Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Carlo Bulletti1* and Francesco Maria Bulletti2
Received: January 18, 2024; Published: January 29, 2024
*Corresponding author: Carlo Bulletti, Past President of the “Società Italiana Di Fertilita’, Sterilita’ E Medicina Della Riproduzione (Sifes- Mr)”- Associate Professor Adjunt Department of Obstetrics, Gynecology and Reproductive Scince, Yale University, New Have (Ct) USA
DOI: 10.26717/BJSTR.2024.54.008593
Title: Italian Law 40/2004 and the Evolution of Reproductive Technology: A Comprehensive Analysis
Introduction: Law 40/2004 has been a contentious legislative measure in Italy, often labeled a “Catholic law.”
This law has significant ethical implications, particularly in the context of assisted reproductive technologies.
The legislation emphasizes respect for nascent life and includes provisions restricting various aspects of
reproductive techniques.
Historical Background: Infertility has been perceived differently throughout history, ranging from a personal
desire to a medical condition. Law 40/2004 marked a turning point in Italy’s reproductive landscape, with
significant opposition from religious institutions. However, it contributed to a substantial increase in assisted
fertilization births, accounting for approximately 4.2% of all newborns in Italy by 2021.
Access to Reproductive Assistance: The right to access infertility treatments and services is a crucial aspect
of reproductive justice. Challenges persist in ensuring equal treatment opportunities, particularly when public
options are limited and waiting lists are extensive, disproportionately affecting couples in their late 30s.
The Public vs. Private Dilemma: Private equity’s growing presence in fertility centers has raised concerns.
Private equity acquisitions may lead to higher spending without commensurate quality improvements.
Fertility care has become attractive for investment due to rising demand for Assisted Reproductive Technology
(ART) and its commercialization.
Navigating the Role of Third Parties in Reproduction: Genetic parenthood is evolving to emphasize the
commitment to care for a child, regardless of genetic connections. Third-party reproduction, including
donated gametes and gestational carriers, offers new possibilities for diverse family structures.
The Issue of Gestational Carriers in Italy: Gestational carriers, who carry pregnancies created by genetic
parents or gamete donors, present ethical and legal considerations. Evidence suggests that gestational
carriers, intended parents, and newborns do not experience harm, but prohibition is rooted in ideology and
religion.
Concluding Remarks: The clash of paradigms led to the enactment of Law 40 in 2004, resulting in considerable
implications for reproductive technology and patient access. The law’s application has faced constitutional
challenges and opposition from religious institutions, but it significantly contributed to assisted fertilization
births. The future of reproductive technology includes advancements in generative Artificial Intelligence,
genetic parenthood reconsiderations, and artificial womb technology, which may reshape parental roles
and workplace protections. Children may be born from two male parents, eliminating constraints related to
ovarian exhaustion in women.
Abbreviations: VR: Virtual Reality; AR: Augmented Reality; MR: Mixed Reality; ART: Assisted Reproductive Technology; ASRM: American Society for Reproductive Medicine; GCs: Gestational Carriers; PGT: Pre- Implantation Genetic Testing
The Law 40/2004 (https://www.gazzettaufficiale.it/eli/ id/2004/02/24/004G0062/sg) stands out as one of the most contentious legislative measures in the history of the Italian Republic. It is the outcome of a parliamentary debate that commenced in the late 1950s and escalated into what can only be described as highly impassioned discussions from the year 2000 onwards. Italian legislation concerning assisted reproduction unquestionably exemplifies the challenges of legislating on bioethical matters in our country. The narrow majorities achieved in parliament, exemplified by the final Senate vote on 10th February 2004 (where the law was approved with 277 votes in favor, 222 against, and 3 abstentions), along with the contentious results of the four repealing referendums held on 12th and 13th June 2005, serve as clear indicators that the approved text was far from a consensus-driven piece of legislation. Nonetheless, its relative approval was made possible by a cross-party majority that emerged during a political climate where, following the dissolution of the center, traditionally Catholic parties, representing both major parliamentary groups, sought to appeal to the moderate electorate known for its heightened sensitivity to certain issues. Consequently, in 2004, supporters of the subsequently ratified legislation included not only the center-right parties, traditionally conservative and in government at the time, but also some center-left parties and representatives who saw it as appropriate to align with the preferences of their Catholic constituents.
Furthermore, right from its inception, it was evident that Law 40 drew clear inspiration from certain values, particularly in its stance toward the unborn child. These values were undeniably influenced by the teachings of the Church’s Magisterium, to the extent that many have labeled it a “Catholic law.” While the nuances of the term “Catholic law” can vary considerably, it is indisputable that Italian legislation can be characterized, at the very least, as ideologically oriented. As one of its most prominent advocates, former president of the National Bioethics Committee (Comitato Nazionale di Bioetica) C.N.B., Francesco D’Agostino, aptly phrased it, the law is “not ethically neutral” as it consciously upholds a fundamental ethical principle—respect for life in general and nascent life in particular. From an alternative perspective, it is equally undeniable that Italian legislation, in its effort to balance the competing interests arising from the application of assisted procreation techniques, particularly those of the mother and the unborn child, primarily seeks to safeguard the embryo. This focus on protecting the embryo to a significant extent has led authoritative scholarship to identify an “imbalance” in favor of the embryo in terms of protection, to the potential detriment of the mother.
This emphasis is exemplified by regulatory provisions that prohibit experimentation on embryos (Article 13, Paragraph 1), interventions lacking exclusively therapeutic and diagnostic purposes (Article 13, Paragraph 2), any form of eugenic selection (Article 13, Paragraph 3), cryopreservation (except in very limited circumstances) and embryo disposal (Article 14, Paragraph 1), the creation of more embryos than strictly necessary for a single simultaneous implantation, not exceeding three (Article 14, Paragraph 2), as well as the reduction of multiple pregnancies, except for cases stipulated in Law 194/78 (Article 14, Paragraph 4). The legislation also imposes numerous restrictions on access to these techniques (Articles 4 and 5) and a complete ban on any form of heterologous procreation (Article 4, Paragraph 3), effectively preventing procreation in Italy for couples in which one partner suffers from absolute sterility. While subsequent parliaments and governments have displayed insensitivity to the gaps, inconsistencies, and constitutional concerns surrounding Law 40 since 2004, the same cannot be said for the Judiciary. From the very beginning of the law’s enactment, the Judiciary has consistently issued judgments of various levels and degrees of significance, especially regarding the law’s most contentious provisions.
