Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Pauline Dike1, Isatta Wurie1,2* and Mohamed Samai1
Received: January 09, 2024; Published: January 24, 2024
*Corresponding author: Isatta Wurie, College of Medicine and Allied Health Sciences, University of Sierra Leone, Sierra Leone
DOI: 10.26717/BJSTR.2024.54.008585
Background: Complete blood count (CBC) parameters which are useful markers of anaemia vary across population. Anaemia is highly prevalent in women of reproductive age in Sub-Sahara Africa, and the very high rate of maternal mortality in lowincome countries has been attributed to haematological complications such as anaemia and thrombocytopenia among other common causes. This study therefore, aims at exploring the result statistics of CBC parameters amongst a healthy population. Specific objectives are to evaluate the mean, median and range of Haemoglobin (Hb), Red cell count (RBC), Mean Corpuscular Volume (MCV), White Blood Cell Count (WBC) and Platelet (PLT) count using automated analysers and result validated with external quality assessment report. Their indicators were also used to analyse for the prevalence of anaemia, thrombocytopenia and thrombocytosis.
Methods: A retrospective, cross-sectional study was conducted on healthy non-pregnant women of reproductive age (18-40years), with normal chest X-ray and ECG report between 2020 and 2022. The samples were derived from archived databank that de-identified all personal data including requesting clinicians. A total of 252 data of eligible participants meeting the acceptance criteria were used in the final analysis.
Results: The mean, median and range of the haematological parameters were: Hb (g/dl) mean=10.6, median=10.6, range=4.8-13.3; RBC (x1012/l) mean=4.56, median=4.43, range=2.29-6.30; MCV (fl) mean=83.5, median=84.5, range=59.8-96.0; WBC (x109/l) mean= 5.5, median=5.3, range=1.9-17.5; PLT (x109/l) mean=203, median=193, range=85-1033. Using the WHO criteria for anaemia, the prevalence of anaemia in the population was 89.7% of which the defined moderate-anaemia was the predominant degree of anaemia (63.5%). The result further showed a 13.9% thrombocytopenia while thrombocytosis was at 0.8%.
Conclusion: A prevalence of 89.7% is high and although most of this fall within the moderate anaemia range, it is still a public health threat to women of reproductive age and thus could contribute poor maternal and foetal health outcomes. Furthermore, the high thrombocytopenia may also impact on pregnancy outcome if untreated. The values of haematological parameters from this study differ from values derived from non-African population as well some African countries, thus there is need to establish the reference range for Sierra Leone as this will give a better picture of the actual situation.
Abbreviations: CBC: Complete Blood Count; RBC: Red Cell Count; MCV: Mean Corpuscular Volume; WBC: White Blood Cell Count; EQA: External Quality Assessment; RML: RAMSY Medical Laboratories; RDW: Red Cell Distribution Width
Background
Complete blood count (CBC) is a routine haematological test in Medicine (Jacob [1]). It is also routinely performed in pregnancy (Kaur [2]) and is one of the most commonly requested laboratory tests (Bakrim, et al. [3]). Its parameters consists of red blood cell (RBC) counts, red cell indices, haematocrit, haemoglobin concentration, white blood cell (WBC) counts, WBC differentials and platelet (PLT) counts (Jacob [1]). CBC is a very important laboratory test because it helps not only in monitoring the sick but also in assessing the healthy (Bakrim, et al. [3]). It aids the diagnosis of anaemia, infection, some cancers, acute haemorrhagic states, allergies and immunodeficiencies, and in monitoring the adverse effects of drugs that cause blood dyscrasias (Jacob [1]). As (Mekonnen, et al. [4]), rightly put it, the information got from CBC not only guide additional investigations needed for monitoring and diagnosing the sick but also aids appropriate and timely management of the patients. Certain factors which can be pre-analytical or analytical, pathological or physiological like age, sex, height, environment, race, nutritional status, ethnic origin, lifestyle, biorhythms, consumption of alcohol or drugs, and pregnancy, can influence the values of CBC (Bakrim, et al. [3]), and these factors have to be considered when interpreting CBC laboratory results (Riley, et al. [5]). For instance, in reproductive age women, considered as women between the age of 15-49.99years (WHO [6]), significant variation has been observed in all haematological parameters in pregnant women as compared to non-pregnant control groups (Bakrim, et al. [3]).
