Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yeasmin Jahan Afroze1*, Naznin Akter Jahan2, Iftekhar Hossain Chowdhury3, Irfan Nowroze Noor4, Masuma Tabassum5 and Sharmeen Tania Shovah6
Received: January 10, 2024; Published: February 01, 2024
*Corresponding author: Yeasmin Jahan Afroze, Assistant Registrar, Department of Facio-Maxillary Surgical Oncology., National Institute of Cancer Research and Hospital, Dhaka-1212, Bangladesh
DOI: 10.26717/BJSTR.2024.54.008606
Introduction: Oral health of women during pregnancy is an important part of health. Not only it can compromise pregnancy outcomes, but also it may affect their newborn’s overall health. The aim of the study was to find out the oral health problems and practices among pregnant women.
Methods: This descriptive type of cross-sectional study was carried out among 375 pregnant women. Sampling technique was convenient sampling and data were collected through face-to-face interview using a pretested semi structured questionnaire and a check list was filled in following oral examination.
Results: The percentage of decayed 52.7%, missing 20.0% and filled tooth 23.6% was more in age group ≥30 years (p<0.05) and age group 25-29 years had more gingival bleeding 53.3% and periodontal pocket 16.4%. Gingival bleeding 49.1% was more in 2nd trimester and periodontal pocket 16.4% was more in 3rd trimester (p<0.05). 52.6% participants ate sugar containing snacks or drinks in between meal more than twice a day had more gingivitis (p<0.05); 77.5% participants had decayed tooth went for their last dental visit in >1 year but <2 years; 87.5% and 29.2% participants had gingivitis and periodontitis went for their last dental visit in <6 months respectively.
Conclusion: Oral health related awareness, practices and services are the most important factor for improvement of the oral health of pregnant mothers.
Clinical Relevance: Scientific Rationale for Study: As we know, in developing countries the majority of people live under the poverty line and they lack of knowledge about oral hygiene. Everyone goes to the dentist when a problem arises. As a result, pregnant women suffer from different kind of health problem. When pain arise, if pregnant women take pain killer, drug causes abortion and different kind of complication.
Principal Findings: Oral health is one of the parts of health and has an important role during pregnancy.
Practical Implications: Prevent dental disease, it is crucial to practice good oral hygiene on a regular basis in pregnant women. Gingivitis is the most prevalent gum disorder, along with periodontitis.
Keywords: Oral health; Pregnancy; Woman
Pregnancy is a natural process accompanied with considerable physiological and hormonal changes in women’s body, including oral cavity. There are many common oral health problems in pregnancy such as gingivitis, periodontitis, tooth mobility, tooth erosion, dental caries, and benign gingival lesions [1]. Oral health is an important issue to general health of both the expectant women and her infants. The incidence of oral health problems has been positively correlated with lower educational achievement and lower socio-economic status [2]. Mother’s oral health practices during pregnancy, such as dental visits, oral hygiene, and consumption of sweets have a significant effect on their oral health during pregnancy and on their children’s oral health in the future [3]. Expectant women should be counseled to perform routine brushing and flossing, to avoid consuming excessive amounts of sugary snacks and drinks, and to consult a dentist during pregnancy [4]. A few oral changes are shown during pregnancy. Immunological, dietary, and behavioral factors associated with pregnancy are believed to be contributing factors. Pregnant women are especially susceptible to gingival and periodontal diseases. In addition, they may not experience symptoms until advanced disease stages and therefore unknowingly increase perinatal risks include premature birth, low birth weight babies, pre-eclampsia, ulcerations of the gingival tissue, pregnancy granuloma, and tooth erosion. These risks increase in women who experience nutritional deficiencies or have less frequent visits to the dentist.
