Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Tawfiq Nidal Turjman1* and Samir Rahmani2
Received: October 25, 2023; Published: November 14, 2023
*Corresponding author: Tawfiq Nidal Turjman, Medicine, Royal College of Surgeons in Ireland - Bahrain, Block 228, Road 2835, Al Sayh Muharraq Governorate, Bahrain
DOI: 10.26717/BJSTR.2023.53.008449
Background/Aims: This retrospective study was done on patients who underwent endoscopic sleeve
gastroplasty (ESG) to explain their weight loss, outcomes, adverse events, and safety. The results were
compared to available literature and current standards to understand how effective they were.
Methods: 331 patients (200 female, 131 male) had an ESG during the time period, August 2020 to
February 2022. Median BMI 33.8 kg/m2, median age 33 years old, median ESG time 37 min, and median
hospital stay was 16.8 hours. Using apollo overstitch, 5-6 sutures were inserted, starting at the prepylorus
to the greater curvature, and part of the fundus of the stomach. Patients followed a strict liquidbased
diet and follow-up appointments were made at 6 and 12 months to confirm and record progress
on a microsoft excel sheet.
Results: Median weight loss of 21.5% of total body weight in the first 6 months with a low revisional
ESG rate of 0.9% due to poor weight loss. Severe adverse events had an overall rate of 1.5% (5 patients
in total) due to pulmonary embolism (2 patients), internal bleeding (1 patient), external bleeding (1
patient), and perforation to fundus with helix (1 patient), while mild adverse events had an overall rate of
40% (133 patients), due to complaints of left shoulder pain (due to fundus sutures).
Conclusions: Results show that this new endoscopic method is safe, reversible, and less invasive with
satisfactory and maintained weight loss outcomes, making it a valuable option in weight loss management.
Keywords: Endoscopic Sleeve Gastroplasty; Obesity; Outcomes; Laparoscopic Sleeve Gastrectomy; Efficacy
Abbreviations: ESG: Endoscopic Sleeve Gastroplasty; LSG: Laparoscopic Sleeve Gastroplasty; TWL: Total Weight Loss; TBWL: Total Body Weight Loss; EWL: Excess Weight Loss
This retrospective study explains the results of 331 ESG cases, done at Novomed Surgical Hospital, and aids to provide an understanding of the overall efficacy, safety, and durability of the procedure, as well as a brief and refreshing review of the primary idea behind ESG. Pioneering in the field of medicine is of upmost importance as world health concerns such as obesity becomes an ever more, rising issue and thus, surgical interventions have proven to produce a reduction in mortality of the severely obese [1]. Traditional bariatric surgeries are being used to combat obesity, but with technological advancements, there are other alternatives that can be used, with careful selection, to solve this problem from a different angle. ESG is the new, minimally invasive method that works by limiting the gastric lumen through sutures stitching the greater curvature of the stomach and reforming the stomach into a tubular structure [2]. This is done by inserting full-thickness sutures along the interior lining of the stomach, using a double-channel endoscopic device, and inserting it transorally, while the patient is under general anesthesia (with endotracheal intubation) [2]. Considered among the less invasive procedures, ESG’s approach does not require any abdominal incisions being made, unlike the traditional laparoscopic sleeve gastrectomy (LSG) that requires incisional intervention, therefore, ESG’s safety profile is described as an improvement to LSG, while still yielding satisfactory weight loss outcomes [3]. This up and coming procedure has also proven to aid lowering risks of metabolic obesity-related conditions by lowering level of HbA1c, risk of liver steatosis and fibrosis, triglyceride level, and systolic blood pressure [3].