Throughout history, the tension between innovation and the preservation of established norms has been a recurring theme, often resulting in individuals suffering as a consequence. Infertility within couples is a longstanding issue, dating back to ancient times. Even in biblical times, such as in the story of Sarah, the wife of Abram, who faced infertility and sought unconventional solutions, like having a child through her Egyptian slave, Hagar (Genesis 16:1-4). Initially, some viewed infertility not as a medical condition but as a personal desire, despite the World Health Organization categorizing infertility as a condition causing psychophysical suffering and treatable as an illness. In Italy, infertility affects approximately 15% of the reproductive population (source: https://www.iss.it/en/infertilità-e-pma). Significant changes in societal norms must navigate debates between liberals in representative democracies, who align with scientific guidance and societal sentiments, and conservatives who resist such “leaps forward” to preserve long-standing customs, often rooted in religious beliefs. In Italy, Nobel Prize (2010) laureate Robert Geoffrey Edward’s (1925-2013) pioneering work on in vitro fertilization raised hopes for addressing infertility among couples. However, the Italian medical- scientific community operated within a regulatory void. Over just 70 years, deeply entrenched principles, traditions, and methods of procreation, spanning millennia, were upended. This transformation stemmed from an outdated interpretation of nature that conservative factions sought to uphold, coupled with reluctance to embrace new parenting models that challenged the traditional genetic framework.
In the hierarchy of definitions of parenthood today, genetic parenthood seems to be superseded by that which can be defined as “a formal act of unlimited assumption of responsibility to love unconditionally who you decide is your child” The enactment of Law 40 marked a significant turning point in Italy’s reproductive history. It faced strong opposition from the Catholic Church and other religious institutions, despite leading to the birth of approximately 4.2% of new babies in the country as of 2021 (source: https://www.epicentro. iss.it/pma/stato-di-attuazione-della-legge-40-dati-2021). The average maternal age in Italy, at 36.8 years, exceeded the European average of 35 years (based on European IVF Monitoring - EIM 2018 data). Furthermore, Italy witnessed a substantial increase in births resulting from assisted fertilization, with a 73% rise over a decade, as reported by the Ministry of Health’s Statistics Office. In 2021, this accounted for 108,067 newborns, constituting approximately 4.2% of all newborns in the country by 2023. Critics labeled the period following Robert G. Edwards’ groundbreaking work as the “Wild West,” condemning in vitro fertilization as unnatural. This opposition was fueled by the strong resistance from the Catholic Church and other religious denominations. Despite Italy’s secular constitution, Catholic education and values wielded substantial influence, not only within conservative circles but also among liberal groups. Lawmakers, following extensive parliamentary hearings, enacted Law 40, which imposed significant restrictions on assisted reproductive techniques.
A consultative referendum was conducted, necessitating a quorum for validation. The Church discouraged participation to prevent the quorum from being met (https://opusdei.org/it/article/ il-papa-sostiene-lastensione-ai-referendum-sulla-fecondazione-assistita/). Although a significant portion of voters favored these techniques, the referendum was invalidated due to the failure to reach the quorum requirement. Instead of facilitating the introduction of Nobel laureate Robert G Edwards’ groundbreaking discoveries into Italian society, Law 40, with its methods and ambiguities, ushered in a decade of suffering. Infertile couples were compelled to seek reproductive treatments abroad, with approximately 3,000 couples embarking on such journeys each year (source: https://www.ansa.it/canale_saluteebenessere/ notizie/sanita/2019/04/06/eterologa-dopo-5-anni- 3000-coppie-allestero-ogni-anno_dcef4c06-2a13-41c7-a97b-6fd- 9f55969bc.html). Efforts were made to impede the implementation of the results of Edwards’ groundbreaking discovery through various means. Even today, attempts persist to outlaw surrogate pregnancy. This opposition involved the dissemination of misleading information, nostalgic references to traditional methods, ridicule of modern reproductive practices, and a strong emphasis on the religious concept of the sanctity of life prevalent in religious and theocratic societies, promoting solely “natural” means of reproduction without technological intervention.
