Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Yi-Syuan Lai1* and Li-Chi Chiang2
Received: December 01, 2023; Published: December 13, 2023
*Corresponding author: Yi-Syuan Lai, Department of Nursing, Tri-Service General Hospital, China
DOI: 10.26717/BJSTR.2023.54.008502
The study aims to achieve knowledge translation in nursing for pressure injury care. The caregivers of patients with pressure injuries and their family can benefit from translating knowledge, attitude, and practice, and they can have more knowledge related to pressure injuries, and learn how to react to and care for patients. In this way, it will be possible to promote wound healing and prevent recurrence of pressure injuries. This study is a randomized controlled trial. There are seventy participants. The experimental group receives care plans in which knowledge translation is applied, and the control group receives usual care. After twelve-week intervention, the caregivers significantly increase their knowledge, attitude, and practice related to pressure injuries. During the intervention, the patients have better wound healing. The recurrence, rehospitalization rate, and death rate are significantly reduced after the intervention. (p<0.05). The care plans with knowledge translation and wound follow up will be offered in order to avoid infection or deterioration caused by poor circulation and to reduce patients pain and the recurrence. The caregiver’s knowledge, attitudes and practice on pressure injuries prevention are promoted. The patients can have effective wound care. This study can be a reference for pressure injury care in the future.
Keywords: Pressure Injury; Caregiver; Knowledge Translation
Pressure injury meaning to lie down (lying down), refers to a localized injury to the skin or subcutaneous soft tissue, usually located on a bony prominence or in contact with an iatrogenic device Related, it can develop within 2 to 6 hours (Kosiak, et al. [1]). Studies by Strazzieri-Pulido, et al. [2] and Griswold et al. (2017) indicate that the length of hospitalization and nursing time of patients with pressure injury diseases also increase by 10%. The number of patients also increased by 1.5%, and the number of days spent in the intensive care unit increased by 4 to 30 days, which also reduced the quality of life and increased pain, recurrence rates and procedures (Black, et al. [3,4]). Studies indicate that 95% of pressure injuries are preventable (Waterlow [5,6]). The cost of treating pressure injuries is very expensive (Tariq, et al. [7]), and the cost of treatment is 2.5 times the cost of prevention (Nuru [8]). Tsao, et al. [9] Literature Analysis Caregivers spend more than 17 hours a day caring for patients. Today's clinical pressure injury care includes providing health education sheets, routine turning over forms every two hours and reminders to turn over, and providing wound dressing methods before discharge. They only inform that turning over and wound care are important for pressure injuries, but they are not. There is little understanding of the care problems of the primary caregiver and the causes of pressure injuries.
The caregivers discuss care needs and methods with each other and provide care measures without considering the patient's preferences and family economic status. Most of them use command-style requirements to turn over and use Standardized information is provided for health education. The occurrence of pressure injury itself is not terrible. What is terrible is that patients or caregivers despise the prevention and care of pressure injuries, which subsequently leads to high mortality due to infection and sepsis. Pressure injuries are clinically found. The actual amount of care a person receives is far less than the need for care. In addition, the patient has low autonomy or high dependence (Latimer, et al. [10]). Also, because of the high dependence of pressure injuries, the patients main care. The target of care is even more important. Most of the nursing guidance for pressure injuries at home and abroad is designed for professional medical personnel, and less attention is given to caregivers. Caregivers are the people with whom pressure injuries need to get along day and night after returning home, so pressure injury knowledge will be formulated. Translate the nursing guidance plan and provide appropriate nursing guidance based on the individual needs of the patient and the caregiver, so that the problem can be solved with the right medicine.
