32] Unvalidated herbal remedies when consumed in excessive amount could precipitate organ failure. In many situations, damages caused by herbal products on organs are often insidious [8] and the diagnosis could be missed due to non-predictive nature of the parameters used for the assessment of organ function. Furthermore, in many cases of renal and liver failure, sub-clinical renal and liver diseases precede either acute or chronic organ damage. Early diagnosis of both kidney and liver toxicities will not only improve patients outcome and prognosis, but will also limit the medical, social and economic consequences associated with these disorders and attendant pressure on health systems There was no significant association (P> 0.05) between predictive marker of kidney (KIM 1), liver (αGST) and duration of use of herbal medicine, but individuals who have consumed herbal medicine for more than 10 years had higher mean levels of KIM and αGST.
This finding is consistent with the report of Oshodi and Aina [28] who reported that prolonged use of herbal medicine could lead to kidney and liver disease. Long use of herbal products could have serious health implications especially on major organs of the body-kidney and liver. These organs aside helping to metabolize various xenobiotic, are also very critical in the metabolism of chemicals contained in herbal products. Long history of use of herbal medicine could have prolong effects on these major organs of the body. The role of predictive markers as a tool for diagnostic and prognostic assessment of renal and liver toxicities cannot be over emphasized. Data from the studied population showed that there was a significant difference between the mean values of KIM-1 and conventional marker of kidney disease; and between α GST and other conventional markers of liver disease (P= 0.000). The data from this study is consistent with that reported by (Giffen, et al. [15]) who reported that alpha GST is a viable biomaker because its levels increase more significantly than those of AST and ALT during hepatoxicity. Current biomarkers for assessing kidney and liver damages are not predictive, but diagnostic and prognostic. Creatinie level for example is affected by several factors including the hydration state of the body, body mass and levls are not increased until over 80% of the nephrons are lost. On the other hand, predictive markers such as KIM-1 and alpha GST are more sensitive markers of renal and liver damages, and level are increased as soon as unobserved clinical changes begins to occur in these organs.
It is evident from this study that a good number of subjects from the studied population had elevated levels of KIM-1 and alpha GST without any overt clinical symptoms of kidney and liver damages. Prolonged consumption of herbal-based products among the studied participants could precipitate kidney and liver diseases which could lead to chronic organ failure. Early detection of organ damages using predictive biomarkers could result in better disease outcome. This study also revealed that although there was no significant difference between the levels of predictive markers and duration of use of herbal medicine, but those who consumed herbal medicine for more than 10 years had higher levels of predictive markers for kidney and liver diseases respectively. This implies that use of unstandardized herbal products for a long time could have a deleterious effects on these organs. It is evident from this study that there were significant differences between the mean values of KIM-1 and conventional marker of kidney disease; and between α GST and other conventional markers of liver disease. This implies that assessing predictive are better indicators for organ dysfunction among the studied population.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
AAO conceptualized study, contributed to drafting of study protocol, drafted manuscript, managed and finalized manuscript review. MAA drafted study protocol, performed data collection, laboratory analyses and contributed to drafting of manuscript. Both authors agreed to the final manuscript.
We are grateful to all motor–park workers who gave their consent and agreed to participate in this study.


