Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Gilberto Cruz Arteaga1*, José Antonio Zamudio Gonzalez2, Elizabeth López Rojas1, Alejandra Rojo Coca1, Cristian Mercado Esquivel1, Mónica Adriana Pineda Gutiérrez1, Mario Alberto Huerta Manzano1, Raúl Gutiérrez Cruz1, Olivia Guadalupe Villanueva Martinez1, Arturo Andrade Sanchez3, Elsa Susana Nava1, Katya Barrera Espinosa1, Mirna Edith Jiménez Núñez1, Casandra Mikal Bueno Hernández1, Daniela Leticia Castañon Sánchez1, Carlos Alejandro Martínez Avalos1, Ariadna Elizabeth Vega Rocha4, Dulce Josselyne Pérez Alanis4, Augusto de Jesus Sanchez Arriola1, Alma Italia Guerrero Martínez5, Macedonia Guadalupe Moreno Tovar1 and Marilu Tzompa Robles6
Received: November 24, 2023; Published: December 06, 2023
*Corresponding author: Gilberto Cruz Arteaga, Medical specialist in Family Medicine, Family Medicine Specialist, Family Medicine Unit No. 20, Calzada Vallejo No. 675, Col. Nueva Vallejo, CP 07750, Gustavo A. Madero Delegation, Mexico
DOI: 10.26717/BJSTR.2023.54.008486
Donation is the act of giving an organ, tissue, or cells of oneself to another person who needs it with the purpose of improving their state of health. This process involves medical, social, psychological, ethical and economic aspects. The main factors that motivate the population of our country to donate organs are reciprocity, ethics, and morality, while the obstacles to carrying out this donation are the lack of education and awareness on the subject, myths and questions about the safety of the procedures, as well as the Catholic religion and the belief that organ donation can cause the death of the donor.
Objective: The objective was measure the validation and reliability of the instrument “Determining factors of organ donation in beneficiaries of the Family Medicine Unit (UMF) No. 20”.
Material and Methods: An instrument was carried out on a sample of 200 beneficiaries of the UMF No. 20 OOAD Norte of the IMSS in Mexico City, who agreed to answer the instrument, with prior informed consent. Content validity was evaluated by four experts, construct validity by means of exploratory factor analysis (the Kaiser-Meyer-Olkin (KMO) sample adequacy test and Bartlet's sphericity test) and confirmatory factor analysis (using the maximum likelihood estimation procedure) and reliability with Cronbach's alpha coefficient.
Results: The instrument presented Cronbach's alpha of 0.911, KMO of 0.731 and Bartlett's sphericity test < 0.05, obtaining two dimensions in the instrument: Social and Cultural. Confirmatory Analysis with expected values in Chi-square x2 31.98; PCMIN/DF 1.99; RMSEA 0.071; CFI 0.983; NFI 0.996 and TLI 0.970.
Conclusions: The instrument presented adequate validity and reliability with a clear and interpretable structure.
Keywords: Organ Donation; Validation; Reliability
According to the World Observatory of Donation and Transplantation corresponding to the year 2021, 144,302 solid organ transplants were performed, increasing 11.3% more than in 2020, of these 38,156 were from deceased donors from the region of the Americas [1]. In Mexico, 2,142 solid organs were transplanted in 2021, representing 3.68% of transplants on the American continent. The State of Mexico and Mexico City lead organ donation with 368 and 362 donations, respectively [2]. The most frequently performed transplants are cornea, kidney, liver, and heart [3]. The Mexican Social Security Institute (IMSS) performs 54% of all transplants performed in the country and has established itself as the health institution with the highest productivity [2]. Various factors have been reported as determinants that hinder the acceptance of organ donation [4], such as the social factor, which considers lack of education, awareness on the subject (deceased donor, brain death, cardiac death) [5-8]. and fear of donating due to myths, presenting donations from people who died in 2022 due to cardiac death of 1,564 and 443 due to brain death; the ethical-moral factor is considered that the donor family and society need to have maximum trust, requiring the authorization of the donor or the parties who make the decision [9,10]. In some countries, the declaration of the donor by will, presumed consent and donor card is legislated [11]. Advance directives are regulated in Mexico City with participation ages between 61 and 80 years and predominance of women [12], however, there is also the will to not want to donate organs [13]; the cultural factor is directly related to the population's acceptance or not of this action.