Physical Health Needs of Stressed Consumers and Caregivers
The injury to the patient from a pressure injury to the pain of the wound feels very much like someone biting you, and the body feels like it lacks flesh, making it painful when someone touches or cares for you (García-Sánchez, et al. [11]). After the formation of a pressure injury, it has a significant impact on the patient's quality of life. The pressure injury causes one or more negative emotions in the physical, psychological and social aspects of the patient, and is prone to painful symptoms in life, such as pain, Exudate and odor (McGinnis, et al. [12]), long wound recurrence time, loss of function, increased chance of infection and early warning, unexpected surgery causing loss of function and independence (Reilly, et al. [13-16]). At the psychological level, stress injuries will occur depression, anxiety, tension or stress. In terms of social costs, stress injuries will increase economic expenses (Reilly, et al. [13]). For caregivers, patients with pressure injuries need care, such as turning over, changing wound dressings, equipment required for care (decompression equipment, wound dressings), reducing the caregiver's rest time, patients with pressure injuries requiring hospitalization, financial pressure on caregivers, and Unemployment caused by long-term absence from work will significantly increase the burden faced by caregivers and significantly reduce the quality of life (Rodrigues, et al. [14,16]). The physical and mental image and social problems of the caregiver, the back and forth caused by their own sleep, time, finances, equipment, treatment, etc., are all events that both parties may face and need to deal with.
Pressure Injury Patient/Caregiver Risk Factors
Based on systematic literature review, the risk factors for pressure injury include: older age, diabetes, cardiovascular disease/circulation, multiple diseases, spinal cord injury, incontinence, long operation time, long hospital stay, lower braden risk scale score, fracture, For the use of medical equipment, the above are irreversible factors; BMI is too high or too low, higher temperature, malnutrition, multiple pressure injuries, limited activity, friction/shear, infection, are modifiable factors as follows:
1) Age: each additional year increases the risk of hospitalization by 2.1% P =0.0002 (Huang et al., 2016). The risk increases 2.3 times for those aged 60-84 years compared with those under 60 years old (Strazzieri-pulido, et al. [2]); >70 years old HR = 2.17, P= 0.021, 95% CI: 1.12-4.2 (Artico, et al. [17]), >75 years old P<0.007, odds ratio (OR): 1.05 (Borsting, et al. [18]).
2) Three or more disease diagnoses: Patients with three or more diagnoses have a higher risk of pressure injuries than the average person, OR=1.98~3.18 (Ni, et al. [19,20]). Diabetic patients have a higher risk of pressure injuries than the general population, OR=1.07~5.58 (Frankel, et al. [18,21-23]). Cardiovascular disease/circulation RR=1 (Kumta, et al. [24,25]).
3) Spinal cord injury: Patients with spinal cord injury have a higher risk of pressure injuries than the general population, OR=1.4~16.8 (Frankel, et al. [18,26]); patients with high-level spinal cord injuries have a higher risk, OR=2.81 (Grigorian, et al. [27,28]).
4) Incontinence: Incontinent patients have a higher risk of pressure injuries than the general population, OR=3.27, 95%CI=1.32จ3 (Theaker, et al. [29]).
5) The longer the operation time: RR=1.19 for operation time >5 hours (Kumta, et al. [24]).
6) Long hospitalization >14 days, >10 days in intensive care center: the longer the hospitalization, the risk of pressure injury is higher than that of the general population. OR: 1.008 (Tayyib, et al. [30-32]).
7) The lower the Braden scale score: score <19 points OR=1.3-6.89 points, the patient has a higher risk of pressure injury than the general population (Frankel, et al. [21,22]).
8) Use of medical equipment: ventilator use >72hrs has an OR of pressure injury risk of 23.604; oxygen nasal cannula, BiPAP, nasogastric tube, tracheostomy, endotracheal tube, and plaster are 2.1 times more likely (Cox [33]). Fracture cast use P=0.04, OR=5.2 (Allman, et al. [34]).
9) B M I is too high or too low: < 1 8 . 5 O R : 2 . 7 - 4 . 0 1 ; B M I > 2 4 O R : 1 . 0 4 (O' Brien et al. [18,23,35]).