A retrospective study on 331 patients (200 female and 131 male), who have had ESG during the time period from August 2020 until February 2022, was done. Median BMI of 33.8 kg/m2, median age of 33 years old, median procedure time 37 min, and median hospital stay was 16.8 hours. The procedure was done by a single surgeon at a center of excellence after standardizing all pre- and post-operative pathways. Using apollo endosurgery overstitch, 6 sutures were inserted, starting at the pre-pylorus, greater curvature and the fundus of the stomach. Our modified technique was implemented on all cases by using an average of 10 stitch-insertion points per each suture (modified technique instead of the conventional 6 stitches in two lines), making sure full thickness of the stomach wall is taken in each and single overstitch to include the serosa. The intended suturing pattern used was 10 stitch-insertion points per each suture, 5 inwards and 5 backwards running along the stomach wall, to tighten the stomach and restructure its shape. This has achieved a narrow gastric tube all the way. This was done in supine position, under general anesthesia. Patients were instructed to follow a strict liquid-based diet and afterwards, follow up appointments were made at 6 and 12 months to confirm and record patient progress and weight loss on a microsoft excel sheet. For one week after the procedure, all patients were following a standardized liquid diet and were prescribed a low molecular weight heparin (clexane 40mg subcutaneously, once a day at 6pm). This study is a retrospective observational review of our internal results compared to the available international guidelines, without using any patient details or demographies. No ethical approval was needed as we have reviewed results and outcomes on our internal online system. Patient confidentiality was secured at all times by only using their (unit) MRN number. Verbal consent was obtained from our local research and development (R&D) department to access patient demographies and outcomes. This study was registered at our hospital as a review of service and considered for a clinical governance discussion. Other studies were used to compare between results from the articles and the results of the 331 patients. The gathered information was taken from studies that have met the inclusion criteria:
• Inclusion: English publication, completed research, peer-reviewed article, results explained in detail, publication date range 2015-2022. • Exclusion: Incomplete research, commentary, opinion piece, editorial.
It was recorded that the patients’ median total weight loss in the first 6 months was 21.5%. Long term follow up at 12 months was done on 138 patients (out of 331 total) which showed a maintained weight loss with an average of 19.2% of total body weight. With a revisional ESG incidence rate of only 0.9% (3 patients) due to poor weight loss, most of the patient outcomes were successful, but there were some cases that experienced adverse effects. During the first year of our practice, all patients were prescribed Clexane for one week post-operatively and we had no reported thromboembolic phenomena. This treatment was then stopped due to suspicion of no effect. As a result, two patients experienced a pulmonary embolism, which was treated successfully under the care of our hematologist. Hence, anticoagulant was added again to the post-operative care plan for the rest of the study duration. With the overall incidence rate of severe and mild adverse events being 1.5% and 40% respectively, the above data describes ESG as an acceptable method of weight loss which can be offered to patients after proper counselling and balancing risks and benefits. We had no cases that needed laparoscopic conversion, or any radiological procedures performed post operatively.
Total Body Weight Loss
By comparing the significance of our results to other studies made on a group undergoing ESG, a deeper understanding of the results of the 331 patients can be acquired in order to evaluate their success, especially while operating on the fundus and taking more frequent full thickness stitches. A recent 2018 observational study of 1000 patients, who have underwent ESG, describes their patient outcomes in the first 18 months after the intervention [4]. Patients’ results were shown as mean percentage of total body weight loss recorded in months 6, 12, and 18 (post-op) and there was significant weight loss over time [4]. It is noted that 92.4% of patients complained of abdominal pain or nausea post-op, but these symptoms were suppressed using medications given during the first week [4]. With only 24 patients readmitted for reasons such as severe abdominal pain, post-procedure bleeding, peri-gastric collection with pleural effusion, and post-procedure fever (with no sequelae), the rate of readmissions to the hospital due to adverse events was low [4]. Another retrospective study done in India, investigates and records the results of 53 indian patients after ESG [5] (Figure 1). Results show that 88% of patients have gone through >15% of total weight loss (TWL) at 12 months post-op and no patient experienced any serious adverse events [5]. Interestingly, female, and young patients (<30 years old) had better outcomes in terms of %TWL [5]. A multi-ethnic study done 35 ESG patients of the Asian population in Singapore has collected successful evidence in mean total body weight loss (TBWL) at 3 and 6 months (21 patients on the 3 month follow up and 10 patients on the 6 month follow up): 14.5±4.8% and 16.2±4.9%, respectively [6]. Their procedure was done with an average of 5 sutures and ESG mean time was 65±10 min, which is very similar to our method [6]. By studying the meta-analysis done on 15 different studies with 3994 patients (1815 of them have done ESG and 2179 of them have done LSG), we can accurately identify their dissimilarities through the follow up updates done on patients at 1, 6, and 12 months [7]. Pooled rates of total weight loss (%TWL) in ESG patients in 1, 6 and 12 months was measured to be 8.7 (95% CI 7.2-10.2), 15.3 (95% CI 14.1-16.6), and 17.1 (95% CI 15.1-19.1), respectively, while the pooled rate of %TWL in LSG was proven to be superior (P = 0.001) with a higher rate of 30.5 (95% CI 27.4-33.5) at 12 months post-operation [7]. The pooled rates of BMI and excess weight loss (%EWL) of the ESG results at 1, 6, and 12 months were considered “comparable” to those from the LSG results [7]. All the above studies have shown consistently, a trend of outcomes that match the outcomes of our own study. ESG produces satisfactory results as an innovative and minimally invasive treatment for obese patients.