In countries like Spain and Colombia, there is dissemination through media such as television, however, health personnel have little information that motivates them toward an attitude. favourable in organ donation [14,15], In Mexico, the scarce donation is reported with little knowledge to follow procedures and procedures for donation [16], with lack of advertising campaigns 81.2%, followed by lack of trust in the health system 48.2%, ignorance of the donation process 47.5% and religious beliefs 42.2% [17]; In the economic factor, there are studies carried out in North America referring to transplant expenses that a family can have, fluctuating from $2000.00 to $4410.00 dollars [18] and expenses per donated organ [19], however in Mexico the trade of organs is prohibited, although there are no effective mechanisms to supervise and to punish those who engage in this illegal activity [20-22], foundations have been created that encourage health personnel to donate organs for transplant. Fernández-Rioja, et al. [23]. designed an instrument in Peru with the purpose of measuring their attitude towards organ donation in health personnel.
The instrument consisted of 24 questions divided into 4 dimensions:
(1) Economic
(2) Social
(3) Ethical-Moral
(4) Cultural
with a Cronbach's alpha of 0.771. Jasso, K et al. [24] designed in Mexico an instrument of 21 questions to measure “Attitudes towards Postmortem Organ Donation” taking as inclusion criteria the population of 31 of the 32 states of the country, who had knowledge of organ donation for transplants, with a Cronbach's alpha of 0.87. The objective of the study is to measure the validation and reliability of the instrument “Determining factors of organ donation in beneficiaries of the Family Medicine Unit No. 20 Vallejo”.
A cross-sectional, prolective, analytical study was carried out, validating an instrument. In beneficiaries of the Family Medicine Unit No. 20, belonging to the Deconcentrated Administrative Operation Organ (OOAD) D.F. North of the IMSS in Mexico City. The eligible population was of both sexes, aged 20 to 59 years, with voluntary participation in answering the instrument, prior acceptance of informed consent. Beneficiary personnel who did not wish to participate in the research and/or who did not have the time to answer the instrument were excluded.
Instrument
An instrument was developed with a total of 16 evaluation questions, grouping them into 4 factors: social, ethical-moral, cultural, and economic. Each factor with different number of questions 6, 3, 4 and 3 respectively. To evaluate the acceptance of organ donation, resulting in the measurement finding, a Likert-type scale was used, which measures the responses as follows: Totally disagree 1 point; Disagree 2 points; Undecided 3 points; Agree 4 points and Strongly agree 5 points. Once the instrument format was ready, it was exposed to a first evaluation by experts in organ donation (1 ethicist, 1 psychologist, 1 family doctor, 1 sociologist), where changes were made to the formulation of the instrument, followed by the corresponding modifications; evaluation of each factor grouping them into “Agree”, “Undecided” and “Disagree”, as follows; Social: Maximum score of 30, classifying as “agree” with 24-30 points, “undecided” with 13-23 points and “disagree” below 12 points. Ethical Moral: Maximum score of 20, classifying as “agree” with 16-20 points, “undecided” with 9-15 points and “disagree” below 8 points.
Cultural: Maximum score of 20, classifying as “agree” with 16-20 points, “undecided” with 9-15 points and “disagree” below 8 points. Economic: Maximum score 15, classifying as “agree” with 12-15 points, “undecided” with 7-11 points and “disagree” with less than 6 points. Of the total of 16 items that we have, a total of 85 points will be obtained, evaluating as agree with organ donation when meeting 68 to 85 points, undecided from 35 to 67 points and disagree below 34 points. For the evaluation of the instrument, a validation sheet will be used, for the approval or rejection of the questions formulated in the instrument (1 ethicist, 1 psychologist, 1 family doctor, 1 sociologist), with the following items: clarity in writing, internal coherence, response induction (bias), appropriate language with the level of the informant and whether it measures what it intends. To calculate the participants of the instrument, a necessary sample size (significance with an alpha of 0.05, power of 80% and standard errors with an assumption twice greater than the conventional correlation coefficients) of 200 participants was made, associated with the significance of factor loadings of 0.4 [25].