According to WHO [7], anaemia is highly prevalent in women of reproductive age all over the world and continues to be highest in resource-poor countries. Anaemia and thrombocytopenia are recognized as one of the commonest causeof maternal mortality (Kaur [2]). In Sierra Leone, anaemia prevalence is high (Arinda, et al. 2014) and the rate of maternal mortality in Sierra Leone is among the highest in the world (Carshon-Marsh, et al. 2021).
Statement of the Problem
CBC parameters due to factors relating to sex, age, ethnicity, environment, etc differ from population to population (de Koker [8]), and in women of reproductive age, the values vary not only with age but also with pregnancy status of the woman (Bakrim, et al. [3]), yet, very few studies have been carried out on CBC in reproductive age women in Sierra Leone. In low-income countries, there is high rate of maternal mortality (WHO [8]) with Sierra Leone being one of the countries of the world with the highest rate. (Carshon-Marsh, et al. 2021). It has been observed that one of the most common causes of maternal mortality is haematological complications such as anaemia and thrombocytopenia (Kaur [2]), and some of these complications may be present prior to pregnancy but are only worsened by the stress of pregnancy (WHO [9]). Anaemia, though a global problem is more common in resource-poor nations because of the high prevalence of its causes such as malaria, HIV/AIDs, tuberculosis, hookworm infestation and schistosomiasis (WHO [6]). Sickle cell disease, with its associated severe anaemia, is also very common in Sierra Leone (Wurie, et al. [10,11]).
The high prevalence of anaemia in women of reproductive age in Sub Sahara Africa including Sierra Leone (Arinda, et al. [12]) has become a severe Publichealth problem (Wirth, et al. [13]). In Sierra Leone for instance, teenage pregnancy is very common with many (44.9%) adolescents experiencing child bearing by the age of 19years (Statistics Sierra Leone [14]), and adolescents are more at risk of presenting with anaemia at their first antenatal clinic visit (Bussink Voorend, et al. [15]). Because of the dramatic effects of anaemia in women of reproductive age namely increased risk of maternal and child mortality, families and communities are concerned about the health of women of reproductive age and screening these group of women for anaemia can help reduce the possibility of adverse pregnancy outcomes (Bussink Voorend, et al. [15]).
Aims and Objectives
Aim: To determine the values of complete blood count parameters in healthy non-pregnant women of reproductive age in Sierra Leone.
Specific Objective:
1. To determine the mean, median and range of haemoglobin, RBC, MCV, WBC and platelets in the study population.
2. To determine the prevalence of anaemia in women of reproductive age and categorise the anaemia by severity based on WHO criteria.
3. To determine the Public Health Significance of anaemia prevalence using WHO cut off values.
4. To determine the prevalence of thrombocytopenia and thrombocytosis in the study population.
Significance of the Study
Since haematological complications like anaemia and thrombocytopenia are among the most common causes of maternal mortality (Kaurs, et al. [2]), this study will help to demonstrate the need to initiate interventions towards reducing these haematological abnormalities in non-pregnant women of reproductive age in order to minimise associated adverse pregnancy outcomes.Reduction of anaemia in women of reproductive age by 50% by the year 2025 is one of the global nutrition targets for 2025 (WHO [16]). This study besides demonstrating the need to implement positive actions to fight anaemia, will also help Sierra Leone to assess how close the country is in achieving the target of halving anaemia in women of child-bearing age by 2025. This will help concerned bodies and organisations to strengthen or hasten their planned interventions.
The focus of the study is to determine the level of anaemia and its public health significance in a healthy female population within the reproductive age of 15-49 years using WHO criteria.
The scope of the review:
1. Exploring the definition and concepts of Blood specimen and Complete blood count
2. Review of the findings from previous studies on complete blood count, anaemia and abnormal platelet counts in women of reproductive age.
Definition and Concept of Blood Specimen and CBC
Blood Specimen: Blood is a body fluid that is made up of cellular elements (red cells, white cells and platelets) suspended in the liquid component called plasma. (Jacob [1]). The cellular elements of the blood continued Jacob, have a common origin – the haematopoietic stem cells in the bone marrow.
