Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Irma Nool1*, Mare Tupits1, Lily Parm1, Valentina Raudsepp1 and Marika Peralaan2
Received: December 20, 2023; Published: January 08, 2024
*Corresponding author: Irma Nool, Tallinn Health Care College, Kännu 67, 13418 Tallinn, Estonia
DOI: 10.26717/BJSTR.2024.54.008553
Purpose: to describe the quality of nursing documentation and nursing diagnoses in the nursing care clinic.
Methods: The sample was nursing records before and after the training of NANDA-I nursing diagnoses and
nursing documentation. Observational protocols were used to collect data. The D-Catch instrument was
used for structural assessment of the quality of nursing documentation. Nursing diagnoses were analyzed
qualitatively. The statistical package SPSS 26.0 program was used to analyze the nursing documentation
evaluated with the D-Catch instrument, the Mann ̶ Whitney U test was used to evaluate the differences before
and after the training.
Findings: Most nursing diagnoses were made in the areas of activity/rest and security/protection. The most
frequent nursing diagnoses were the risk for falls and the risk for impaired skin integrity. Evaluating the
quality of nursing records before and after NANDA-I nursing diagnoses training, it was revealed that there
were most inadequacies in the formulation of nursing diagnoses before the training and in the formulation
of results after the training. After the training, the formulation of nursing diagnoses and the documentation
of nursing interventions improved significantly, but the documentation of results deteriorated somewhat.
Conclusions: The results of the research show the necessity of training in improving the documentation of
nursing care.
Implications for Nursing Practice: This study gives insight into usage of nursing diagnoses in nursing care
clinic and the necessity of highlighting the importance of health-promoting nursing diagnoses.
Keywords: Nursing Records; Documentation; NANDA; Nursing Diagnoses; Quality
Nursing documentation is a document created in paper and/or electronic form that shows which patient-centered interventions the nurse has planned and performed. The documentation must reflect the decisions made in the nursing process and their necessity, interventions and assessment (Saranto, et al. [1-5]). Nursing documentation is an inevitable part of the treatment process and the purpose of the activity is to contribute to the treatment process. Documentation has legal significance for the protection of both healthcare professionals and patients. Therefore, correct documentation requires accuracy, making nursing care better and enabling confirmation of decisions made in patient treatment. Based on research, it can be argued that poor documentation is one of the factors that lead to undetected deterioration of the patient’s condition. Documentation should provide an overview of changes in health status as well as changes in medication [6]. Quality nursing documentation strives to foster structured, consistent, and effective communication among nurses and facilitate continuity and patient safety. It links nursing documentation directly to internationally recognized aspects of healthcare quality and patient safety [7]. The quality of nursing documentation meets seven criteria:
1) Is patient-centered,
2) Contains actual nursing work,
3) Reflects nurses’ clinical judgments
4) Is presented in a logical sequence,
5) Is written in real time,
6) Records changes in care, and
7) Meets legal requirements [2].
The task of high-quality nursing documentation is to achieve a continuous, structured and effective exchange of information between healthcare professionals, which results in consistent patient-centered nursing interventions [3]. The use of the NNN taxonomy in the provision of nursing care also increases patients’ satisfaction with the nursing care provided to them [8]. To ensure this, it should be properly and authentically documented. Nursing activities and documentation must be consistently directed, controlled and evaluated by the nursing manager [9]. Legislation regarding patient documentation varies from country to country, but should contain accurate and high-quality information for assessing, planning and providing nursing care. A common national model for documenting patient care would improve information flow, collaboration between multidisciplinary care teams, and patient safety [10]. Nurses spend about one-third of their working time documenting. Nurses’ weak knowledge of documentation methods can cause problems for both patients and nurses, and therefore a common basis for writing correct nursing diagnoses is needed for everyone [11]. A study conducted by the Estonian Health Insurance Fund revealed that nursing documentation in Estonia has improved over the years, but there are still shortcomings [12]. The main conditions in the nursing care clinic are dementia and stroke.