In recent years, research linking periodontitis to the risk for adverse birth outcomes increased interest in the topic of oral health during pregnancy. Increased attention has been focused on maternal periodontitis and preterm and low birth weight [5]. Pregnant women may be more susceptible to periodontal disease since higher concentrations of estrogen and progesterone can induce hyperemia, edema, and bleeding in periodontal tissues, increasing the risk of bacterial infections [6]. Reduction in epithelial keratinization weakens the protective role of epithelium. If this change is influenced by a lack of concern for oral hygiene, plaque and multiplying microorganisms may cause gingivitis and periodontitis [7]. Gingivitis is the most common oral disease in pregnancy in such situations. It is inflammation of the superficial gum tissue. Periodontitis is a destructive inflammation of the periodontium affecting approximately 30 percent of women of child-bearing age. The process involves bacterial infiltration of the periodontium. Toxins produced by the bacteria stimulate a chronic inflammatory response, and the periodontium is broken down and destroyed, creating pockets that become infected. Eventually, the teeth loosen. A more serious situation is when periodontitis relates to osteolysis, the destruction of periodontal ligaments and formation of periodontal pockets that are reservoirs of periodontopathic anaerobic bacteria. Oral Health in pregnancy is an important issues and oral health status of pregnant women is recommending effective preventive measures [8].
Study Design
It was a descriptive type of cross-sectional study. The study was conducted among pregnant women for one year during the period of January 2020 to December 2020. The pregnant women were selected by using Convenient Sampling Method. Sample size was 375. Data were collected by face-to-face interview and oral health problems were identified by oral examination according to the checklist. To collect data, a semi-structured questionnaire was prepared considering variables and objectives of the study and a check list were prepared by following oral health assessment index. Then, translate into Bangla version and data were collected in field.
Pre-Testing
Before data collection, pre-testing of the questionnaire had been done, and sample size was 35. According to the finding of pre-testing necessary modifications were made to the questionnaire.
Data Analysis
Data analysis was done on the computer by using Statistical Package for Social Science (SPSS) software.
A. Table 1: Association between age group and gingival bleeding and periodontal pocket of participants (n =375)
Table 1 shows that the percentage of age group 25-29 years had more gingival bleeding 53.3% and age group ≥30 years and 25-29 years had more periodontal pocket 16.4% & 16.2% respectively. Chi-square tests show the association is statistically not significant and p >0.05.
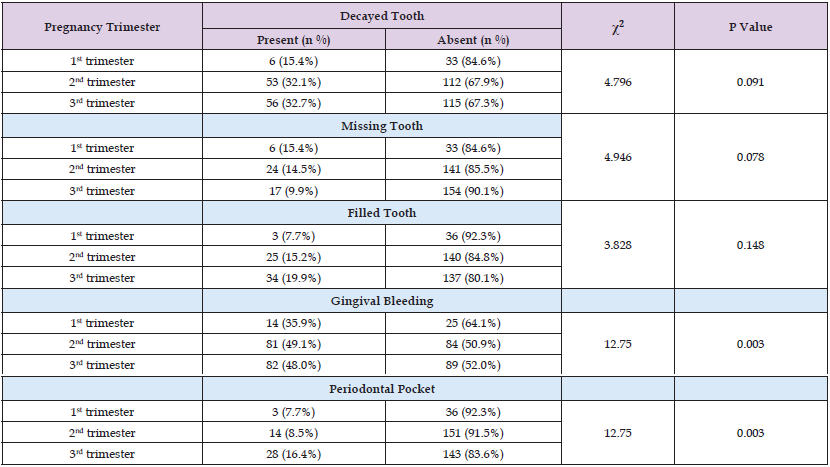
B. Table 2: Association between pregnancy trimester and decayed, missing, and filled tooth of participants (n= 375)
Table 2 shows that the percentage of decayed tooth 32.7% and filled tooth 19.9% was more in 3rd trimester than in 1st trimester. The percentage of missing teeth 14.5% was more in 2nd trimester. Chi-square tests show the association is statistically not significant and p >0.05.
C. Table 3: Association between oral health practices and problems: (n= 375)
Table 3 shows that 32.0% of participants brushed their teeth once a day had more dental caries. 32.4% irregularly brushed their teeth twice or more than twice a day and 36.0% brushed their teeth with toothbrush and powder and 12.6% participants brushed their teeth twice a day and 14.8% irregularly brushed their teeth twice or more than twice a day had more periodontitis. 14.3% brushed their teeth with charcoal or ashes. Chi-square test is statistically not-significant (p >0.05). Table 3 also shows that 68.8% participants brushed their teeth more than twice a day and 47.2% irregularly brushed their teeth twice or more than twice a day had more gingivitis. 85.7% brushed their teeth with charcoal or ashes. Chi-square test reveals that the test is statistically significant (p <0.05).
