Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Jia Yan Qu1, Jing Bo Lu1, Yang Yang Fu2, Cai Ping Meng1, Li Yuan Rong1, Yong Hong Shen1 and Zhi Ran Kang2*
Received: December 07, 2023; Published: December 18, 2023
*Corresponding author: Zhi Ran Kang, Tuina Department, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, China
DOI: 10.26717/BJSTR.2023.54.008512
Objective: To evaluate the quality of evidence and efficacy of acupoint massage for improving peripheral
sensation in DPN.
Methods: We independently searched 4 electronic databases, including Chinese National Knowledge
Infrastructure (CNKI), MEDLINE/PubMed, Embase, and Cochrane Library, for randomized controlled trials
(RCTs) about acupoint massage improving peripheral sensation in DPN from January 1, 2018, to December 31,
2022 (recent 5 years). The main outcome measures were total effectiveness and sensory nerves conduction
velocity (SCV), and Toronto Clinical Scoring System (TCSS). For the statistical analysis, the risk ratio, standard
mean difference, and 95% confidence interval (CI) were used to calculate effect sizes between groups. To
determine heterogeneity, statistical index I² was used.
Results: A total of 1790 DPN participants in 20 RCTs were included in this meta-analysis. The total effectiveness
showed that acupoint massage was more effective than the intervention of the control group for improving
MS [Ratio Risk (RR):1.25, 95% CI (1.19–1.31), P<0.00001]. SCV of common peroneal nerve and median nerve
showed that acupoint massage improves sensory function more than the control group [SMD=1.32, 95% CI
(1.17, 1.48), P<0.00001], [SMD=1.82, 95% CI (1.49, 2.15), P<0.00001]. We also found that acupoint massage
performed better than the control group in improving TCSS [SMD=-0.87, 95% CI (-1.41, -0.34), P=0.001].
Conclusion: Acupoint massage was effective for improving peripheral sensation in DPN. It is suggested to be
an appropriate nursing technique in treating paresthesia of DPN.
Keywords: Acupoint Massage; Nursing Technique; Diabetic Peripheral Neuropathy; Systematic Review; Meta-Analysis
Abbreviation: DPN: Diabetic Peripheral Neuropathy; TCM: Traditional Chinese Medicine; CAM: Complementary and Alternative Medicine; SCV: Sensory Conduction Velocity; VAS: Visual Analogue Scale
Diabetic peripheral neuropathy (DPN) is a complication of diabetes, which progressively damages the human nervous system. The prevalence of DPN is 425 million people in 2017 worldwide, and this number probably rises to 628 million by 2045, estimated by International Diabetes Federation [1]. DPN nearly affected half of people with diabetes [2]. It causes great morbidity and is related to increased mortality [3]. The most common form of DPN, distal symmetric sensorimotor polyneuropathy, causes dysfunctional sensory symptoms including pain, numbness, burning, prickling, or itching sensation that produce substantial influence on quality of life of patients, especially on sleep, mood, and functionality [4-6]. Currently, the core of the treatment for DPN is glycemic control [7]. In addition, pain management for DPN is another principle of treatment [8]. Studies discussed that drugs improve painful DPN, such as opioid analgesics, topical drugs, etc [9-11]. However, there are few guidelines on improving nerve conduction. Some studies have proposed the use of neurotrophic agents such as mecobalamin and lipoic acid, but the clinical effect still need to be debated [12-14]. Therefore, some thought that treatment of DPN is limited [15] Nursing technique can assist clinical treatment to promote health, maintain health, and prevent disease.