10) Infection: People with pressure injuries were more likely to have nosocomial infection (45.9% vs. 20.1%, P=0.001) and other hospitalization complications (86.5% vs. 43.0%, P<0.001) (Allman, et al. [36]), OR: 4.39, 95%CI:6.92จ25 (Yepes, et al. [37]). An increase in body temperature of 1-2กใC, risk of pressure injury OR=3.519; body temperature >38.5กใC; OR=0.2 (Nijs, et al. [38-40]).
11) Malnutrition: Low Albumin: higher risk of pressure injury, OR: 11.6 (Efteli [41]). Albumin decreases by 1g/dl, OR: 3.0 (Allman, et al. [34]).
12) Multiple pressure injuries: >= 2 or more p=0.029 (Rodrigues, et al. [14]).
13) Activity limitation: dependent than independent activity p=0.005, OR=2.1 (Sayar, et al. [32]), OR: 2.96-30.2 (Nijs, et al. [30,38]). Because you need the help of others in daily life, the friction/shear force will increase.
The National Pressure Ulcer Advisory Panel [42] proposed a pressure injury prevention guideline project. According to the European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance [43], interventional measures are divided into: risk assessment, skin and tissue Assessment/Preventive Skin Care, Nutritional Assessment and Treatment, Turning and Early Mobility, Surface Support/Device-Related Pressure Injuries, Pressure Injury Assessment and Monitoring, Pain Assessment and Treatment, Cleansing and Debridement, Wound Dressing, Non-Surgical Treatment, Cleaning, surgery, health professional education, multimedia tools, technology-hybrid care models, combined care categories, comprehensive databases, review all literature titles and outline content, and collect relevant articles that can assist guidance for discussion and analysis.
This study is a randomized controlled trial. The participants are chosen from the burn center and the plastic surgery department in one of the northern medical centers in Taiwan. We categorized the participants by using match random sampling into experimental group and controlled group. Figure 1 Case collection flow chart. Studies and analysis are done by the researcher single-blind studies which evaluates knowledge translation in nursing on patients with pressure injury for wound healing stages, recurrence of pressure injury, readmission rate and mortality caused by pressure injury, and a caregiver's knowledge, attitude, and the results of the care. The experimental group has received knowledge translation in nursing for pressure injury care with precaution teaching plan by using self-designed teaching materials, manuals, videos, multimedia tools (power point, LINE official account, LINE one-on-one lesson, virtual lesson), in-person assistance and assessment. The controlled group maintained the regular nursing intervention. Before providing interventions, we collected every participants' basic information from both experimental group and controlled group (the main caregiver filled in the information, if a participant was unable to do), wound assessment (size, depth, color, discharge types, and odor), the pretest of pressure injury and physiologic index variables (blood pressure, body mass index, serum albumin). The above collection data can be a benchmark for evaluating the outcome of intervention.
We gave posttests after 6-week, 12-week of intervention and 12 weeks after the end of the intervention to check the changes of the wound, recurrence of pressure injury, readmission rate and mortality rate, and a caregiver's knowledge, attitude and skills. The main caregivers of patients with pressure injuries are the objects of health education, educating them on pressure injury care methods and precautions. Because pressure injuries are caused by the pressure caused by the unchanged posture and the weight of the body, resulting in damage to the skin or subcutaneous soft tissue, pressure The occurrence of sexual injuries will cause pain to patients, increased length of hospitalization, repeated admissions and increased mortality; caregivers will feel self-blame and increase their physical and mental load. There are already methods to prevent pressure injuries in guidelines and literature, but pressure injuries continue to occur in homes, institutions, and hospitals. The author found that caregivers do not know how to prevent and care for pressure injuries, nor do they understand pressure injuries. It will affect the safety of the patient after it occurs, so this article will provide care checklist related to pressure injuries, understanding of signs of infection, skin inspection methods, wound dressing steps, turning steps, and nursing guidance on nutritional establishment, and follow-up tracking of wound changes to avoid recurrence of the wound. Deterioration caused by infection or circulatory obstruction can reduce the patient's pain, thereby reducing the recurrence of pressure injuries.