Complete Blood Count Parameters: Haemoglobin (HB) is said to be the marker of anaemia (Zeh, [17]) because anaemia is commonly defined on the basis of Hb (WHO [6]). Haematocrit (packed red cell volume), is the ratio of packed red cell to total blood volume, and long as the plasma volume does not change, the values of haemoglobin concentration and haematocrit correlates with the red cell mass. (Kumar, et al. [18]). Red cell count, that is, the quantity of RBC in the body, determines the amount of oxygen delivered to body tissues. (Jacob [1]). Red cell indices besides being used to classify anaemia as microcytic, normocytic, and macrocytic (the most useful method of classification) (Kumar, et al. [18]), is also helpful in identifying the nature of the primary defect and may even detect underlying abnormality before anaemia becomes obvious. (Hoffbrand [19]). According to (Kumar, et al. [18]), the most useful red cell indices are: Mean Cell Volume (Mean Corpuscular Volume, MCV), Mean Corpuscular Haemoglobin (Mean Cell Haemoglobin, MCH), Mean Corpuscular Haemoglobin Concentration (Mean cell haemoglobin concentration, MCHC) and Red cell distribution width (RDW). MCV is the average volume of one red cell measured in femtolitre (fl); MCH, the average mass of haemoglobin per red cell in pictogram (pg); MCHC, the measure in gram per decilitre (g/dl) of the average concentration of haemoglobin in a given volume of red cell, and RDW, the coefficient of variation in red cell volume (Kumar, et al. [18]). Reticulocyte count gives information about the erythroid activity of the bone marrow (Hoffbrand [19]). WBC count besides giving the total number of circulating leucocytes also gives the differential count where each of the white cells are enumerated. (Murphy, et al. [20]). Platelets count together with leucocyte count help to differentiate pure anaemia from pancytopenia that points at general marrow defect or destruction of cells such as in hypersplenism, and to identify the cause of anaemia. (Hoffbrand [19]).The clinical importance of CBC according to Hoffbrand [21], can be summerised as follows: Haemoglobin concentration and Pack cell volume (haematocrit) are indicators of anaemia or polycythaemia; Red cell indices especially MCV and RDW are key in classifying anaemia; RBC count increase in association with anaemia is characteristic of thalasaemia trait; WBC count and differentials helps in the diagnosis of infections, acute leukaemias and chronic lymphoid and myeloid disorders, and Platelets helps in detecting thrombocythaemia or thrombocytopenia.
Review of Previous Findings from Studies on CBC Anaemia and Abnormal Platelet Count in Reproductive Age Women
Within populations, variations relating to gender, age, ethnicity and environment are observed in haematological indices (de Koker [7]). Studies have shown significant differences in the values of CBC between men and women (Oloume, et al. [22]). Age related differences have been observed among people of same sex (Abiri, et al. [23]), and even among women of reproductive age the values vary depending on whether the woman is pregnant or not (Bakrim, et al. [3]).In a study conducted in China by Luo, et al. [24] among people living in high altitude, the CBC parameters including the RDW-SD & RDW-CV were found to change with increasing age in both men and women with each parameter showing a continuous increase or decrease, for instance, there was a gradual decrease with increasing age in the value of haematocrit in both men and women while the RDW-SD and RDW-CV increases with increasing age. In addition, with age in women, the WBC count, the neutrophils and lymphocytes increases. The pattern of change in haematocrit in a study conducted in Canada (Adel K [25]) was opposite of the China study- levels gradually increases with age. In Korea, study showed that before puberty, the RBC parameters increases but thereafter decreases with age (Nah, et al. [26]). Compared to Africans and Caucasians, Chinese population showed higher WBC, neutrophils, monocytes, RBC, Haemoglobin, HTC and RDW but lower platelets. (Luo, et al. [24]). A study conducted in Iran showed a decrease with increasing age in the mean concentration of haemoglobin in women, and, microcytosis and hypochromias were more prevalent in women of 36-45 years old (Abiri, et al. [23,27]). In their study in Central, Eastern and Western regions of Saudi Arabia, observed some gender, age and regional variations in some CBC parameters: the values of RBC, haemoglobin, and eosinophils differed with age; there was no gender or age variation in WBC parameters; there was a higher platelet levels in females and in those 40 years or older.