Currently, some nursing cares have been applied in DPN, such as hand-food exercise, balance training, supportive education, and selfcare practice, which play a good role in improving symptoms [16- 19]. In China, Traditional Chinese Medicine (TCM) nursing technique is a kind of nursing technique with unique characteristic. It applied TCM theories like Meridian and Channel theory, acupoint theory, and Yin-Yang theory that guide nurses to achieve TCM technique [20] At present, widely used TCM technologies include auricular acupressure, Chinese herb plastering, foot bath with decoction, etc [21-23]. Acupoint massage, as one of TCM Tuina techniques, is also a popular form of complementary and alternative medicine (CAM) worldwide. Studies show it gradually becomes mainstream of TCM nursing techniques [24,25]. Although it is used frequently to improve curative effect of controlling glucose level, acupoint massage has been clinically recorded in studies, demonstrating its ability to improve sensory function in DPN patients. After acupoint massage nursing, sensory conduction velocity (SCV) of common peroneal nerves and median nerves showed it is significantly higher than itself before and got better improvement than control groups [26].
Cheng LH, et al. [27] operated acupoint massage on limbs-acupoint such as Zu San Li [28], San Yin Jiao, [SP 6], Tai Xi (KI 2) and so on, and found improvement on TCSS, even better than control group [27]. In addition, acupoint massage can lower Visual Analogue Scale (VAS) scores and it is regarded useful to relieve painful DPN [29]. Although clinical studies of acupoint massage treating DPN is plenty enough, there is a lack of systematic and quantitative review or meta-analysis to summarize the effectiveness of acupoint massage on improving sensory function and analyze its definite efficacy for DPN. Also, potential mechanisms of acupoint massage have not yet been discussed. This study aimed to evaluate the quality of evidence and efficacy of acupoint massage for improving sensory function in DPN.
Search Strategy
This systematic review was registered with the PROSPERO database (CRD42023406010). This systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement principles, using the population, intervention, control, and outcomes (PICO) model. Two reviewers (JYQ and ZRK) independently searched the following electronic databases (one Chinese database and three databases in English): Chinese National Knowledge Infrastructure (CNKI), MEDLINE/PubMed, Embase, and Cochrane Library. Gray literatures and other unpublished studies were checked on OPEN GRAY and ClinicalTrials.gov. Searching terms for all the databases are displayed in (Tables 1-4). Then they checked titles and abstracts independently to filter studies satisfying the retrieval strategies from January 1, 2018, to December 31, 2022 (recent 5 years) without language limitations. Other authors selected all relevant articles and reached a consensus by discussion.
Inclusion and Exclusion Criteria
Selected articles were eligible if they fulfilled the following inclusion criteria:
1. Randomized control trials (RCTs) or randomized pilot studies, 2. Certainly diagnosed DPN participants, 3. The experimental group including the intervention of acupoint massage alone, 4. The control group that received basic clinical care or drug therapy while excluding any manual therapy, 5. Assessment mainly including SCV of median nerves and common peroneal nerves as the primary outcome, then total effectiveness, and TCSS as the secondary outcomes.
Assessment of Risk Bias and Quality of Evidence
Two authors (ZRK and JYQ) independently assessed the quality of each selected study using the version 2 of the Cochrane risk-of-bias tool (ROB-2) outlined in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (V6.3) for risk of bias [30]. The bias assessment was shown in five domains: randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome and selection of the reported result. The overall risk-of-bias judgement is divided in three levels: low risk of bias, some concerns, and high risk of bias.
Data Extraction
Based on our design, the characteristics and data of our research were assessed and extracted. Two authors (ZRK and CPM) independently extracted the following data from selected studies: first author and year, country, study type, patients characteristics (age, gender, amount, and disease duration), the protocol of experimental and control groups (length of each time, frequency, duration, and follow- up), and outcome measures.
Data Synthesis and Analysis
The analysis was run on the software Cochrane Review Manager 5.4 (the latest version). SCV and TCSS data were considered continuous data. We analyzed continuous data based on the standard mean difference (SMD). The total effectiveness was dichotomous data. For evaluation of dichotomous data, we used risk ratio (RR) and 95% confidence interval (CI). p-value <0.05 represented statistical significance. For the test of heterogeneity, p <0.1 represented heterogeneity between studies that had statistically significant differences. I2 tests were assessed for all outcomes in our research. We regarded I2 ≥75 as significant heterogeneity, I2 ≤50 as low heterogeneity, and I2 <75 but >50 as moderate heterogeneity. When the level of heterogeneity was moderate or low, we used a fixed-effects model. Otherwise, we used a random-effects model. If the heterogeneity was high, we prepared to run a sensitivity analysis and explained the potential reasons for heterogeneity. A funnel plot was established to explore possible publication biases if more than ten studies were in the analysis. Egger’s test was used to test the asymmetry of the funnel plot [31] We performed sensitivity analysis by putting aside one study at a time to ensure the robustness of the results.