Among somatic disorders, the most common are diseases of the circulatory system, diseases of the nervous system (mainly Parkinson’s disease) and diseases of the musculoskeletal system (mainly osteoarthritis) [13]. They also often have high blood pressure, diabetes and cancer [14]. Related to this, patients in the nursing care clinic have a number of psychobiological needs such as body care, mobility, elimination, nutrition, circulatory support, neurological regulation, safety, and physical integrity. Psychosocial needs are also important and have the following indicators: communication, cognition, love, acceptance, self-actualization, emotional security and sociability [15]. Psychosocial aspects such as support network, description of emotions related to the health and illness process, use of coping strategies, and patient and family knowledge of treatment, as well as aspects related to sexuality, hobbies, and leisure activities, have been found to be partially documented or undocumented [16]. The purpose of the research is to describe the quality of nursing documentation and nursing diagnoses in a nursing care clinic.
Sample
In October 2018, an applied research was started at West-Tallinn Central Hospital in Estonia, first NANDA-I nursing diagnoses training was conducted for all nurses of the nursing care clinic. The nursing clinic has 130 beds, and at the time of the study, 52 nurses worked in the clinic, 38 of whom completed a two-day training in NANDA-I nursing diagnoses. The nursing clinic has 6 departments and the nurses working there received 16 hours of training. The training was conducted by three lecturers, with one of the trainers working at both the hospital and the university. The first eight hours dealt with the theoretical foundations of NANDA I, and the second eight-hour training included the analysis and joint discussion of the electronic nursing history prepared by each participant’s nurse. NANDA International II Taxonomy Nursing Diagnoses: Definitions and Classification 2015 – 2017 [17] in Estonian was used in the training. Since earlier versions of the book were also in use in the clinic, nursing diagnoses based on earlier versions were also considered correct. The sample was nursing records before and after training in NANDA-I nursing diagnoses and nursing documentation. Nursing records had to meet the following criteria: prepared for a patient who had been in the hospital for at least three days; the start and end dates of the patient’s case are between 3 months before and 3 months after the end of the training, and an individual nursing plan has been drawn up for the patient.
The data were extracted from the LIISA electronic information system used in West-Tallinn Central Hospital. The data was compiled from the part of the nursing history, which consists of the nursing history, the nursing plan, and the nursing diary. The nursing records were printed out and delivered to the researchers at the agreed time in the conference hall of West-Tallinn Central Hospital, where the analysis of the nursing records also took place. Before the training, 292 disease cases were obtained during the 4 months before the training, of which 276 met the criteria. Before the training, 54 nursing records were randomly selected in the nursing care clinic. After the training, 3 months after the training, a total of 246 disease cases were obtained within 4 months, of which 148 met the criteria and 47 nursing records. Were randomly selected.
Observational protocols were used to collect data. There were different observation protocols. Protocols 1 - 2 were tables where the researchers entered data from the nursing records before and after the training. The tables contained information on the following aspects: treatment case number, department, nursing diagnoses, related factors, defining characteristics, purpose, nursing interventions according to the nursing diagnosis, assessment, document reflecting the assessment. The third protocol contained the researchers’ individual assessments according to the D-Catch instrument, and the fourth protocol contained the consensus and sum scores based on the individual assessments. The D-Catch instrument contained six questions: record structure, admission documentation, nursing diagnoses, interventions, progress and outcome evaluation and legibility. All questions were assessed on a 4-point Likert-type scale. Admission documentation, nursing diagnoses, interventions, and progress and outcome evaluation were measured as a total score of quality and quantity criteria. The research question was given 1-4 points for quality and quantity, and the results were added together. The minimum result obtained by summing was 2 and the maximum was 8. Question structure and legibility were measured only based on the quality criterion and there was no summing. The quality criterion points were as follows: 4 – very good; 3 – good; 2– incomplete; 1– absent [18]. The D-Catch instrument allows assessment of nursing diagnoses according to the PES format, which includes P ̶ problem (nursing diagnosis name), E ̶ etiology (related factors), S ̶ signs and symptoms (defining characteristics) [19].
For qualitative analysis, nursing diagnoses were divided into problem-focused and risk diagnoses. Diagnoses were categorized according to NANDA-I Taxonomy II domains. The SPSS 26.0 program of the statistical package for social sciences was used for statistical analysis. The chi-square (χ2) test was used to compare percentages before and after training. The Mann ̶ Whitney U test was used to assess the difference in nursing records quality before and after training Mann ̶ Whitney U is a non-parametric test for comparing the arithmetic means of two groups. The test was chosen because the sample was not normally distributed. Differences where p<0.05 were considered statistically significant.