According to (Zeh, et al. [17]), in African populations, values obtained from most haematological parameters not only differ from that of Western population but also vary (though insignificantly) from one African country to another (Zeh, et al. [17]) Unlike non-African populations where the values of most haematological parameters in both genders showed a continuous change with age (Nah et al. [26,27]), in African population this difference was observed only in males while no significant age-related variation was noted in adolescent and adult female (Zeh, et al. [16]). In a study, the range of haemoglobin level in females in some West African countries such as Mali, Burkina Faso, Togo and Nigeriawas higher (12–13g/dl), than in East and Southern Africa (11.2–14.4g/dl). (Kone, et al. [28]). A study conducted in Blantyre Malawi showed a lower valuesof WBC, haemoglobin, haematocrit, MCV & platelet in adults compared to published values from Caucasian population. (Chisale, et al. [16,29] observed no gender or age variation in the absolute lymphocytes, basophils, eosinophils and monocytes counts. The results of many haematological parameters from a study in Yaoundé Cameroon correlated with that of other African countries but vary with that obtained from the countries in Northern hemisphere. (Oloume, et al. [22]). According to Miri Dshe, et al. [30], Kenyan and Ugandan references showed lower haemoglobin values and higher haematocrit values compared to the result they obtained from Nigerian population. In Liberia, haemoglobin and related haematology assays were found to be lower than the lower limit of United State range. (Kei, et al. [31]).
In studies conducted in Sierra Leone, the mean white cell count was found to be 5.0x109/l (range =2.4-12.0 x109/l) and showed no gender-related difference (Sahr, Hazra and Grillo (1995). The mean platelet count, the SD and the range were 197 x109/l, 25 x109/l and115-335 x109/l respectively (Gevao [32]). In the Sierra Leone studies just as in other indigenous African population, leucopenia was noted (Sahr, et al. [33]) and platelet count was lower than in Caucasians (Gevao [32]). Anaemia and thrombocytopenia are among the commonest causes of maternal mortality (Kaur, et al. [2]). Anaemia is very common in women of reproductive age worldwide and continues to be highest in resource-poor nations because of the high prevalence of its causes such as HIV/AIDS, tuberculosis, sickle cell disease, hookworm infestation and schistosomiasis (WHO [6]). In women of reproductive age, physiological changes such as menstruation, pregnancy and bleeding during child birth increase the risk of iron deficiency, and therefore anaemia (WHO [33]). Reduction of anaemia by 50% by the year 2025 is one of the Global nutrition targe set by WHO (WHO [15]) which has now been extended to 2030 (WHO/UNICEF [34]). Anaemia in non-pregnant women of reproductive age was defined by WHO [35] as Hb <12g/dl. Anaemia severity in non-pregnant women of reproductive age was categorized as: mild anaemia (Hb 11.0-11.9g/dl), moderate anaemia (Hb 8.0-10.9g/dl), and severe anaemia (Hb <8.0g/dl). (WHO [35]). Also, anaemia prevalence in a population was stratified as: no public health problem (prevalence ≤ 4.9%), mild public health problem (prevalence of 5.0-19.9%), moderate public health problem (prevalence of 20.0-39.9%) and severe public health problem (prevalence ≥ 40.0%) (WHO [18]).