Literature Search
In the initial database search, we detected 719 studies. After removing duplicate studies and any irrelevant articles by screening titles and abstracts, 69 studies were left for full-text checking. When reading the full text of these articles, 48 were excluded. 20 of them were not randomized trials or even just case reports; 13 of them focused on motor function of peripheral nerve, which did not match our research interest. A total of 9 studies did not use acupoint massage alone, and 7 studies lacked the outcome measure, total effectiveness, or SCV, or TCSS. At the end of the selection process, 20 studies met the inclusion criteria (Figure 1) [26-28,32-49] After assessing the Cochrane tool ROB-2, the condition of studies quality came out. (Figure 2) displays the overall quality of studies, which showed approximately 22.2% low risk, 66.7% some concerns and 11.1% high risk of Overall bias. Regarding bias of deviations from intended interventions, we had to consider that acupoint massage requires therapists to contact patients’ bodies with their hands; complete blinding of participants and personnel was impossibly done, so we gave ‘some concerned’ as assessor. All included studies perform well on bias of missing outcome data and measurement of the outcome. As shown in Figure 3, we saw that some studies had several items of high risk. Comparatively, Tian [42] and Zhu [39] got a bad performance on bias of deviations from intended interventions, which rarely displayed information about intervention [39-42] and Zhang [43] got a good grade which owned four low risk of bias, while Liang [48] and Huang [26] only had two low-risk items [26,28,43].
Patient Characteristics
There were 1790 DPN participants in 20 RCTs (Table 5). In total, 892 people were from the experimental group, which received acupoint massage, and another 898 were from the control group, accepting basic clinical care, and MeCobalamin tablets. Also, 963 participants were male, while 827 participants were female. In terms of age, the study of Tian et al had the oldest participants, in which the experimental group age was 69.21±3.11 years, and the control group age was 69.67±3.05 years [41]. Huang et al.’s study had the youngest participants; the experimental group age was 52.03±9.87 years, and the control group age was 51.24±10.27 years [26]. And Hou et al did not present age of patients [34]. The disease duration in all included studies was no more than 20 years, but Lin et al and Wang Wei et al. did not display patients’ duration of disease [40,46]. Zhang [43] had the shortest duration of disease, in which experimental group was 1.42±0.34 years while control group was 1.51±0.38 years [42]. Zhou et al had the longest duration, in which experimental group was 20.08±3.14 years while control group was 20.17±3.32 years [36].
Intervention Characteristics
All included studies used acupoint massage in the experimental groups (Table 6). Twelve studies applied massage on distal limbs mostly [26,27,31-34,36,37,45-48]. While the other eight focused more on head and face acupoints [35,38-44]. As for the control group, most studies used Mecobalamin tablets, which is a form of vitamin b12 suggested to benefit in improving nerve conductivity and neuropathic symptoms [50]. Lin [40] and Yang [47] only applied hypoglycemic drugs without detailed names and doses [39,46]. Cheng, et al. [27,42] and Wang Wei [38] also provided neurotrophy drugs for patients, still, without detailed information [27,43,46]. Alone Zhou [37] used health care as the control group intervention [37] The duration of a single treatment session was from 15 to 60 minutes. Wei, et al. [22,34,42] and Wang F [41] did the longest single session (60 mins) [32,33,41,42]. As for frequency of acupoint massage, most studies did 7 times per week (1 time/d). A few researches such as Lin [40] and Zhu [39] operated massage 21 times a week (average 3 times/d) [38,39]. Two studies performed intervention 14 times a week (average 2 times/d) [34,35]. In terms of total time, three studies lasted for 2 months, [44,45,48] while the others lasted for half a month or a whole month. Most of all studies only made an instant observation after treatment rather than at follow-up, except for one study that completed a 4-week follow-up [48].