Analysis of Data
Descriptive statistics were performed to obtain frequencies and percentages in the demographic characteristics (sex, age, education, religion, marital status) of the 200 participants beneficiary to the U.M.F. No. 20 Vallejo. In content validity, the agreement of the evaluation of the item under review reported by each of the experts was carried out through the judgment of 4 experts. The degree of agreement between experts will be determined using the Fleiss Kappa coefficient, where: <0 poor agreement, 0.01-0.20 slight agreement, 0.21-0.40 acceptable agreement, 0.41-0.60 moderate agreement, 0.61-0.80 considerable agreement, 0.81-1.00 almost perfect agreement. Reliability was evaluated using the result of Cronbach's alpha coefficient where results were less than 0.5: unacceptable, 0.5- <0.6: poor, 0.6- <0.7 questionable, 0.7 to <0.8 acceptable, 0.8- <0-9 good and greater than or equal. 0.9 is excellent. Construct validity was analysed through the existence of high correlations between the variables through Bartlett's sphericity: with values returned by x2 (chi-square) obtaining significant values as they are less than 0.05 and a confidence level of 95%, and the Kaiser-Meyer-Olkin Index (KMO), taking into account values that fluctuate between 0 and 1, with an acceptable value > 0.5, If KMO ≥ 0.9, the test is very good; notable KMO ≥ 0.8; median for KMO ≥ 0.7; low for KMO ≥ 0.6; and very low for KMO < 0.5. Therefore, it is considered that factor analysis should be performed if it is greater than 0.5; Bartlett's test of sphericity (acceptable value less than 0.05) [26]. Likewise, the extraction of the factors was obtained using the orthogonal rotation method, varimax if it has low correlations < .7 and/or oblique, direct oblimin if it has high correlations > 0.7.
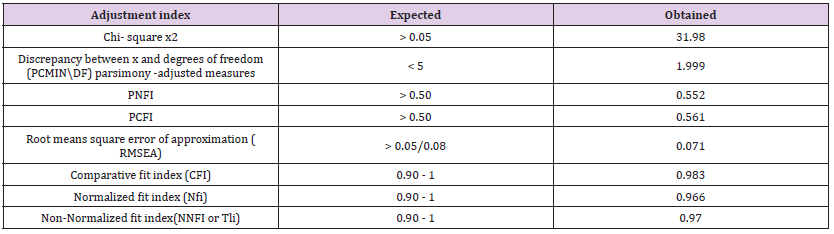
The procedure was repeated as many times as necessary until a stable factor structure was obtained. Items that had a factor loading less than 0.40 or that were not theoretically related to the factor were eliminated. Confirmatory factor analysis was performed using the maximum likelihood estimation procedure. The minimum standards of the fit indices were, namely: Chi-square X2 with expected > 0.05; Discrepancy between x and degrees of freedom (PCMIN/DF) < 5 ; Parsimony- Adjusted Measures (PNFI and PCFI) > 50; Root Mean Square Error of Aproximation (RMSEA) < 0.05/0.08; Comparative Fit Index (CFI) 0.90 – 1; Normalized Fit Index (NFI) 0.90 – 1; Non-nromalized fit index (NNFI or TLI) 0.90 – 1((Byrne, 2010; Hu y Bentler, 1999); The Hoelter statistic to check whether the sample size provided an adequate estimate of the model fit, determining a minimum cut-off point of 200 (Byrne, 2010). Statistical analysis of the data was carried out using the SPSS 26.0 statistical program for Windows.