D. Table 4: Association between frequency of rinse of mouth and problems: (n= 375)
Table 4 shows that 62.5% participants rinsed their mouth 2-3 times in a week had more gingivitis. Chi-square test shows that the test is statistically significant (x2= 3.735 and p >0.05). Table 4 also shows that 31.3% participants rinsed their mouth 2-3 times in a week had more periodontitis. Chi-square test is statistically significant (x2= 8.453 and p <0.05)
E. Table 5: Association between dental visit and oral health problems: (n= 375)
Table 5 shows that 77.5% participants who had decayed tooth went for their last dental visit in >1 year but <2 years and shows that 35.0% participants who had missing tooth went for their last dental visit in >1 year but <2 years. The Chi-square test is statistically significant. Table 5 also shows that 57.5% participants had filled tooth went for their last dental visit in >1 year but <2 years. The Chi-square test is statistically significant.
Table 1: Association between age group and gingival bleeding and periodontal pocket of participants (n =375).
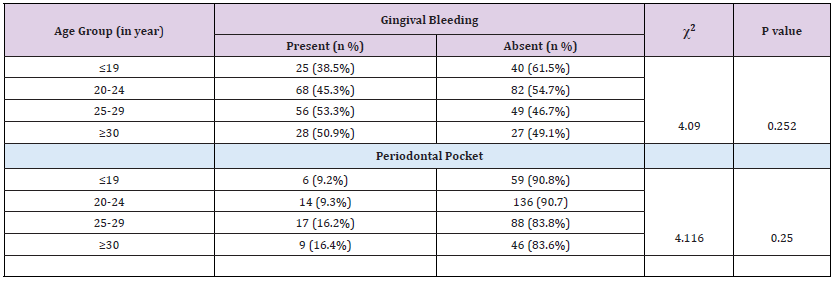
Table 2: Association between pregnancy trimester and decayed, missing and filled tooth of participants (n= 375).
The present study showed that 40.0% of pregnant women were in 20-24 years age group. The mean age of pregnant women was 23.99 years. These findings contrast with the study was done by [9] in Dhaka city, revealed that larger proportion of respondents (72%) had fallen within the age group of 20-24 years. 19% represented the age group of 15-19 years. In the United States a study was done to determine national and state-specific estimates of dental care use and found that 27.37% pregnant women were in between 25-29 age groups, 26.29% were between the ages of 20-24 years [10]. The study showed that 36.5% pregnant women’s educational qualification was up to secondary; 24.5% participant’s educational qualification was up to primary. Similar result was found in the past study where more than half of the respondents (57%) completed SSC level, 23% of the respondents had primary education respectively [9]. According to demographic characteristics among Carolina Oral Health Literacy study participants who were pregnant for the first time, 25% did not finish high school, 30% received a high school or general educational development diploma and 45% completed some college or higher education [11]. The present study showed that 65.5% pregnant women never went for a dental visit. 12.3% pregnant women went to last dental visit in more than 2 years but less than 5 years; 10.7% respondents went to last dental visit in more than 1 year but less than 2 years.
In 2011 a study was carried out to describe the self-reported oral hygiene habits and self-care in the oral health in a sample of Iranian women aged 21-35 years during pregnancy and found that 41% women had dental visit more than 2 years ago, 12% had visit less than 2 but more than 1 year ago, 29% visited dentist 6-12 months ago and 18% visited less than 6 months ago [12]. In this study the percentage of decayed tooth 52.7%, missing tooth 20.0% and filled tooth 23.6% was more in age group ≥30 years and age group ≤19 years had less decayed tooth 20.0%, missing tooth 4.6% and filled tooth 9.2%. In Iran a study revealed that the percentage of D/DMFT in 15–25 years age group was 78% and in 35–44 years age was 44%, while percentage of M/DMFT in 15–25 years and 35–44 years age group were 14 and 44%, respectively. The contribution of filling teeth among DMFT was low in all age groups [13]. The present study showed that the percentage of decayed teeth 32.7% and filled tooth 19.9% was more in 3rd trimester. The percentage of missing teeth 14.5% was more in 2nd trimester. A previous study presented that 69% respondents had dental problem in 2nd trimester stage, 27% reported at the stage of 3rd trimester and only 4% respondents were at the stage of 1st trimester. The present study also shows that 28.5% of participants had bleeding gum. 14.7%, 11.2% and 9.9% participants had food impaction in gum, swollen gum, and painful gum respectively and 29.3% participants had tooth sensitivity. 26.7% and 72% of participants had tooth decay and painful tooth respectively.