Efficacy of Acupoint Massage: Total Effectiveness
Effectiveness is a way for clinical research to judge the effect of the Traditional Chinese Medicine intervention. It is divided efficacy into four levels: cured, highly effective, moderately effective, and poorly effective. Total effectiveness included the first three levels, and the calculation formula was ((cured+highly effective+moderately effective patients)/(total patients)×100%), which was based on the Criteria of Diagnosis and Therapeutic Effect of Diseases and Syndromes in Traditional Chinese Medicine [51] Fourteen studies used total effectiveness to explore the efficacy of interventions, and we put the post-intervention data into a meta-analysis. [26,32-44] The meta-analysis showed no significant heterogeneity (I2=0%, p=0.55). The fixed model was used. The results showed that the differences between acupoint massage groups and control groups were statistically significant [RR: 1.25, 95%CI (1.19,1.31), p<0.05] (Figure 4). Sensitivity analyses implied no significant change when any study was removed.
Peripheral Sensory Neural Conduction: SCV
Myelin and axonal damages are two major lesions in DPN [52] As a part of nerve conduction study parameter, SCV mainly shows the myelin sheath function of sensory nerves [53] Thus, SCV is a good indicator of DPN and may be useful as an objective parameter in research studies. In our research, SCV of median nerve was used to assess sensory conduction of upper limbs, while SCV of common peroneal nerve for lower limbs. Five studies including 425 patients used median nerve SCV to assess sensory nerve conduction of DPN patients [37,38,45-47] The heterogeneity between studies was moderate (I2=52%, p=0.08). We used the fixed model. The results showed that after analyzing post-intervention data, acupoint massage was significantly more effective than the control in improving the upper limbs sensory nerve conduction [SMD=1.82, 95% CI (1.49, 2.15), p<0.00001], (Figure 5). And eight studies including total 812 patients applied SCV of common peroneal nerve to evaluate lower limbs nerve conduction [26,37,38,41,42,45-47] The heterogeneity between studies was low (I2=40%, p=0.11). We used the fixed model. The results showed that acupoint massage was significantly better than the control group in improving the lower limbs sensory nerve conduction [SMD=1.32, 95% CI (1.17, 1.48), p<0.00001], (Figure 6). Sensitivity analyses implied no significant change when any study was removed.
Overall Condition: TCSS
TCSS was established in 2001 by Perkins et al, for screening DPN and assessing severity of the disease [54,55]. The score systems is made up by three parts including symptom scores, reflex scores, and sensory test score. Six items is in symptom scores for evaluating, and one point will be got for each item appearance. Reflex scores consist knee and ankle test, reduced reflex meaning 1 point while normal reflex meaning 0 point. Sensory test scores include five sense tests (abnormal for 1 point, normal for 0 point) [55]. Six studies including 389 DPN patients used TCSS as the assessment. [27,35,40,41,48,49] Meta-analysis showed high heterogeneity in the included studies (I2=84%, p<0.00001); a random model was used. So, we conduct a sensitivity analysis by removing one study (Lin [40]), then we recalculated the combined estimate on remaining studies. The results of heterogeneity became stable after we ran the sensitivity analysis (I2=52%, p=0.08). The differences were statistically significant between acupoint massage and control groups, implying that acupoint massage was more effective in improving the overall condition of DPN patients [SMD=-0.61, 95% CI (-0.93, -0.29), p<0.05] (Figure 7).