Validation
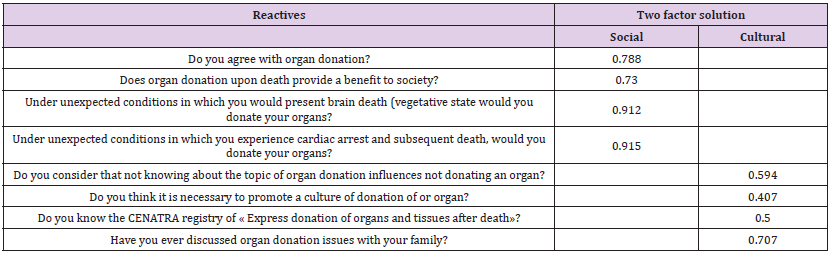
The instrument of determining factors in the acceptance of organ donation was applied to 200 beneficiaries of the U.M.F. No. 20 Vallejo, with predominance of female sex 64% (n=128), age group 20 to 39 years 52% (n= 104), high school education with 37.5% (n=75), Catholic religion 71% (n=71%) , single marital status 42% (n= 84) (Table 1). Scale reliability. Consistency . The total instrument with 16 questions had an initial Cronbach's alpha coefficient of 0.764, which indicates acceptable internal consistency (Table 2). The corrected total element correlation values in Table 2 present items with non-optimal values (≥ 030), so 5 questions were eliminated after the final consensus, presenting a total instrument with 11 questions with a Cronbach's alpha coefficient. of 0.911, which indicates excellent internal consistency (Table 3). In construct validity, a principal components analysis with orthogonal rotation was carried out because the correlations between items were between .3 to .5. Items that were not grouped into a factor with factor loadings greater than .4, that were grouped within a theoretical factor different from the one proposed, or that were not grouped into a factor that had at least three items were eliminated. In the final solution, eigenvalues greater than 1 showed the existence of two factors. This solution converged in five iterations and explained 58.29% of the variance. The items have factor loadings greater than .40 within their factor and communalities greater than .25. The final instrument was made up of 8 items that are presented in (Table 4). Bartlett's test of sphericity was significant , acceptable (929.01, df = 28, sig < 0.000) ; and the Kaiser-Meyer-Olkin sample size adequacy indicator was medium (.731). The alpha of the total instrument was 0.65. The measures adjusted for parsimony for the instrument of determining factors in the acceptance of organ donation were suboptimal given the modification indices proposed three covariances between the error terms of four items (Figure 1). The final model showed expected fit indices: x2 /df = 31.98, RMSEA = .071, CFI = .983, and NNFI = .970, Hoelter statistic of 200 (α = 0.01), with adequate sample size (Table 5).
Table 1: Demographic Characteristics of the instrument determining factors in acceptance of organ donate from the U.M.F. 20 Vallejo.
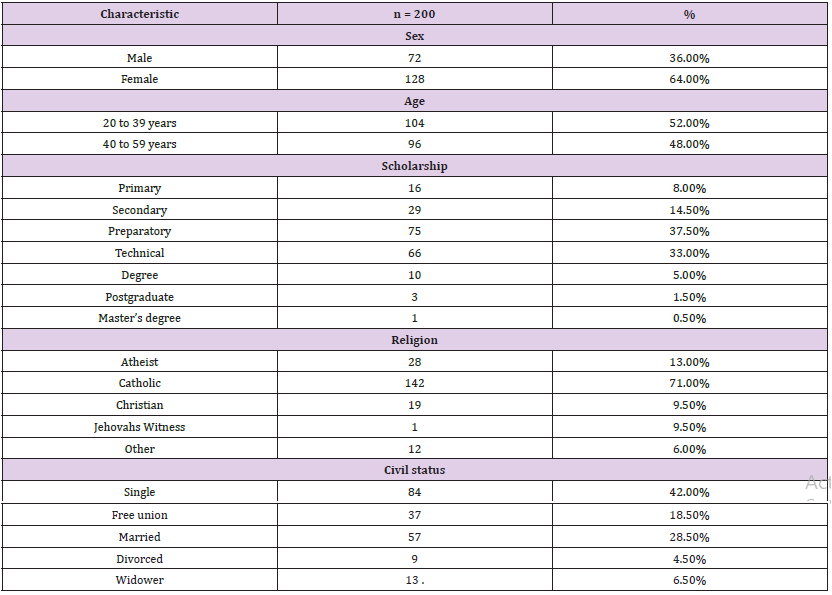
Table 2: Crombach’s Alpha value of each question of the questionnaire of determining factors in the acceptance of organ donation in beneficiaries of the Family Medicine Unit No. 20.
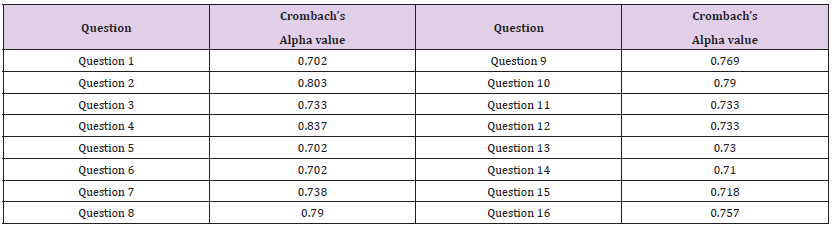
Table 3: Crombach’s Alpha values * of each question of the questionnaire of determining factors in the acceptance of organ donation in beneficiaries of the Family Medicine Unit No. 20.