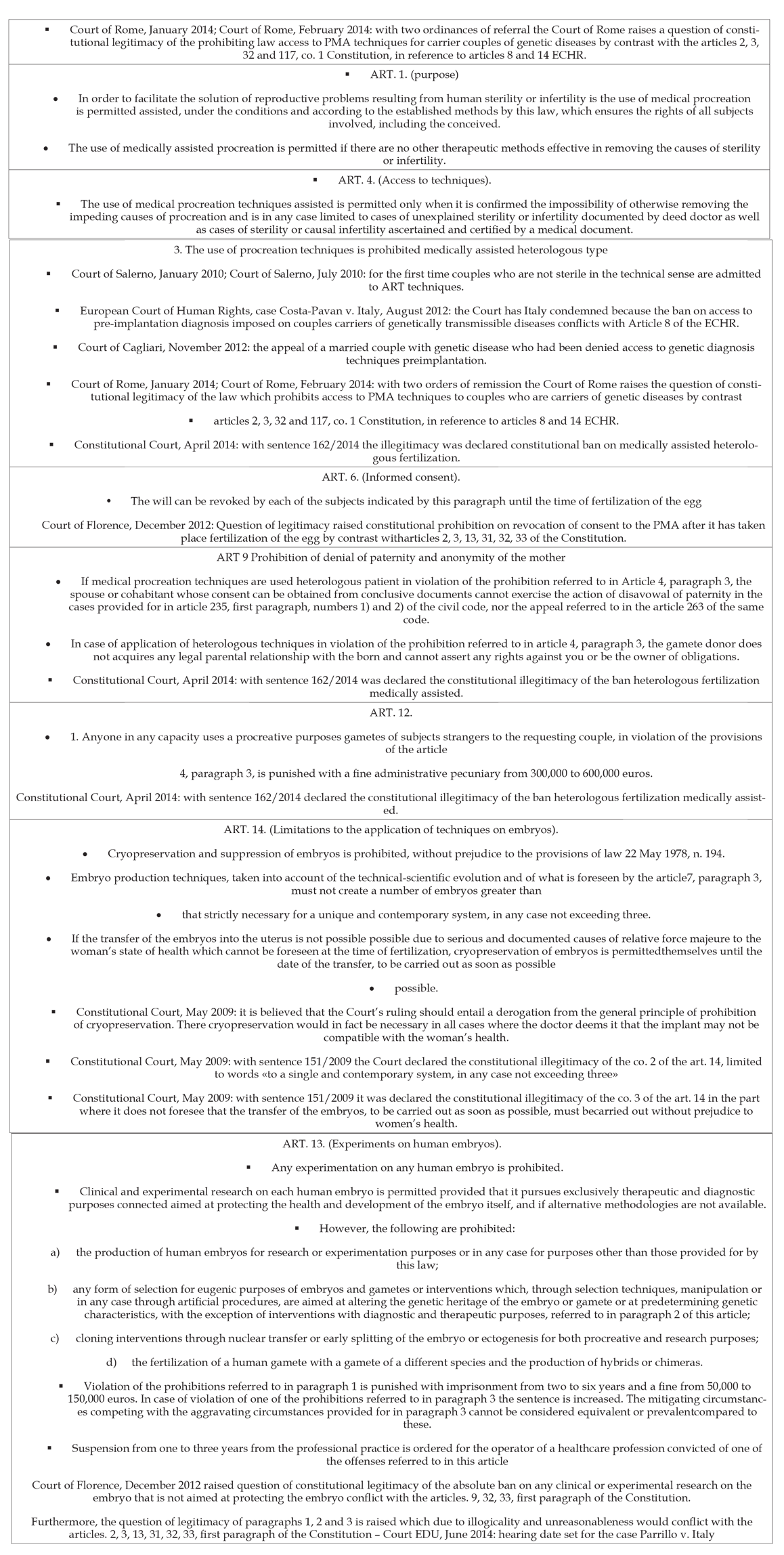
This stance distanced itself from embracing science and its accomplishments as integral parts of nature, particularly when applied to the realm of life. Ironically, it contradicted certain religious principles, leading to a complete rejection of life itself. The vehement opposition to reproductive technologies culminated in a fierce battle within the parliamentary chambers and the Senate. Ultimately, Catholic determination prevailed across the political spectrum. The prevailing narrative favored exclusively natural means of reproduction. The Church’s involvement in referendums further exacerbated the divide, encouraging people to abstain from voting to prevent the quorum from being met. Although a quorum is indeed required, the result becomes law irrespective of the voter turnout, thereby encouraging people to voice their opinions. Nevertheless, the suffering endured by infertile couples was undeniable, prompting the Constitutional Court to repeatedly assess the constitutionality of specific provisions within the law. These assessments led to the declaration of unconstitutionality, overturning many of the law’s prohibitions and marking a significant shift in the country’s reproductive landscape (Table 1). Over the years, starting from the first IVF birth in 1978, an estimated 12 million babies have been born as of June 2023 (source: https://www. focusonreproduction.eu/article/ESHRE-News-COP23_adamson).
Table 1: The robust democratic institutions in place, aimed at balancing state powers, enabled the Constitutional Court to rectify many scientific anomalies and social condemnations stemming from the law (Table 1). As we commemorate the 20th anniversary of the law’s enactment, some prohibitions remain in place, alongside persisting injustices and grievances stemming from previous bans. The key prohibitions outlined in Law 40, which regulated access to ART programs, have been addressed and removed by the Supreme Court. The crux of the law revolves around granting embryos the status of legal subjects, which, in turn, imposes a series of obligations and particularly restrictive prohibitions.
Delivery rates have been on a steady rise, constituting up to 7.9% of birth cohorts in Europe and up to 5.1% of children born in the United States [1, 2].
1. IVF does not have a significant impact on the health of children,
although the category of subfertile or infertile couples
carries a greater risk that becomes evident in the health outcomes
of their children whether they conceive in vitro or in
vivo. However, long-term studies are still ongoing [3].
2. Presently, nearly 3% of all children in Germany, and in countries
with liberal reimbursement policies like Denmark, as
much as 6% of all children, are conceived through in vitro
fertilization (IVF). In simpler terms, in every school class,
there is approximately one IVF-conceived child [4].
3. In Italy, as of today, approximately 4.2% of newborns are
born through the use of ART (Assisted Reproductive Technology),
with a clear increase in the proportion of children
conceived using this technique compared to spontaneous
conceptions. Additionally, the use of third-party reproductive
methods is also on the rise (source: https://www.iss.it/
en/rpma-dati-registro).
Data sourced from Istat (https://www.istat.it/it/files/2023/10/ Report-natalita-26-ottobre-2023.pdf) reveals a consistent decline in the number of births in Italy since 2008, a year that marked the highest recorded birth rate since the early 2000s. In absolute terms, there has been an average annual decrease of approximately 13 thousand births, amounting to a relative reduction of 2.7%. In comparison to 2008, Italy has witnessed a significant drop of over 183 thousand births, equivalent to a decrease of 31.8%. This decline in births can be attributed to structural shifts within the female population of childbearing age, typically considered to be between 15 and 49 years. In this demographic segment, the number of women has decreased over time. Those born during the baby-boom era (spanning from the latter half of the 1960s to the first half of the 1970s) have largely exited the reproductive phase, while those who remain within this age bracket today have been affected by the so-called “baby-bust,” characterized by a continuous decline in fertility between 1976 and 1995, culminating in the historic low of 1.19 children per woman in 1995. Additionally, the trend of children born to unmarried parents continues to rise. According to Istat, “there are 163,317 such births (+3.5 thousand compared to 2021, and nearly 50 thousand more than in 2008), constituting 41.5% of the total births.