Caregivers can improve pressure injury prevention knowledge and skills and become more comfortable in care. This study focused on patients with pressure injuries and their primary caregivers in the orthopedic surgery ward of a medical center in northern Taiwan. The inclusion criteria for the cases included
a. Pressure injuries of 1-3 degrees as determined by medical staff,
b. Patient needs There are caregivers,
c. Patients and caregivers, who must be over 20 years old,
d. Informed consent for this study (if the patient is confused, the consent form can be filled out by family members),
e. Caregivers understand the content of health education (MMSE) >24 points);
Exclusion conditions include
a. The patient has >3 disease diagnoses,
b. Is diagnosed by a physician as a terminal patient or has a life expectancy of <3 months,
c. Has an acute life-threatening problem (active bleeding site, Acute myocardial infarction, acute bronchitis, etc.),
d. Pressure injury caused by invasive tube placement,
e. Need to wear a non-invasive positive pressure respirator,
f. Need to stay in an intensive care center for a long time (>10 days),
g. Patients who require long-term operations, each operation requires >5 hours,
h. The caregiver has dementia,
i. The caregiver has mental illness or alcohol and drug addiction,
j. No caregiver.
The number of subjects in the study was estimated with reference to a similar study by Almeida Medeiros, et al. [40] and using G-power 3.1 statistical software. The statistical method used two groups of data comparison analysis method (Mean: Difference between two independent means [two group]). Set the effect size to 0.5, the second type error to 0.05, the power to 0.8, and the distribution ratio of the two groups to 1. The calculated number of samples is 52, and the expected attrition rate is about 20%. The total number of cases is expected to be 70, with 35 in the experimental group and 35 in the control group. Figure 1 Case collection flow chart.
There was no significant difference in the demographic characteristics of caregivers and pressure injury patients between the experimental group and the control group. Table 1 Basic demographics of patients, Table 1 Basic demographic attributes of caregivers. Among the number of patients with recurrence of pressure injury 3 months after intervention, a total of 53 (75.7%) patients had no recurrence of pressure injury after 3 months, and 17 (24.3%) patients had recurrence of pressure injury 3 months later. , a total of 35 (50%) patients in the experimental group h ad no recurrence of pressure injury after 3 months, and 0 patients had recurrence of pressure injury after 3 months; a total of 18 (25.7%) patients in the control group had recurrence of pressure injury after 3 months. Pressure injury did not reoccur, but 17 (24.3%) patients had reoccurrence of pressure injury after 3 months. The chi-square test p=0.00001 between the two groups showed a significant difference between the two groups. The control group was the relative risk RR of the experimental group (relative risk) value: 1.94, 95% confidence interval (95% CI) is 1.41-2.68, indicating the recurrence rate of pressure injury in the control group after 3 months. It is 1.94 times higher than that of the experimental group, as shown in Table 2. Among the number of patients who were readmitted to the hospital due to pressure injuries 3 months after intervention, a total of 57 (81.4%) patients were not readmitted to the hospital due to pressure injuries 3 months later, and 13 (18.6%) patients were readmitted due to pressure injuries 3 months later.