Stevens, et al. [36] demonstrated anaemia prevalence of 30% globally, 13% in high income countries, 50% in southern Asia, 30% in Southern Africa, 31% in East Africa and 49% in West Africa. In all the cases above the degree of anaemia was mostly moderate followed by mild. The public health significance of anaemia in the above study was mild globally and in high income countries, moderate in southern and East Africa, and severe in Southern Asia and West Africa. In India Anaemia prevalence was 48.9% in 2014 (Verma, et al. [37]) and 64.32% in 2022 (Singh, et al. [38]). In both studies, the order of severity was moderate followed by mild. Also in the two studies, anaemia was a severe public health threat. Prevalence of anaemia was 20% (a moderate public health problem) in urban Parkistan (Qadir, et al. [39]) and 15.1% (mild public health problem) Iran (Abiri, et al. [23]). Anaemia prevalence in Africa vary from place to place. Anaemia was a moderate public health threat in East Africa with the exception of Rwanda where it was a mild public health problem (19.23%), and Mozambique and Tanzania where it was severe public health problem (53.98% and 44.83% respectively) (Teshale, et al. [40]). Liberia and Nigeria reported severe public health threat of anaemia prevalence (42% and 55% respectively) (WHO, GHO [41]). Previous studies conducted in Sierra Leone reported anaemia prevalence of 42.2% (Statiatics Sierra Leone [13]) and 44.8% (Wirth, et al. [12]) and the public health significance of anaemia was severe in both studies. Anaemia in both studies was largely mild while severe anaemia was uncommon (0.5% and 1.1% respectively). Very few recent studies have been conducted on abnormal platelet count in non-pregnant women of reproductive age. Results from closely related studies showed thrombocytopenia prevalence of 11.6% in women older than 20yrs (Alpert, et al. [42]) and 1.9% in those aged 18-29yrs and 2.6% in those between 30-39yrs (Blino, et al. [43]). Blino also reported the prevalence of thrombocytosis of 2.6% and 1.4% in those 18-29yrs and 30-39yrs respectively. In Saudi, the prevalence of thrombocytopenia and thrombocytosis were 0.16% and 6.34% respectively (Shaheen, et al. [27]). A study conducted in Malawi demonstrated 17.1% prevalence of thrombocytopenia (Chisale, et al. [29]). There is no recent data on prevalence of thrombocytopenia and thrombocytosis in in women of reproductive age in Sierra Leone.
Study Design
A retrospective cross-sectional descriptive study [44-52] of apparently healthy non-pregnant women of reproductive age who did CBC laboratory test between 2020-2021 at the study site as part of routine employment or immigration or scholarship check.
Study Setting
This study was conducted in RAMSY Medical Laboratories (RML) in collaboration with SYN LABS Medical laboratory in Ghana. RML is a fourstar certified laboratory that participate in quality management system according to ISO 15189-2015. It subscribes to international external quality assessment (EQA). It is located in Freetown, the capital of Sierra Leone with a branch in Bo, Southern district. The data is co-validated by SYN LABS medical laboratory, a fully accredited laboratory in Ghana and the haematological department subscribe to international external quality assessment.
Study Population
The study population was made up of non-pregnant women aged 15-49 years who had presented themselves for blood test at the requests of their institutions following approved medical investigations (including imaging exams) such as: chest x-ray, electrocardiography (ECG), blood pressure, blood sugar and pregnancy tests.
Sample Size
This is a retrospective study and focused on data recorded within a period of two years (2020 -2021). 252 women of reproductive age who presented at the study site within the stated period for the above mentioned reasons were recruited.
Sampling Technique
Data were extracted from archived, de-identified laboratory result forms of legible participants and input into Microsoft excel.
Inclusion Criteria
1. Women aged 15 to 49 years
2. Medical report from the medical exams which included pregnancy test, ECG, Chest X-ray, blood pressure, blood sugar, medical history such as hypertension and diabetes, and social history such as cigarette smoking and alcoholism.
Exclusion Criteria
All those that did not have normal medical report such as:
1. Positive pregnancy test
2. History of hypertension or diabetes
3. History of smoking or alcoholism.
4. Abnormal blood pressure or blood sugar.
5. Abnormal chest x-ray or ECG
Data Collection Management and Analysis
The variables collected were haematological parameters per age. The variables were input directly from laboratory result form into Microsoft excel and cross-checked for accuracy. The laboratory rechecked data entry with electronic database to ensure data quality before data was exported to SPSS (Statistical Package for Social Sciences) version 26 for analysis. The mean, median, range and standard deviation (SD) were determined for the haematological parameters. The following WHO criteria was used to stratify anaemia based on haemoglobin concentration into mild, moderate and severe, and to determine the public health significance of anaemia prevalence (Tables 1.1 and Table 1.2).
Ethical Consideration
The data was de-identified to ensure confidentiality. Ethical clearance was obtained from the ethics and scientific review committee, COMAHS USL.