Among these, 35.0% have parents who have never been married, while 6.5% come from couples where at least one parent has a prior marital history. Since the turn of the millennium, the proportion of births outside of wedlock relative to the total number of births has consistently increased, showing a gain of 33 percentage points.” Geographically, the majority of births to unmarried parents are in the Center (48.7%), followed by the North-West (42.4%), the North-East (42.3%), and the South (36.8%). Istat’s report also notes that “the recent increase in the share of births outside of wedlock (+1.6 percentage points) aligns with the average growth over the past decade (+1.5). This trend is especially prevalent among younger demographics, where births outside of marriage account for 59.5% of births among women up to 24 years old and 41.9% among those aged 25 to 34. Among native Italian couples, these figures rise to 73.2% and 45.7%, respectively. For couples above the age of 34, the proportion of births out of wedlock stands at 36.6% across all couples and 38.5% among Italian parent couples alone.” Furthermore, Istat highlights that “the majority of births outside of marriage are attributed to couples who have never been married (84.2% of the 163 thousand births in 2022), as opposed to couples where at least one partner has a prior marital history (15.8%). This is indicative of a value system, particularly among younger couples, where marriage is viewed as less obligatory than in the past before starting a family.
For instance, among mothers up to 24 years of age, births to never-married parents account for 54.6% of the total, compared to 36.4% for those aged 25 to 34, and 28.0% for those over 34.” Istat further notes that the critical issues concerning family planning have evolved over time. While at the beginning of the millennium, the focus was primarily on the decision to have a second child, today, the predominant factors influencing the choice to have children primarily revolve around economic challenges facing the country. “In 2022, nearly half of all births represent firstborn children,” as highlighted by the Institute. Specifically, firstborn births amounted to 192,525 units, accounting for 48.9% of all births, marking significant absolute growth (+6 thousand) and relative growth (+3.2%) compared to 2021. Conversely, births beyond the first child decreased by 6.1% in the past year. The increase in firstborn children can be attributed to couples finally realizing their postponed reproductive plans due to the pandemic. In fact, the growth observed between 2021 and 2022 fully offsets the reduction experienced between 2020 (192,142 firstborns) and 2021 (186,485 firstborns), amounting to a decline of -2.9%. However, it’s important to note that the increase in firstborns is part of an overarching long-term trend. From 2008 to the present, first-order births have seen a decrease of 32.4%, while subsequent-order births have decreased by 31.2%.
Furthermore, Istat indicates that the contribution to the birth rate by foreign citizens continues to diminish. “Children born to parents where at least one partner is foreign decreased in 2022,” as stated by Istat, totaling 82,216 births, constituting 20.9% of all births. Since 2012, the last year that saw an increase compared to the previous year, these births have declined by 25,789 units. Those born to couples where both partners are foreign nationals amount to 53,079 (26,815 fewer than in 2012), representing 13.5% of the total births. Births within mixed couples, which increased from 28,111 in 2012 to 29,137 in 2022, exhibit a less predictable trend over time. However, the maturation of immigrant communities in the country, as evidenced by the significant rise in Italian citizenship acquisitions, has made it increasingly challenging to assess the family behaviors of foreign-origin citizens. In fact, there has been a substantial number of citizenship acquisitions by those communities that significantly contribute to the birth rate among the resident population. Recent data on citizenship acquisitions reveal that, in 2021, approximately 40% of foreign women acquiring Italian citizenship hail from Albanian, Moroccan, and Romanian backgrounds. The prevalence of births to both foreign parents relative to the total number of births is notably higher in the Northern regions (19.3%), where foreign presence is more established, and to a lesser extent in the Central regions (15.1%). In contrast, the Southern regions report much lower incidences than the rest of Italy, with 5.6% in the South and 5% in the Islands.
On Average, Women in Italy Become Mothers at The Age Of 31.6 Years Old: “For the overall population of resident women, the average age at childbirth remains unchanged from 2021, standing at 32.4 years,” explains Istat. Notably, this average age is higher for Italian women (32.9 years) compared to foreign-born women (29.6 years). However, when compared to the data from 1995, there has been an increase of over two years in the average age at childbirth. Additionally, the average age at the birth of a woman’s first child has seen a significant increase, now at 31.6 years, which is more than three years higher than the corresponding figure in 1995. When comparing fertility rates by age in 1995, 2010 (both for Italians and total residents), and 2022 (again for Italians and total residents), there is a noticeable shift in fertility patterns towards older ages. In comparison to 1995, fertility rates have increased among women aged over 30, while they continue to decline among younger women. This trend becomes even more pronounced when considering Italian citizens exclusively. Among Italian citizens, the recovery of postponed childbearing is evident only starting from the age of 35 (shttps://www.istat.it/it/ files/2023/10/Report-natalita-26-ottobre-2023.pdf). Consequently, the percentage of individuals over the age of 65 has risen from 8.6% in 1955 to 24.0% today, and the average age of Italians has increased from 32.6 to 46.4 years. This calls for radical societal changes. A society that allows people to live longer lives should prioritize not only quantity but also the quality of everyone’s existence.
This includes strengthening essential services, starting with healthcare and social services, and extending to services that enhance overall quality of life. Furthermore, it is crucial not to abandon efforts to encourage a birth rate that arises from free and informed choices, primarily by women. Having children is a challenging endeavor in Italy, affecting couples of all kinds and particularly single women who choose to become mothers, a group that has been growing significantly. To address this, it is necessary to envision a comprehensive support system for childbirth. This system should expand the options for procreation within legal bounds, provide economic and social assistance to those wishing to overcome the challenges of “zero growth,” increase the availability of childcare facilities, and extend school hours. Additionally, it should establish assisted reproduction centers with efficient waiting list management, especially for women in their late 30s. Leaving a one or two-year waiting list for 38-year-old women is not assistance but a barrier to fertility, ultimately leading to infertility.