The previous study showed that respondents complained of bleeding gums, sensitive tooth, cavities, toothache and gingival swelling were 78%, 52%, 35%, 11% and 10% respectively [9]. The study showed that the percentage of gingival bleeding 49.1% was more in 2nd trimester and periodontal pocket 16.4% was more in 3rd trimester. In this present study 32.9% participants ate sugar containing snacks or drinks in between meal more than twice a day had more dental caries and 52.6% participants ate sugar containing snacks or drinks in between meal more than twice a day had more gingivitis. A study was done in Iran showed that women in third trimester of pregnancy had significantly more periodontal pocket > 3.5 mm, compared to women in second trimester. The study also revealed that sweet consumption more than once a day and flossing less than once a day were positively related to BOP [13]. The present study revealed that 92.5% pregnant women did not visit a dentist during pregnancy and only 7.5% pregnant women visited a dentist during pregnancy. Pregnant women who went for dental visit, among them 60.5% pregnant women’s reason for last dental visit were pain or trouble with teeth, gum, or mouth. In 2004-2005 in Ohio surveyed women regarding their perceptions of dental care and dental care practices. More than half 54% of the respondents reported that dental care was important during pregnancy, yet only 44% received care during pregnancy.
Fewer than half 40% treated they were advised by their obstetric provider to seek dental care during pregnancy, and 10% reported a dentist refused to provide them care because they were pregnant [4]. The study showed that the women who had decayed tooth 77.5%, missing tooth 35.0% and filled tooth 57.5% went for their last dental visit in more than 1 year but less than 2 years (p= 0.000). The previous study showed that expectant mothers who had dental visit in the previous years had significantly more filled and missed teeth (p < 0.01) and also women who did not visit a dentist in the previous years had significantly less DMFT.
This cross-sectional study has been observed that majority of the participants were young pregnant mothers with lower economic group, lower educational and occupational status. The educational and occupational statuses of pregnant women in Bangladesh were not satisfactory. Larger portion of the pregnant women gave priority of sweetened food or drinks as their extra meal which may predispose them to get more oral diseases and an extensive number of pregnant women did not seek oral health care during pregnancy. In addition to this, very few participants were advised to visit dentists by their prenatal care providers during pregnancy period. The study also revealed that majority of the pregnant women were suffered from gingivitis and dental caries and a small number of pregnant women got periodontitis. So, this study provided some directions in future research regarding the impact of oral health knowledge, behavior, and food habit on the pattern of oral diseases with a larger sample size and expanded volume of queries in questionnaire to evaluate the actual proportion of oral diseases and to find out the important predisposing factors in Bangladesh for better oral health outcomes.
The authors gratefully acknowledge the contribution of Md. Najmul Kabir Chowdhury, Associate Professor, Dhaka College, Dhaka.
YF: Conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources and software, validation, writing original draft, editing, and review. NJ: Conceptualization, funding acquisition, methodology, supervision, validation, writing original draft, editing, and review. IC: Conceptualization, methodology, supervision, writing original draft, editing, and review. IN: Conceptualization, methodology, supervision, writing original draft, editing, and review. MT: Conceptualization, methodology, supervision, writing original draft, editing, and review. SS: Conceptualization, methodology, supervision, writing original draft, editing, and review.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is funded by own funding research.
N/A
We have no conflict of interest in this research.
• Formal permission was taken prior to data collection from the Ethical Committee of NIPSOM, Dhaka as well as from Maternal and Child Health Training Institute and Dhaka Medical College Hospital.
• The respondents were explained about the possible comfort and discomfort as well as objectives of the study.
• No physical or chemical intervention was given to the respondents.
• At any stage of the study, the respondents should have the right to withdraw themselves from the study for any reason whatsoever.
• Memo no: NIPSOM/IRB/2020/1225. Date: 17/12/2020
N/A.
N/A.