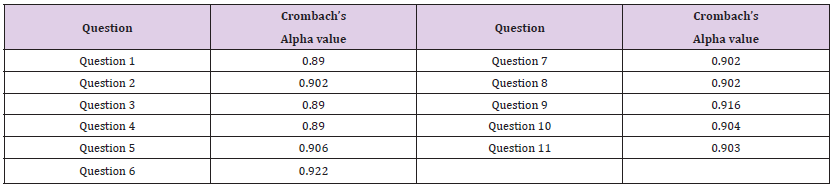
Table 4: Factor loadings of the instrument determining factor in the acceptance of organ donation in beneficiaries of the UMF No. 20 obtained in the exploratory factor analysis.
Note: Crombach’s Alpha if element is removed.
Table 5: Expected adjustment indices for a structural equation model and indices obtained for the confirmatory factor analysis of the questionnaire of determining factors in the acceptance of organ donation in beneficiaries of the Family Medicine Unit No 20.
A relevant aspect about the two dimensions (Social and Cultural) obtained after the confirmatory and exploratory analysis in this instrument are the items it presents, due to the fact that in a study carried out in Costa Rica, in health personnel on an item related to social sphere, I report that 26.3% of health personnel have the mistaken concept that brain death is a reversible condition [27]. Consistent with this result is another study carried out in Spain on health personnel that asks, among other items, Is a brain-dead patient dead? Could a person who died from cardiac arrest become a donor? states that 64.5% have a low level of knowledge regarding donation [28]. Therefore, in addition to updating continuous training on organ donation issues for health personnel, it is important to consider a consistent, clear, and relevant question that measures what it intends to measure. Our instrument has factor loadings above 0.90 in at least three items of both dimensions (social and cultural). Also showing good fit indices obtained through confirmatory analysis. There are instruments that have measured the Social, Cultural, Ethical, and Economic dimensions in reference to organ donation, however they have only managed to perform exploratory analysis [23], with a low KMO result and an explanation of the variance of 52.07. These values in our instrument improved by only considering the Social and Cultural dimensions in the median KMO and explanation of the variance of 58.29. There is another study [24] that did carry out confirmatory analysis by considering attitudes towards organ donation as dimensions (favorable, unfavorable, and distrustful attitudes) reporting factor loadings above 0.35 and with acceptable values in the adjustment indices such as RMSEA, CFI, NNFI. This opens a path to be able to carry out, between different social and cultural environments, the possible relationship of attitudes within the social or cultural field at various educational levels, places and ages of the population. Although there are few instruments with an exploratory and confirmatory level of analysis within organ donation, it is important to continue creating new instruments that, in the case of our study, provide new evidence to increase items within the Social and Cultural dimensions and in turn. perhaps allow greater openness to organ donation, which is increasingly necessary according to current health conditions.
The results of the instrument “Determining factors of organ donation in beneficiaries of the Family Medicine Unit (UMF) N0. 20, demonstrated good validity and reliability, which may allow its reproducibility in other Family Medicine Units of the different OOAD of the Country within the IMSS that have similar characteristics to the present study to identify the determining factors in the acceptance of organ donation.
To management personnel of the OOAD DF North, director of the UMF 20, to the medical personnel who contributed as a work team to make this article a reality for the benefit of IMSS beneficiaries.
To all the researchers of the original article for obtaining the data source that allowed this study to be successfully completed. All authors of this study approve the publication of this article.
The researchers of this article information declare that there is no economic interest or conflict of interest.
Study carried out in Family Medicine Unit No. 20 Calzada Vallejo 675, Col. Nueva Vallejo, CP 07750 , Gustavo A. Madero Delegation. Mexico City, of the Decentralized Organization of Administrative Functioning (O.O.A.D.) of the North Delegation of the Federal District (D.F. North) of the Mexican Institute of Social Security (I.M.S.S.).