In recent years, there has been a growing awareness of the principles of reproductive justice, which has garnered increasing attention in various spheres such as media, public health, and public policy. However, one crucial aspect of the reproductive justice framework often goes unnoticed—the right to have a child, particularly the right and the ability to access infertility treatments and services. Individuals with low incomes and historically marginalized communities frequently face disparities in accessing infertility evaluations, treatments, and care. This commentary seeks to delve into these inequalities and advocate for their examination and resolution through the lens of reproductive justice. When we scrutinize access to infertility care in other countries from a reproductive justice perspective, it becomes evident that in order to uphold the right to have a child, we must critically assess the systems and structures that obstruct the realization of this right (Sister Song Women of Color Reproductive Justice Collective, available at: https://www.sistersong.net/reproductive- justice, data accessed January 10, 2024). This involves:
• Advocating against legislative and institutional policies that
perpetuate disparities in risk and resources, including unequal
insurance coverage, gender and racial pay gaps, and insufficient
support for paid family leave.
• Leading, funding, and prioritizing research that goes beyond
merely identifying disparities to uncover their root causes and
propose remedies for these inequitable outcomes.
• Envisioning a concept of reproductive health and well-being
that genuinely promotes reproductive justice, ensuring access to
infertility care irrespective of race, income, location, or insurance
status.
It is essential to note that assisted fertilization techniques do not entail extraordinary risks for newborns, while the selection of samples (hypofertility) poses greater risks to both newborns and maternal health [3]. In essence, the choice to pursue infertility treatments, whether it involves in vitro fertilization with or without gamete donation, pre-implantation genetic diagnosis, or the use of gestational carriers, falls within the realm of scientifically validated medical options for addressing reproductive health challenges. The rejection of these options by conservatives or those adhering to their religious doctrines remains a matter of individual choice and should not be used as a tool for coercing others. This upholds the principles of a liberal democratic system. Moreover, challenges persist in ensuring equal treatment opportunities, particularly in cases where treatment facilities are imbalanced in favor of the private sector, and public treatment options are limited with waiting lists exceeding a year. For couples, especially those in their late 30s, such waiting lists do not constitute a treatment option but rather a barrier to fulfilling their desire to have children [5].
The rapid expansion of private equity into the realm of women’s health, specifically fertility, mirrors the pace and extent of acquisitions observed in other sectors of the healthcare industry [6,7]. The growing role of private equity in fertility: A measured view, available at https://www.fertstert.org/news-do/growing-role-private-equity- fertility-measured-view. While private equity investments have extended across hospitals, ambulatory surgery centers, retail healthcare, and physician practices, fertility has emerged as a medical specialty with the most significant market share under private equity ownership. By 2018, nearly 15% of fertility practices were affiliated with private equity, accounting for 29% of all assisted reproductive technology cycles performed in the United States. Some of the largest fertility practices in the country are now backed by private equity firms, such as Inception Fertility (backed by Lee Equity), US Fertility (backed by Amulet Capital), Pinnacle Fertility (backed by Webster Equity Partners), and Ivy Fertility (backed by In Tandem). This level of private equity involvement in fertility underscores the imperative for reproductive endocrinologists (REIs) to comprehend the role of private equity and its ramifications in today’s healthcare landscape.
In Europe, particularly in countries like Italy and Spain, private equity has recently acquired the majority of fertility medical centers, including IVIrma, Genera, 9.baby, and Eugyn One notable example is IVI RMA, a reproductive medicine group backed by KKR, which has acquired the North American operations of Eugin Group, encompassing the Boston IVF fertility network and Toronto-based TRIO, from healthcare group Fresenius. This strategic expansion aims to position IVI RMA as a prominent fertility group in North America and strengthen its commitment to delivering fertility services. The acquisition will add over 600 employees across 13 labs and 32 satellite offices to IVI RMA’s existing network, bringing the organization’s total headcount to more than 4,400 globally. Moreover, Boston IVF brings multiple academic affiliations, including prestigious institutions such as Harvard Medical School, Dartmouth Hitchcock Medical School, Boston University Medical Center, and Tufts Medical Center. The move signals IVI RMA’s dedication to further growth and collaboration with like-minded physicians and organizations that share its cultural and medical vision for leading in the U.S. medical landscape. (https://www.reuters. com/markets/deals/kkr-talks-buy-spanish-fertility-clinic-company- eugin-fresenius-report-2023-10-02/;https://www.bloomberg. com/news/articles/2022-03-28/kkr-is-said-to-near-deal-for-fertility- treatment-provider-ivirma-l1aglpjd?embedded-checkout=true).
The increasing presence of private equity in fertility centers necessitates a closer examination of its impact on healthcare delivery and patient outcomes. Private equity refers to the use of capital from institutional investors for investing in private companies, aiming to sell these holdings within 3 to 7 years, typically to other private equity firms or corporate owners, often resulting in substantial profits. These investments often involve high levels of leverage, using debt to finance the acquired company. These ventures can yield annual profits exceeding 20% to 30%. For medical practices, particularly those run by physicians, private equity can offer significant advantages. It injects capital into these practices, facilitating infrastructure improvements, expansion, and provides business and managerial expertise, all while benefiting from economies of scale. Founders of these clinics may receive substantial payouts and enjoy investment diversification as well. A common business model in this context involves private equity acquiring a “platform” practice, typically a larger practice with brand recognition, multiple offices, physicians, and a broad geographic reach. Smaller practices are subsequently added to consolidate the field. From an economic standpoint, consolidation allows practices to grow their local market share, centralize administrative and operational functions, and reduce overhead costs. Larger practices also gain greater negotiating power with payers and suppliers.
In a healthcare landscape that is increasingly complex, private equity can provide a source of capital that enables fertility practices to expand and compete effectively against larger entities. Fertility has become an attractive sector for outside investment due to several key factors. Firstly, the demand for Assisted Reproductive Technology (ART) has consistently risen in the United States due to delayed childbearing, increasing infertility rates, and improved success rates of in-vitro fertilization (IVF). The commercialization of ART services has expanded beyond infertility treatment, encompassing fertility preservation and preimplantation genetic testing (PGT), contributing to a substantial $8 billion fertility services market, with IVF services projected to grow at a 10% rate through 2024. Secondly, the fertility landscape remains highly fragmented, with practices historically operating independently, bucking the trend of physician employment by larger healthcare institutions. Furthermore, fertility care has traditionally involved a predominantly cash and commercial payer base, making it a lower-risk field in terms of reimbursement and regulation, compared to specialties reliant on Medicare or Medicaid. This environment results in limited regulation, a high rate of self-pay for infertility treatment, and reportedly robust operating margins, particularly for IVF.