A total of 252 women of reproductive age (15 to 49years) were enrolled in this study and all were included in the final analysis. The minimum age was 19yrs and the maximum 36yrs.The mean and median age of the whole population are 24.87 and 24.00 respectively. The participants were divided into three age groups (Table 2.1).
Haematological Parameters
The mean, median, range and standard deviation (SD) of RBC, HGB, MCV, WBC and PLT for the whole population and per age group are shown below (Tables 2.2 & 2.3. The histogram of the mean of each of the haematological parameters show normal distribution curve (Figures 1-6). depicts the mean per age group. For all the haematological parameters, age group 15-25yrs has the highest range while the 34-49yrs has the lowest. The mean WBC decreases from one age group to the next while the median increases. The mean and median RBC is lowest in age group 34-49yrs. The lowest mean Hb is found in those 15-25yrs.The mean MCV increases across the age groups. The highest mean PLT is found in those 15-25yrs.
Table 2.3:The Mean, Median, and Range of WBC, RBC, HGB, MCV, and PLT per Age Groups of Participants.

There is no significant correlation between age and the values of each of the haematological parameters (p value > 0.005). The scattered dot graphs of the relation and age and haematological parameters are shown in Figures 7-11. Basedon WHO criteria for categorizing anaemia by severity (see Table 3.1), the prevalence of anaemia in the study population and in the different age groups are shown in Table 2.4.
Only 10.3% of the participants had ‘no anaemia’, the rest (89.7%) had mild anaemia or worse. Moderate anaemia is the predominant anaemia (63.5%) while severe anaemia was uncommon (1.6%) and was seen only in those 18-25yrs of age. The presence of anaemia in 89.7% of the participants makes the prevalence of anaemia in this population a severe public health problem (≥40%) (Table 2.5). Mild or worse degree of anaemia was found in 91.1% of participants 25yrs and below, 86.8% those between 26 and 33yrs of age and 87.5% of those 34yrs and above. The commonest degree of anaemia in all the age groups was moderate anaemia while severe anaemia was noticed only in those 15-25yrs of age. This study also found varying degrees of thrombocytopenia (platelet count <150 x109/l) and thrombocytosis (platelet count >400 x109/l). The prevalence of thrombocytopenia and thrombocytosis are represented in Tables 2.6 & 2.7. Thrombocytopenia was present in 12.5% of participants 15-25yrs of age, 15.8% of those 26-33yrs and 25% of those 34yrs and above. There was an increase in prevalence of thrombocytopenia across the age groups. 60% of all cases of thrombocytopenia was from participants between 18 and 25yrs of age. Thrombocytosis was found only in 1.2% of those 34yrs and above and this was the only age group with thrombocytosis.
Table 2.6:Prevalence of thrombocytopenia (platelet <150 x109/l) and thrombocytosis (platelet >400 x109/l) in the study population.
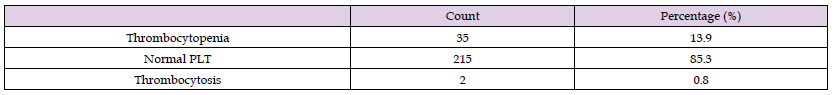
Note: 13.95% of the population has thrombocytopenia while 0.8% has thrombocytosis.
CBC parameters vary from one population to another (de Koker [7]). Studies have also shown that haematological complications like anaemia and thrombocytopenia are common causes of maternal mortality (Kaurs, et al. [2]). This study therefore, assessed the mean, median and range of haematological parameters as well as the prevalence of anaemia (based on WHO criteria), thrombocytopenia and thrombocytosis in the study population. The results of this study showed that significant proportion of participants have values of haematological parameters that are lower than established reference range with low Hb levels being the most common abnormal finding. The prevalence of anaemia (low Hb) in this study was 89.7%. The prevalence in the different age groups were 91.1% in those 25yrs and below, 86.8% in those between 26 and 33yrs of age and 87.5% in those 34yrs and above. Anaemia was thus most common in youngest age group. Moderate anaemia was the commonest degree of anaemia (63.5%) while severe anaemia was uncommon (1.6%) and was found only in those 25yrs and below. The contribution of each age group to the different degrees of anaemia decreases greatly across the age groups with age group 18-25yrs making to greatest contribution to all the degrees of anaemia severity. This pattern of relationship as well as the observation of severe anaemia only in those 25yrs and below may be largely due to the great difference in the number of participants in the different age groups (66.67% of the study population is between 18 and 25yrs while only 3.17% is greater than 33yrs old) which created a greater chance of obtaining abnormal values.