Table 1: Baseline clinical characteristics of 296 COVID-19 patients in Hospital Universitario Fundación Santa Fe
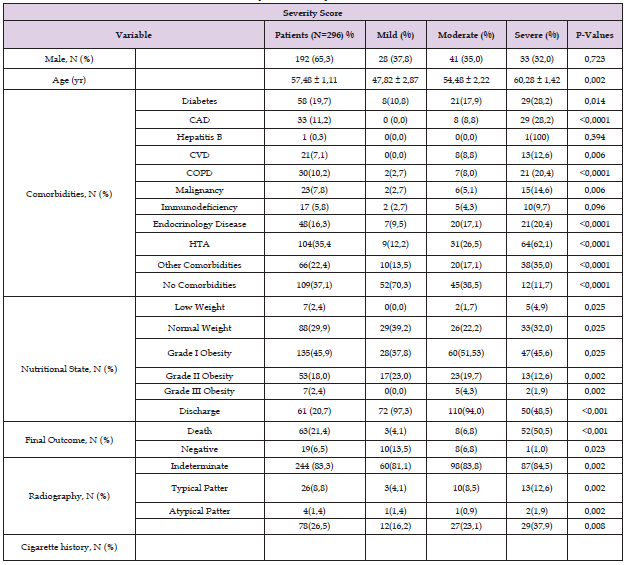
Note: Data are presented as the mean ± SD or N (%). Abbreviations: CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CVD,Cerebro vascular disease; HTA, Hypertension.
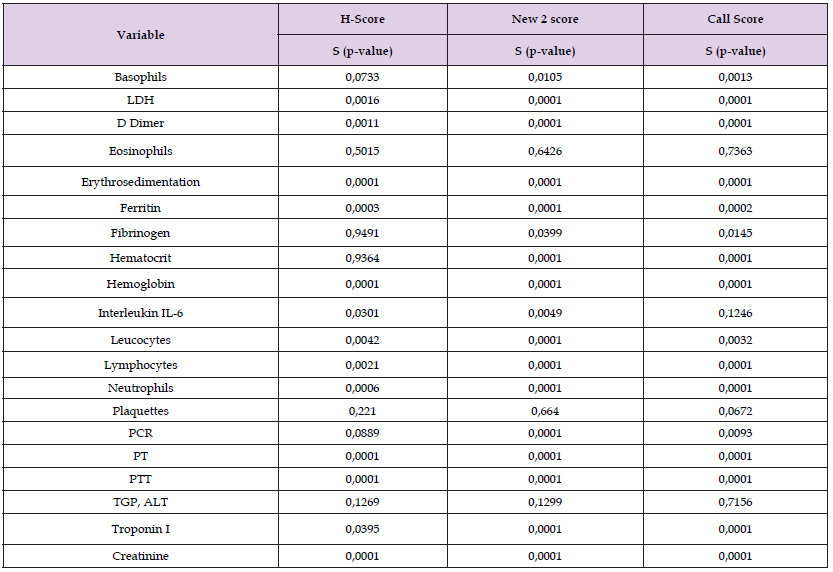
Table 2: Multinomial logistic analysis, spearman correlation score, between severity classification and laboratory parameters.
In terms of rehospitalization, a total of 35 (50%) patients in the experimental group were not rehospitalized due to pressure injuries after 3 months, and 0 patients were rehospitalized due to pressure injuries after 3 months; a total of 22 (31.4%) patients in the control group were rehospitalized. The pressure injury did not reoccur after 3 months. However, 13 (18.6%) patients had reoccurrence of pressure injury after 3 months. The chi-square test of the two groups showed that p=0.00001 showed a significant difference between the two groups. The control group was the experimental group RR. Value: 1.59, 95% confidence interval is 1.23-2.05, indicating that the readmission rate due to pressure injury in the control group after 3 months is 1.59 times higher than that of the experimental group, such as Table 2. Among the patients who died 3 months after intervention, a total of 61 (87.2%) patients died at 3 months. No death occurred after 3 months, and 9 (12.8%) patients died after 3 months. A total of 34 (48.6%) patients in the experimental group did not die after 3 months, and 1 (1.4%) patient died after 3 months; control group A total of 27 (38.6%) patients in the group did not die after 3 months, and 8 (11.4%) patients died after 3 months. The chi-square test of the two groups showed p=0.012, showing a significant difference between the two groups. The relative risk RR value of the experimental group: 1.26, 95% confidence interval 1.04-1.52, which means that the mortality rate of the control group after 3 months is 1.26 times higher than that of the experimental group, as shown in Table 3.