These factors have made private equity’s entry into the fertility sector particularly noteworthy. However, concerns have arisen about potential impacts on costs, access, and equity. Worries include pressure to maximize returns, potentially leading practices to prioritize self-pay patients over insured ones, deliver streamlined, low-complexity care rather than meeting complex needs, or establish new offices in higher-income areas instead of socio-economically disadvantaged communities. Such pressures might also encourage revenue diversification through elective procedures and ancillary services, increased internal referrals, and reliance on lower-cost clinicians. In the realm of fertility, profit-driven motivations could prompt patients to undergo costly, potentially unnecessary procedures or limit services to those with higher financial means. The acquisition of the majority of infertility treatment centers, in a logic of growing revenues imposed by private equity together with the employment of many gynecologists in the sector, can determine some obvious dangers:
• Abusing the use of diagnostic tests or therapeutic measures
of unproven efficacy but high cost (adds On); (ESHRE Addons
working group, [8], dead184, https://doi.org/10.1093/
humrep/dead184; https://www.dailymail.co.uk/health/article-
11574771/amp/Risky-IVF-add-ons-audit-couples.html?
fbclid=IwAR3ZVFVSvVYiFyEhXfuQOAilsInsV2_yNFEFg7_
rdxygbRcwkFW9cm2neqk).
• Intercept couples under the age of 35 with a hasty start to
treatment;
• Occupy the majority of the directors of the scientific societies
that liaise with the government in the negotiation of the price
list of the IVF cycles paid to the affiliated private centers thus
introducing conflicts of interest between their work dependence
and their work dentologically directed to the interests
of the community through the scientific society (conflict evident
when reading the ethical code of any scientific society).
Lastly, always from the representative table of the scientific societies, give scientific visibility to the invisible through a tacit agreement to invite them to society conferences and receive infertile couples for treatments. Or include them in scientific publications with the same purpose, increasing the number of authors even to over 20 names without them knowing the contents [9]. While there is limited empirical evidence regarding the effects of private equity in fertility, findings from other healthcare sectors suggest that private equity acquisitions may lead to higher spending without commensurate quality improvements. However, the unique nature of fertility care in the U.S., which allows easy tracking of pregnancy success rates, may yield a more nuanced impact on quality metrics. Some data suggests that private equity-affiliated practices may offer lower shares of ART cycles for male-factor infertility, increased use of pre-implantation genetic testing (PGT), with no differences in IVF success rates for women under 35. Moreover, the effects of private equity on Reproductive Endocrinology and Infertility (REI) training, satisfaction, and retention remain largely unknown. Recent research indicates affiliations between a quarter of fellowship programs and medical schools with private practice fertility clinics, potentially altering productivity expectations, workplace culture, practice patterns, and career paths for new generations of REI physicians. Additionally, it remains uncertain whether the involvement of private equity in clinics will support or alter research and development efforts in fertility [10].
The ongoing trend of private equity in the fertility sector necessitates careful consideration. Private equity investments may provide benefits such as practice growth, enhanced access to care, and improved quality through knowledge transfer. However, they also carry potential risks, including the prioritization of profits over patient care. The effects on the fertility workforce, including turnover, workplace culture, and physician satisfaction, are not yet fully understood but require investigation. As private equity’s influence grows, professional societies and policymakers are taking steps to address potential negative impacts. Transparency of practice ownership and potential regulatory enforcement may be necessary to ensure the preservation of patient care and clinical quality [6,7]. The growing role of private equity in fertility: A measured view, available at https://www. fertstert.org/news-do/growing-role-private-equity-fertility-measured- view). In conclusion, while private equity can bring benefits, it is essential for physicians to weigh the potential positive and negative consequences of these ownership shifts in the fertility sector as they continue to evolve.
The traditional notion of genetic parenthood as the primary factor in determining parental status is undergoing a transformation. It is gradually yielding to a new definition of parenthood, which places greater emphasis on the formal commitment to wholeheartedly love and care for a child, irrespective of genetic connections. In today’s context, this assumption of responsibility is progressively overshadowing the concept of genetic parenthood, as it offers more robust and enduring assurances of child-rearing. Third-party reproduction encompasses the utilization of donated eggs, sperm, or embryos from a third party (the donor) to assist individuals or couples (the intended parents), particularly those grappling with infertility, in conceiving a child. This concept departs from the traditional model of a father-mother family where third-party involvement is absent. Third-party reproduction is also pursued by couples facing challenges with natural conception, same-sex couples, and unpartnered individuals. It has emerged as a highly effective treatment alternative, especially within the evolving landscape of diverse family structures. Consequently, this therapeutic avenue has become a pragmatic solution, bringing immeasurable joy and fulfillment to individuals who might otherwise have been unable to embark on the journey of parenthood if these medical and legal possibilities were not accessible. Thus, third-party reproduction encompasses the utilization of donated gametes (sperm or oocytes), donated embryos, or the engagement of a gestational carrier (GC) to facilitate another individual or couple in realizing their dreams of parenthood.
Over time, the terminology linked to third-party reproduction has become a subject of debate within the scientific community. In 1978, Louise Brown gained worldwide recognition as the first “test-tube baby.” However, subsequent pioneering cases emerged in the field of fertility treatments that involved third-party contributions. The term “artificial insemination” persisted for a considerable period. https:// www.nytimes.com/1978/08/06/archives/life-in-the-test-tube.html In 1983, an Australian woman in menopause achieved a successful pregnancy through the donation of oocytes by a younger woman. In 1985, a woman without a uterus accomplished parenthood when one of her own eggs was fertilized in vitro and then transferred into another woman’s uterus, who carried the pregnancy on her behalf (.Gamete and embryo donation have firmly established themselves as fertility care options accessible to individuals and couples confronting infertility or genetic conditions. In recent years, with the expanding landscape of diverse family models, an increasing number of patients, including single men and women, same-sex couples, and transgender individuals seeking parenthood, have embraced these techniques more extensively. The concept of new forms of parenthood has gained prominence. Significantly, just a few months ago, the UK witnessed the birth of the first children conceived using DNA from three parents (source: Scientific American). This challenges the conventional notion that “a baby must have one mother and one father (genetic),” as it is no longer universally applicable.