The systematic review and meta-analysis evaluated the efficacy of acupoint massage for improving function of sensory nerves in DPN patients by total effectiveness, upper and lower limbs SCV, and TCSS. After the screening and selecting process on four major literature databases, 20 studies met the inclusion criteria, and we included them in the meta-analysis. The publication year of all studies was from January 1, 2018, to December 31, 2022 (recent 5 years). There were 20 RCTs. The intervention of the experimental group was acupoint massage, while that of the control group was drug therapy (Mecobalamin or hypoglycemic drug) and health care. The test of homogeneity and several statistical tests were run in the meta-analysis. In total, 1790 people with DPN were included. To evaluate efficacy and improvement of peripheral sensory function in included DPN patients, we used total effectiveness to see comparation of therapeutic efficacy between two groups, SCV to achieve sensory conduction assessment, and TCSS to compare overall condition between acupoint massage group and control group. 14 studies used the total effectiveness, [26,32-44] 8 studies used SCV of common peroneal nerve, [26,37,38,41,42,45-47] 5 studies applied SCV of median nerve, [38,39,46-48] and six studies chose TCSS [27,35,40,43,48,49]. Most studies collected instant outcome instead of a follow-up, except for one study, which had a 4-week follow-up [48] The meta-analysis results showed that acupoint massage had significantly better efficacy than the control group (p<0.05).
It is important to mention that the standard of levels division
of total effectiveness was based on the outcome measure (OM) that
the study chose and the calculation between baseline and post-intervention
scores. The calculation formula of the standard was
baseline post 100%
baseline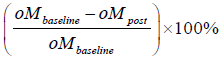 . A percentage <20% was regarded as poorly effective,
a percentage ≥20% but <50% was defined as moderately effective,
a percentage ≥50% but <85% was defined as highly effective,
and a percentage ≥85% was defined as clinically cured [51] Then we
could calculate total effectiveness based on the number of patients at
each level. Considering that all studies came from China, this method
of evaluating the efficacy of TCM therapy was chose because of its
popularity in Chinese clinical trials rather than in other areas worldwide.
However, its accuracy and comparability would be influenced
by the choice of OM. To sum up, researchers could not guarantee the
consistency of the OMs used in their total effectiveness. We, therefore,
do not recommend that researchers use total effectiveness in
their clinical trials. If necessary and unavoidable, please use a unified
standard measure to calculate total effectiveness as much as possible.
Results of the meta-analysis showed that acupoint massage was
more effective in improving SCV than the control group intervention
(p<0.05), suggesting that acupoint massage could be related to myelin
sheath reparation and protection. The curative mechanism of
acupoint massage was ever discussed. Some researchers thought that
effect on sensory neuron receptors and interaction between themself
and acupoint massage could be a possible proof. After all, massage
was operated on surface of body, on which distributed thousands of
receptors.
. A percentage <20% was regarded as poorly effective,
a percentage ≥20% but <50% was defined as moderately effective,
a percentage ≥50% but <85% was defined as highly effective,
and a percentage ≥85% was defined as clinically cured [51] Then we
could calculate total effectiveness based on the number of patients at
each level. Considering that all studies came from China, this method
of evaluating the efficacy of TCM therapy was chose because of its
popularity in Chinese clinical trials rather than in other areas worldwide.
However, its accuracy and comparability would be influenced
by the choice of OM. To sum up, researchers could not guarantee the
consistency of the OMs used in their total effectiveness. We, therefore,
do not recommend that researchers use total effectiveness in
their clinical trials. If necessary and unavoidable, please use a unified
standard measure to calculate total effectiveness as much as possible.
Results of the meta-analysis showed that acupoint massage was
more effective in improving SCV than the control group intervention
(p<0.05), suggesting that acupoint massage could be related to myelin
sheath reparation and protection. The curative mechanism of
acupoint massage was ever discussed. Some researchers thought that
effect on sensory neuron receptors and interaction between themself
and acupoint massage could be a possible proof. After all, massage
was operated on surface of body, on which distributed thousands of
receptors.