Note: Abbreviations: ALT, alanine aminotransferase; aPTT, activated partial thromboplastin time; AST, aspartate aminotransferase; CI, confidence interval;CRP, C-reactive protein; LDH, lactate dehydrogenase; OR odds ratio; TnI, troponin i
In this study, patients in the experimental group who received "Nursing Guidance on Pressure Injury Knowledge Translation" had a lower recurrence rate of pressure injuries three months after the intervention (RR: 1.94) and a lower admission rate due to pressure injuries compared with patients in the control group. (RR: 1.59), mortality rate was reduced (RR: 1.26), and all reached significant differences (p<0.05). In a project article on improving the incidence of pressure injuries, Liao et al. (2021) analyzed that the reasons for the high incidence of pressure injuries among inpatients are that there is no suitable "nursing guidance" provided to foreign domestic helpers, and the caregivers do not know how to turn over, position, and care. Patients have insufficient knowledge on pressure injury prevention, etc., and the above reasons are used to establish medical personnel education and training, pressure injury care guidance leaflets and videos, and turning assistive tools to reduce the rate of pressure injury. The results of this study are similar to this study, and nursing guidance is recommended. Able to provide individual pressure injury care guidance to patients, caregivers and families. One article reported a total of four hospitalizations within 10 months after the last healing of a third-degree pressure injury wound to the sacrum (Zhang, et al. [44]).
According to Lyder et al. [23,45], patients with pressure injuries are more likely to be readmitted to the hospital within 30 days after discharge, odds ratio OR (Odds Ratio) = 1.33, The occurrence of pressure injury was significantly associated with an increased risk of in-hospital death OR=3.94, and the 30-day in-hospital mortality OR= 2.18. A sample of 5,000 patients from a tertiary hospital in Seoul, South Korea, reviewed 5.6 years of cases. The in-hospital mortality rate of pressure injury patients was 3.94 times higher, while the in-hospital mortality rate of pressure injury patients aged 65 and above was 4.09 times higher. The length of time patients were admitted to the intensive care unit, the intensive care unit readmission rate of pressure injury patients was 57.1% (OR: 2.57), and the emergency department readmission rate was 35% (OR: 1.70) (Han, et al. [45]). A Japanese literature review from 1 to 4 years found that the average wound healing time was 18.4 days (9-37 days), and the recurrence rate of pressure injuries was 37.5%, the number of recurrence days is 41-745 days, and 25% of patients with recurrent pressure injuries die within 2 months (Kuwahara, et al. [46-51]); the risk of mortality within 30 days after discharge for pressure injury patients is 2.81 (95%) CI =2.44-3.23), hospital cost comparison P<.001) [52-53], the hospitalization time with pressure injury is longer than that without pressure injury (20.9 days vs. 12.7 days, P = 0.0001) (Allman, et al. [36]), the above The research results of the article all show that the occurrence of pressure injuries will increase the number of days of hospitalization, hospitalization expenses, and recurrence of pressure injuries. rates, readmission rates, and mortality.
In 2003, a pressure injury is listed as one of the indicators of care quality in clinical setting by Taiwan joint commission on hospital accreditation. That reflects that a pressure injury is a significant heath care issue. Nowadays, it still constantly happens at hospitals, home, and nursing homes: Pressure injuries cause pain, and increase length of hospital stay, rehospitalization rate, and death rate. In current clinical practice, standardized guidelines and basic principles are followed for pressure injury management, and it is found that most of the caregivers are unsure about what are the consequences of having pressure injuries and how to manage and prevent them. Therefore, the caregivers are more passive, and feel nervous and confused. In literature, there are guidelines for pressure injury prevention and management. However, they are primarily designed for heath professionals. As a result, to achieve evidence-based practice and knowledge translation, I hope to make individual management plans for each patient, provide caring support, and follow up with patients. And caregivers can benefit from knowledge, attitude, practice, and caring effect.