Anaemia prevalence in this study was higher than studies conducted globally, in Asia, in high income countries and in Africa (Stevens, et al. [37]), as well in India (Verma, et al. [38,39]), Pakistan (Qadir, et al. [40]), Mali (Armah-Ansah, 2023), Iran (Abiri, et al. [23]), East Africa (Teshale, et al. [41]), and in Nigeria and Liberia (WHO [8]). This differences may be due to normal geographical, ethnic and cultural variations. The prevalence obtained from this study was at least double the values reported from other studies conducted in Sierra Leone (Wirth, et al. [12,13]). This variation may be because the two studies (Wirth et al and Statistics Sierra Leone) were conducted in more diverse environments with varied environmental factors, dietary habits etc. Comparison of anaemia prevalence in different age groups in different studies was not possible because age groups are not homogenous in all studies, but anaemia seems to be most prevalent in the youngest age groups in different studies. In Sierra Leone for instance, anaemia prevalence was highest in age group 15-19yrs in the studies of Wirth et al, and in age group 18-25yrs in the present study.
In line with this study, moderate anaemia was the predominant anaemia found in India (Verma, et al. [38-40] and in Mali (Armah-Ansah, 2023). The severity of anaemia in many other countries including previous studies conducted in Sierra Leone was not in concordance with the findings of this study. Mild anaemia was the predominant anaemia reported by Steven, et al. [37] globally, in high income countries, in Asia and in different parts of Africa. Mild anaemia was also the predominant anaemia in Sierra Leone (Wirth, et al. [12]; Statistics Sierra Leone [13]). Severe anaemia was uncommon in this study as well as in almost all other studies. For instance, the prevalence of severe anaemia in Sierra Leone was 1.6% (present study), 1.1% (Wirth, et al. [12]) and 0.5% Statistics Sierra Leone [13]. Based on WHO criteria, anaemia in this study is a severe public health problem (that is, it is greater than 40%). This is in agreement with overall anaemia prevalence in Southern Asia and in West and Central Africa (Stevens, et al. [37]). Countries like India (Verma, et al. [38,39]), Mozambique and Tanzania (Teshale, et al. [41]), Liberia and Nigeria (WHO [8]) reported anaemia prevalence that was also a severe public health threat. Also in line with this study, anaemia was a severe public health threat in other studies conducted in Sierra Leone (Wirth, et al. [12,13]). The finding of anaemia prevalence that was a moderate public health concern globally, in East Africa and Southern Africa (Stevens, et al. [37]) and in Urban Pakista (Qadir, et al. [40]) was not in consistent with this study. Still very different from this study was the finding in high income countries (Stevens, et al. [37]), in Iran (Abiri, et al. [23]) and Rwanda (Teshale, et al. [41]) of anaemia prevalence that was a mild public health problem.The results of this study thus supports the claims that anaemia though a global problem is more common in resource-poor nations (WHO [6]); that there is high prevalence of anaemia in women of reproductive age in Sub-Sahara Africa including Sierra Leone (Arinda, et al. [11]), and that the prevalence of anaemia in Sierra Leone is a severe public health problem (Wirth, et al. [12,13]).