Touching and pressing-related receptors were considered as the most relative receptor with mechanical force form massage [56] For instance, Pacinian corpuscles and Meissner’s corpuscles, two rapidly adapting receptors, are sensitive to quick touch, blowing, vibration, and two-point discrimination [57,58] In terms of slowly adapting receptors, Merkel’s cell and Ruffini corpuscle could encode stimulus of the location where mechanical force loads [59,60] The matter thing is that all these receptors are linked with Aβ fibers, which are responsible for conducting stimulus signal from outer force. Another theory presented that acupoint massage was related to nerve reparation. Wu found that massage could accelerating the process of axon regenerating, leading to myelin sheath recovering [61] Meanwhile, the researcher also found proliferation of Schwann cells after massage treatment on rats’ peripheral nerves. Schwann cells would wrap axon up and secreted nerve growth factor to help myelin sheath grow [62] In Traditional Chinese Medical theory, function of sensation relies on fluent flow of Qi and Blood. TCM theory guiding massage therapy (or say ‘Tuina’) was mainly Meridian, Channel, and Acupoint theory. We TCM thought an essential substance called “Qi” flowed and moved in meridians and channels. The flow of “Qi” made up essential functions of the human body, such as motor function. Many functions are affected when the flow of “Qi” is blocked or deficient.
Acupoints, which were gates regulating flow of “Qi” running from inside to outside and were also reflection spots of diseases or trigger points of massage therapy, were on the route of meridians and channels. Thus, we could use massage to contact meridians and acupoints to regulate the flow of “Qi”; then, the dysfunctional situation would be improved. In our included studies, some of them operated massage on distal limbs acupoints. For example, Peng et al. choose HT-1, LU-5, LI-11, LI-4 and PC-8 as the upper limbs acupoints, and SP-12, ST-36, GB-34, SP-6 and ST-41 as the lower limbs acupoints, then both SCV of common peroneal nerve and median nerve became significantly better after treatment than control group [45] After TCSS was meta- analyzed, results showed significant difference between acupoint massage and intervention of the control group for improving overall condition of sensory function (p<0.05). However, the heterogeneity of TCSS between the two groups was high (I2=84%). We conducted a sensitivity analysis by removing one study at a time. Then the level of heterogeneity became stable when Lin [40] was removed. Restricted to the amount of data, we did not perform a subgroup analysis, but after we flipped the article from head to toes, we inferred that duration of the disease and frequency of massage treatment could be the source of heterogeneity. Lin [40] did not give details about duration of disease in characteristics of DPN patients, while other five studies showed an exact number about duration.39 Duration of a disease could reflect severity and how long patients suffer from DPN. If they did not provide any information about it, then it was a risk in meta- analysis. As for frequency of massage, the author reported a frequency of 21 times per weeks (average 3 times per day). Compared with the other five studies, this frequency seemed to be a little longer, as well as time length of single treatment. Comparatively long time of treatment usually meant much stimulus, which could make the data of curative efficacy unstable under meta-analysis. Additionally, more follow-up is needed in future studies. We should not only focus on the instant effect of massage but also care about its long-term efficacy.
Acupoint massage improved sensory function of peripheral nerves better than the control intervention in terms of the total effectiveness, SCV of median nerve and common peroneal nerve, and TCSS. More standardized and normalized RCTs are needed to make the meta-analysis more accurate and valuable.
Z.-R. Kang made substantial contributions to the conception or design of the work. J.-B. Lu achieved data acquisition of the work. J.- Y. Qu made contribution to data analysis and interpretation. J.-Y. Qu drafted the work or revised it critically for important intellectual content. C.-P. Meng, Y.-Y Fu, L.-Y. Rong and Y.-H. Shen agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors approved the final version to be published.
The authors declare that they have no conflict of interest.
This article was supported by Outstanding Young Talents Project (RY411.34.02) from Shanghai Nursing Association, Reserve TCM Talents Project (RY411.40.04) from Shanghai University of Traditional Chinese Medicine, and Traditional Chinese Medicine Scientific Project (2022QN087) from Shanghai Municipal Health Commission.
All data generated during this study are included in this published article.