Permission to conduct the research was obtained from the author of the D-Catch instrument, the hospital and the Tallinn Medical Research Ethics Committee (decision no. 2742). In addition, confidentiality agreements were signed between the researchers and West-Tallinn Central Hospital. The study was conducted in a room allocated for this purpose by the hospital. The patient’s name and personal identification number were deleted from the nursing records. All nursing records were coded and the data of the nurses who completed the nursing records were deleted. The study results were generalized and the personal data of the patients and the nurses who completed the nursing documentation were not disclosed.
The related factors were partially present both before and after the training in almost half of the cases. There was a statistically significant difference in the presence of defining characteristics in the nursing anamnesis, where before training defining characteristics were present in less than a quarter of the nursing records and after the training in more than half of the nursing records (see Table 1). Problem- focused nursing diagnoses were established both before and after the training in a total of eight domains. Most nursing diagnoses were made in the field of activity/rest. The areas of self-perception, role relationships, sexuality and coping/stress tolerance were not addressed. Before the training, 28 different nursing diagnoses were formulated in different wording, which did not match the NANDA-I II taxonomy or were incorrectly worded. Some diagnoses were made several times, there were a total of 68 non-matching nursing diagnoses before the training. After the training, 7 different nursing diagnoses were made in different wording, a total of 9 different times, which did not match the taxonomy of NANDA-I II. Most often, different nursing diagnoses were combined into one or offered in the wording of the nursing diagnoses themselves (see Table 2). Risk diagnoses were established both before and after the training in a total of only five areas. Most risk diagnoses were established in the field of security/ protection.
Table 1: Documentation of related factors and defining characteristics in nursing records before (N=54) and after training (N=47).
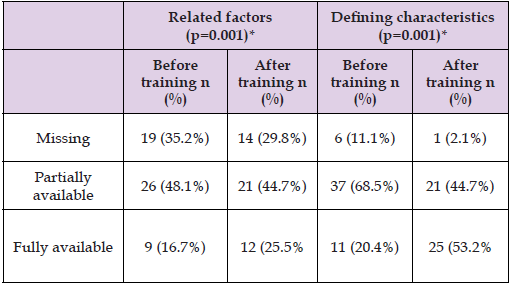
Note: *χ2-test
Note: * Nursing diagnoses that do not match the NANDA-I II taxonomy or are incorrectly worded.
Before the training, 22 different risk diagnoses were established in different wording, which did not match the NANDA-I II taxonomy or were incorrectly worded. Some risk diagnoses were established several times, in total there were 35 non-matching risk diagnoses before the training. After the training, 5 different risk diagnoses were established in different wording, which did not match the NANDA-I II taxonomy. Most often, when formulating risk diagnoses, the word “danger” was used instead of “risk” (see Table 3). Health promotion diagnoses were not found in any of the nursing records. Evaluating the quality of nursing records before and after the training and different parts of the nursing records in relation to their quality, it was revealed that before the training, the total score of nursing interventions (7.11±0.904), the quality of the structure of the nursing record (3.87±0.339) and the quality of legibility (3.83±0.376)) were the highest. and the lowest was the sum score of nursing diagnoses (6.11±1.110) and the quantity of nursing diagnoses (3.04±0.643). After the training, the quality of legibility (3.91±0.282), the quantity of nursing interventions (3.87±0.397) and the sum score of nursing interventions (7.60±1.035) were the highest, and the sum score (6.04±0.756), the quantity (3.06±0.791) and quality (2.98±0.725) of progress and outcome evaluation were the lowest. After the training, the quantity (p<0.0001), quality (p=0.002) and sum score (p<0.0001) of nursing diagnoses and quantity (p=0.015), quality (p<0.0001) and sum score (p<0.0001) of nursing interventions improved statistically significantly. The quantity of the results was slightly worse (p=0.009) (see Table 4).
Note: * Nursing diagnoses that do not match the NANDA-I II taxonomy or are incorrectly worded.