Introduction
Traditionally, genetic parenthood has been the primary determinant of parenthood. However, contemporary perspectives are evolving to emphasize the formal act of assuming unconditional responsibility and love for a child, irrespective of genetic ties. This shift has given rise to the use of gestational carriers (GCs) as a means of assisted reproduction, allowing individuals or couples to have a child through the transfer of an embryo created by genetic parents or gamete donors.
Gestational Carrier Defined
A gestational carrier, often referred to as a GC, is an individual who carries a pregnancy resulting from the transfer of an embryo created by one or more genetic parents or gamete donors. Notably, the GC does not provide the egg and, therefore, is not genetically related to the child, distinguishing this method from traditional surrogacy where a genetic link exists.
Evolution of Gestational Carrier Usage
The birth of an infant conceived through in vitro fertilization (IVF) and the use of a GC in 1985 marked a significant milestone, sparking worldwide medical and legal discussions. Initially sought by individuals with a long history of infertility, the utilization of GCs has expanded over the years. With advancements in embryo cryopreservation, more than half of GC cycles now involve frozen embryos. In the United States, data reveals a substantial increase in the number of GC cycles, accounting for 2.5% of IVF cycles in 2013. In 2019, approximately 5.4% of embryo transfers in the US involved gestational carriers.
Complexity of GC Utilization
The use of GCs is a multifaceted process, distinct from egg donation. The American Society for Reproductive Medicine (ASRM) has provided recommendations for practices employing GCs. These guidelines offer insights into non-medical factors influencing GC selection, including ethical and legal considerations.) [11,12]; 10.4103/ jhrs.JHRS_138_17. PMID: 30568349; PMCID: PMC6262674. https:// www.asrm.org/practice-guidance/practice-committee-documents/ recommendations-for-practices-using-gestational-carriers-a-committee- opinion-2022/).
Research Questions and Findings A comprehensive literature review yielded 248 relevant articles addressing various aspects of GC utilization.
Findings Revealed
• Gestational carriers serve as a gold-standard medical provision
for individuals facing absolute obstacles to carrying a pregnancy
to term.
• The desire to transmit life to a child is considered a biological
right or amenity.
• The ethical permissibility of gestational carriers for samesex
couples is a topic of debate.
• Evidence indicates that gestational carriers, intended parents,
and newborns do not experience psycho-physical harm.
• Prohibition of gestational carrier procedures is primarily
rooted in ideology and religion.
• The self-determination of one’s body usage is a fundamental
principle, similar to organ, tissue, and gamete donation.
• Detachment of a supposed “specific” mother-fetus dialogue
does not generate pathology.
Ethical concerns include respect for human life and potential exploitation of individuals with low economic conditions through attractive financial offers. Some countries exclude economically disadvantaged women from becoming gestational carriers to address this criticism. However, babies born from gestational carriers show no detectable harm, similar to those adopted at birth, when raised in loving environments. In summary, gestational carriers offer a viable option for individuals and couples facing reproductive challenges. Ethical concerns surrounding self-determination, body usage, and human dignity persist but must be balanced with the potential for fulfilling parenthood dreams and the absence of harm to all parties involved.
In the era of digital advancements and the emerging metaverse, the healthcare sector, particularly assisted reproductive technology (ART), stands at the forefront of innovative possibilities. With the global metaverse market predicted to reach a substantial USD 824.53 billion by 2030, IVF clinics have a unique opportunity to integrate digital technologies with fertility treatments (source: Metaverse Market Size and Forecast, March 2023). This integration has the potential to improve accessibility and prioritize patient-centered care, catering to the expectations of tech-savvy Millennials and Generation Z. However, while these advantages are promising, they come with challenges, including safeguarding patient privacy and addressing technological disparities. This article delves into the role of fertility clinics within the metaverse, exploring the potential for treatment, patient engagement, and staffing while recognizing the obstacles on the horizon. The Metaverse Unveiled: The metaverse is a swiftly evolving digital ecosystem that envisions an immersive virtual realm where users can interact and experience life in ways not achievable in the physical world. This immersive experience is built upon technologies such as virtual reality (VR), augmented reality (AR), and mixed reality (MR), offering a wide array of applications, spanning gaming, entertainment, education, and virtual workplaces. While its ultimate function remains subject to ongoing development, the metaverse is designed to complement and expand upon the existing internet infrastructure.
The clash of paradigms that led to the enactment of Law 40 in 2004, and its subsequent prohibitions after approximately 25 years of the application of the groundbreaking “in vitro fertilization” technology, resulted in considerable implications. This journey, which initially brought hope to sterile couples struggling with fertility issues, and later reversed most of the bans, underscores several important reflections:
• Belonging to the world of liberal democracies within a
semi-globalized context of democracies allows individuals to seek
necessary medical treatments abroad, provided they can afford
the higher costs.
• The principle of utilizing the outcomes of technological research,
as long as it doesn’t harm third parties and prioritizes
the health of the newborn, aligns with the principle of individual
self-determination in a secular state. It supports the free choices
made by individuals, free from ideological, political, or religious
biases that intrude upon secular constitutional rights.
• Legislative regulations should be adaptable and founded on
general and flexible principles, capable of accommodating subsequent
technological advancements. This approach ensures that
evolving innovations do not result in pockets of unnecessary suffering.
• The regulations must be in tune with present realities, while
also acknowledging ongoing research worldwide. This awareness
should guide the formulation of rules and choices that promote
progress and change.
• A universal crime proposal related to third-party pregnancy
should be rooted in scientific data rather than mere ideology. Any
associated prohibitions should be detailed, with specific considerations
for oblations.
• The nation itself should adjust its laws to avoid ambiguity
concerning the procurement of gametes from abroad, where bans
may still apply. This can involve public and private institutions,
including hospitals and healthcare networks, covering the costs
of gametes not readily available within the country.