Thrombocytopenia and thrombocytosis were present in varying degrees in the study population (prevalence of 13.9% and 0.8% respectively). The prevalence of thrombocytopenia increased across the age groups. Age group 18-25yrs made greatest contribution (60%) to overall thrombocytopenia. The two cases (1.2%) of thrombocytosis were obtained from among participants aged 18-25yrs. This age group related findings may be in part due to the unequal distribution of participants in the age groups. Very few recent studies have been conducted on abnormal platelet count in non-pregnant women of reproductive age, therefore, result of closely related studies were included in the comparison. Alpert, et al. [43], obtained thrombocytopenia prevalence of 11.6% in women >20yrs in United States, a finding that is in line with this study. Blino, et al. [44] obtained a lesser degree thrombocytopenia: 1.9% in those aged 18-29yrs and 2.6% in those between 30-39yrs. In addition, Blino reported the prevalence of thrombocytosis of about 2.6% and 1.4% in those 18-29yrs and 30-39yrs respectively. This shows that in those 18-29yrs, thrombocytosis was more common than thrombocytopenia and that thrombocytosis was present in those 30yrs and above, but in the present study, thrombocytopenia was far more common in all age groups; however, the few cases of thrombocytosis in this study (0.8%) was seen in those 18-25yrs and this age group falls within the age group with higher thrombocytosis than throbocytopenia in Blino study.
Chisale et al in their study conducted in Malawi, obtained a higher prevalence of thrombocytopenia (17.1%) than this study. In a study conducted in Saudi on healthy population 18yrs and above (but with 96% of the study population less than 40yrs), thrombocytosis was more prevalent (6.34%) than thrombocytopenia (0.16%), a finding that is also not in line with this study. from this comparison, one can say that thrombocytopenia has no specific pattern of distribution because some non-African countries has a higher prevalence than some African countries and vise versa. There is no recent data on prevalence of thrombocytopenia and thrombocytosis in Sierra Leone. The mean, range and SD of the haematological parameters from this study are compared to previous documented reference ranges in Table 3.1. Themean of most of the haematological parameters from this study is lower than the mean of the other studies. The lower limits of the range of HB, WBC, RBC, HB, MCV & Platelet are also found to be lower than that of the other studies. A comparison of the mean and range of WBC and PLT in Sierra Leone studies is given in Table 3.2 below. From the table, the mean values of both WBC and PLT from the present study is similar to that of the other studies but for both WBC and PLT the range obtained in this study is far greater than the previous studies (especially the upper limits of the range).
Note however, that the study population differ to some extent in the three studies: the study of Gevao was conducted among adult females and that of Sahr was conducted among healthy population which included both males and females but there was no significant gender-related variation in the result. Therefore, the variations observed may be due to the differences in study population. Comparison of variations relating to age groups is not possible because age groups are not homogenous in all the studies. The results of this study showsno significant correlation between age and the haematological parameters, and this is consistent with studies conducted in some other African countries (Zeh, et al. [16]) but was not in line with some non-African studies (Nah, et al. [25,26]).
Conclusion
The values of complete blood count parameters from this study vary with values obtained from most non-African population as well as some African countries. There is no significant correlation between age and the values of haematological parameters. There is high prevalence of anaemia in the study population (89.7%) with moderate anaemia being the predominant anaemia (63.5%) while severe anaemia was uncommon (1.6%). Anaemia prevalence in the study population is a severe public health problem. Thrombocytopenia is present in significant amount in the population (13.9%).
Limitation
This study indicates that there is high prevalence of anaemia in women of reproductive but it failed to explore the contribution of demographic characteristics to anaemia prevalence. The study population was not diverse, therefore, the findings of this study may not be a perfect representation of reproductive age women in Freetown or Sierra Leone at large.
Recommendations
A prospective study is recommended in future research in order to involve a larger and more diverse population, and to be able to exclude other factors such as haemoglobinopathies, HIV/AIDS, etc., that may interfere with the values of haematological parameters so as to establish local reference interval of haematological parameters. This will help to minimise over diagnosis of abnormal blood count. From the results of this study, government and non-governmental organizations are invited to revisit the established strategies for reducing anaemia in women of reproductive age in Sierra Leone and to find new ways of achieving this aim in order to reduce the high rate of maternal mortality from haematological complications like anaemia. The Government of Sierra Leone has established targets to reduce maternal mortality to 650 per 100,000 live births, neonatal mortality to 23 per 1,000 live births and under-five mortality to 71 per 1,000 in the 2017-2021 National Reproductive, Maternal, Neonatal, Child and Adolescent Health (RMNCAH) strategy (MoHS, 2017). In view of this all related health parameters should be improved and as anaemia could pose a threat to the RMNCAH strategy, this study can serve a marker to provide information that could help in improving maternal health.