Note: *Mann Whitney U test
Patients in the nursing care clinic have a number of psychobiological needs such as body care, mobility, elimination, nutrition, circulatory support, neurological regulation, safety, and physical integrity. Psychosocial needs are also important and have the following indicators: communication, cognition, love, acceptance, self-actualization, emotional security and sociability [15]. The present study revealed that the most frequent nursing diagnoses were risk for falls and risk for impaired skin integrity the nursing care clinic. Also, the adult failure to thrive was documented 23 times before and once after the training, which after the training, as the nurses’ knowledge of nursing diagnoses increased, was replaced by the frail elderly syndrome. In a study conducted in Turkey, the most frequent nursing diagnoses in the nursing care department were ineffective role performance and ineffective health maintenance, and similar to our study, the risk for falls [20], which was also more frequent in (Dias, et al. [21]) study along with the risk for impaired skin integrity. In addition, Dias, et al. [21] point out the risk for pressure ulcer, obesity, risk for constipation and obesity, of which the risk for pressure ulcer and risk for constipation were documented to a small extent in the nursing records examined in this study. The frail elderly syndrome is also being talked about more and more and is one of the most frequent nursing diagnoses in nursing care clinic patients [21].
In their meta-analyses, (Zhang, et al. [22]) found evidence that the risk of mortality is higher among frail patients. In the nursing records reviewed in this study, frail elderly syndrome was one of the most frequent nursing diagnoses. Although a significant number of patients in the nursing clinic are bedridden patients, due to which there are problems with weight and constipation due to lack of exercise, the given nursing diagnoses were very little mentioned. Before the training, there were many inaccuracies in the formulation of nursing diagnoses, which improved significantly after the training. Apparently, the nurses were not used to using the NANDA-I nursing diagnoses book before the training or did not have the skills to use the book correctly, and several diagnoses were formulated by the nurses themselves or used diagnoses that do not appear in the NANDA-I II taxonomy. In a study conducted by Kocacal (Güler, et al. [20]), it was found that the most nursing diagnoses were established in the field of activity/ rest and safety/protection, and the least in the field of sexuality and life principles. This is consistent with the results of the present study. For problem-focused nursing diagnoses, eight domains were covered, and for risk diagnoses, only five domains were covered. Unfortunately, no health-promoting diagnosis was established.
Evaluating the quality of nursing records before and after the NANDA-I nursing diagnosis training, it was revealed that there were most inadequacies in the formulation of nursing diagnoses before the training and in the formulation of results after the training. (Tuinman, et al. [23]) and (Moldskred, et al. [24]) also concluded in their study that there were most inadequacies in nursing documentation when formulating nursing diagnoses and presenting results. This may indicate that standardized nursing language is not being used. After the training, the formulation of nursing diagnoses and the documentation of nursing interventions improved significantly, but the documentation of outcomes deteriorated somewhat. Here, the reason may be that training focused more on formulating nursing diagnoses than outcomes. In a study conducted by (D`Agostino, et al. [25]), it was found that both liability and structure were rated very low. However, in the present study, both structural components were rated very highly. The fact that the nursing documentation is electronic certainly contributed to the liability of the documentation, and nothing remained unclear due to illegible handwriting. The structure of the nursing record was also clear.
The nursing records were selected randomly before and after training and the nursing documentation of the same nurse has not been compared as researchers got anonymous nursing records without personal data of the nurse and patient. Although the sample was small, the results of the research can be generalized within the framework of one clinic, but not to all nursing care clinics in Estonia.
The results of the research show the necessity of training in improving the documentation of nursing care. Most nursing diagnoses were made in the areas of activity/rest and security/protection. The most frequent nursing diagnoses were risk for falls and risk for impaired skin integrity in the nursing clinic. No health-promoting diagnoses were established. After the training, the formulation of nursing diagnoses and the documentation of nursing interventions improved significantly. The study showed the importance of training in improving the quality of nursing documentation. Since nursing diagnoses are reviewed every two years, training is also necessary every two years to review changes in nursing diagnoses.
The continuing education is needed to have training on NANDA-I nursing diagnoses in every two years. More attention must be paid to health-promoting nursing diagnoses.
All authors have read and agreed on the final version of the manuscript. The first author was responsible for statistical analysis. In other parts of the article all authors contributed equally.
Authors thank the hospital for making the research possible.
The authors have declared no conflicts of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Permission to conduct the research was obtained from the author of the D-Catch instrument, the hospital and the Tallinn Medical Research Ethics Committee (decision no. 2742).