• The evolving landscape of reproductive technology presents
intriguing possibilities, including the rapid advancements expected
in generative Artificial Intelligence, genetic parenthood reconsiderations
in light of children born to three genetic parents, and
the advent of artificial wombs, which could reshape parental roles
and workplace regulations.
• New scientific discoveries will inevitably face resistance,
often stemming from efforts to uphold traditional values or religious
beliefs. However, over time, such resistance tends to wane,
allowing society to embrace innovative breakthroughs.
• Respect for the law has always been paramount, and the line
between adhering to it and addressing medical needs has historically
been where ethical medical indications have prevailed.
• In just seven decades, long-standing principles and traditions
regarding human reproduction have been upended. Law 40,
despite opposition from religious institutions, has contributed
significantly to the birth of approximately 4.2% of newborns in
Italy, reshaping the reproductive landscape.
• The intention of Italian law should have been to facilitate
the adoption of Nobel Prize-winning discoveries in reproduction.
Instead, its methods and ambiguities led to a decade of suffering
for infertile couples, forcing them into reproductive migration to
access essential healthcare.
• Attempts to impede scientific advancements, such as banning
pregnancy for others, have often relied on misleading
information, nostalgia for traditional methods, and religious
arguments. The rejection of scientific progress in the realm of reproduction
contradicts religious principles and the broader embrace
of science in society.
• Despite opposition, representative democracies have legislated
and respected the rule of law, even when religious institutions
sought to influence policy outcomes.
• The constitutional court has played a pivotal role in addressing
the unconstitutionality of various sections of the law,
relegating many prohibitions to the country’s history.
• A robust public healthcare service is essential for an equitable
and universal healthcare system. Allowing private sector
interests to overshadow public interventions poses risks that a
well-functioning society cannot afford.
Practices such as adding unnecessary exams or procedures, driven
by profit motives in the private healthcare sector, have been criticized
by scientific societies as contributing to financial gains at the
expense of patient well-being (as exemplified by ESHRE’s recommendations
against such practices).
We need legislation that can adapt to the evolving landscape of science. Legislation should support procedures that pose no evidence of harm to third parties and, therefore, should not be subject to regulatory prohibitions. Furthermore, we must respect religious beliefs that do not seek to impose specific reproductive techniques on their adherents. However, it’s crucial that individuals, acting on behalf of their beliefs, do not inflict suffering on others. It’s worth noting that both Italy and Europe have expressly secular constitutions.
Despite the legal prohibition on trading gametes, assisted reproduction centers across the country, both public and private, have been increasingly providing gametes, often at market prices. This practice continues unabated, even as the Pope expresses support for a conservative bill that would criminalize the use of gestational carriers for those physically unable to carry a full-term pregnancy, citing concerns about the commodification of the human body. The same behavior was expressed at the time of law 40 promulgation with the invitation to the Italians to avoid to vote to not rech the quorum requested Paradoxically, the state continues to financially support the acquisition of oocytes and spermatozoa from donors abroad, whether offered for free or at a cost. The question arises as to whether using a reproductive organ, whether voluntarily or for compensation, can truly be distinguished from the commodification of gametes offered in similar ways. (https://www.gazzettaufficiale.it/atto/serie_ generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta= 1998-07-11&atto.codiceRedazionale=098A6139&elenco30giorni= false;https://www.avvocatipersonefamiglie.it/notizie/ altro2/costituisce-reato-il-commercio-di-gameti-anche-nellambito- della-fecondazione-eterologa/; https://www.avvenire.it/vita/ pagine/litalia-nel-viavai-globale-di-embrioni)
• It is crucial to emphasize that any proposal to universally
criminalize surrogacy should be based on sound scientific evidence
rather than ideological beliefs. Such legislation should include clear
provisions and details regarding the prohibitions. Additionally, the
country should address the ambiguity surrounding the prohibition
of commodifying human bodies. Public and private institutions, including
hospitals, regions, and large healthcare networks, should be
allowed to procure gametes from abroad, as they do for those not
readily available in Italy due to existing bans. There is a growing trend
of both conservative and progressive government regions purchasing
gametes. Furthermore, penalties for transgressions should be clearly
defined, with fines of up to 600,000 euros and imprisonment for up to
2 years for those purchasing oocytes with state approval. It is worth
noting that those who choose to engage in sexual activities for financial
gain should not face any sanctions, a stance that seems justified.
While there are other instances of individuals renting their bodies
for various purposes, such as agricultural labor, this discussion could
lead to further complexities. In addressing these debates, it’s essential
to acknowledge the future developments likely to shape the next
30 to 40 years.
o These include the rapid advancement of generative Artificial
Intelligence, which will accelerate scientific progress and have a
profound impact on democracies worldwide. The concept of genetic
parenthood, upon which many countries’ legal systems are
based, may need swift revision, particularly in light of cases in England
where children have already been born with genetic contributions
from three parents (two mothers and a father).
o Additionally, advancements in artificial womb technology
may lead to changes in current choices, such as uterus transplants
and surrogacy, with potential legal and social implications
regarding parental roles and workplace protections [9,13-15].
In the future, children will be born also from two male parenthood.
Remarkably, today, there are already three generations of
mice conceived and born through somatic cells taken from their
tails, a development that Nature has aptly dubbed “sons of two fathers.”
This breakthrough signifies the elimination of constraints
related to ovarian exhaustion in women and opens the door to
possibilities like Emperor Hadrian realizing his dream of having a
child with his beloved Antinous [16-25]; Mice with Two Fathers?
Researchers Develop Egg Cells from Male Mice Recent research
offers a tantalizing glimpse at a future in which two men can have
biological children together, but any human applications remain
far in the future (https://www.scientificamerican.com/article/
mice-with-two-fathers-researchers-develop-egg-cells-frommale-
mice1/).
o Nevertheless, it is expected that new leaders will vehemently
oppose these groundbreaking scientific achievements and
make every effort to obstruct their utilization [26-39]. They will
likely attempt to impede scientific applications that promote life,
all in the name of defending life itself, as per their own interpretations
and religious beliefs. Fortunately, history has shown that
such resistance tends to wane over time, akin to tears dissolving
in the rain.