Adverse Events
Weight loss procedures can cause adverse events, thus looking at different types of weight loss interventions and taking into account the rate of adverse events will give us a broader understanding of how our ESG study compares to other studies on ESG and other types of procedures. Using the same meta-analysis on the 15 different studies and utilizing it to assess the results of the two procedures, ESG and LSG, will help highlight the differences in their safety profiles [7]. This wide-range study demonstrates the records of pooled rates of adverse events in both procedures [7]. The statistical evidence shows a certain advantage in risk control in endoscopic sleeve gastroplasty in this study, as it is the less invasive method, thus making it the relatively safer option, because it takes less time, has less adverse events, and is reversible [7]. Both the pooled rate of adverse events in ESG being 2.9% (95% CI 1.8-4.4) and our own study’s pooled rate of severe adverse events being 1.5%, show an identical advantage over the pooled rate of adverse events in LSG in terms of safety [7]. An alternative proof of the superior safety in ESG is seen in a comparative study made on patients who have either undergone endoscopic sleeve gastroplasty or intragastric balloon insertion (fluid filled IGBs were used for implantation) in a time range of December 2015 until October 2017 [8]. After comparing the results of the two treatments, it was found that the group of patients, who have been treated with intragastric balloon insertion, experienced a higher incidence of adverse events of 17% (P=0.048), while the other group of patients, who had been treated with ESG, had only 5.2% (P = 0.048) [8]. Additionally, the ESG group had better weight loss outcomes, compared to the patient group who were treated with intragastric balloon insertion [8]. Another meta-analysis done on ESG operations (1542 patients) from 9 studies, has concluded that the overall estimate of severe adverse events was 1% (P = 0.08) and the pooled rate of mild adverse events was 72% (P < 0.01), giving further insight on the general safety of ESG [9] (Tables 1 & 2).
Table 1: Adverse events of 331 patients that have done ESG in a single surgical hospital, displayed in table form.
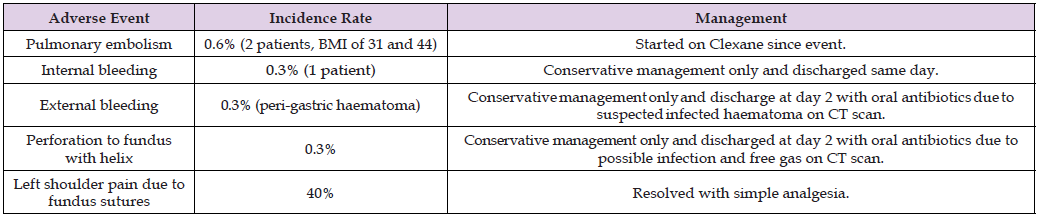
Note: Table abbreviations: Endoscopic sleeve gastroplasty (ESG), body mass index (BMI).
Revisional Procedures
Other than analyzing the outcomes of ESG procedures and comparing their rate of adverse events to other procedures of the same or different nature, there are some cases that are more complex, because they fail to produce a satisfactory outcome after their primary weight loss intervention. Thus, they require a revisional operation after the first one (after taking a psychological educational course to ensure the weight regain is not due to their incompliance with the required diet and so they require revisional ESG), because of weight regain, loss of satiety, or due to poor weight loss [10]. A retrospective analysis, conducted on 120 ESG procedures done between March 2017 and May 2019, has reported 4 cases that underwent a redo endoscopic sleeve gastroplasty due to multiple reasons: weight regain, insufficient weight loss and a progressive loss of satiety [10]. After retaking ESG, there were no adverse events that took place, and three of the four patients were available for their 6 month follow up to show results: the mean %EWL (excess weight loss) and mean %TBWL (total body weight loss) were 44.2% and 20.4%, respectively, proving the revisional ESG procedure successful [10]. Another option is discussed in an article made on 1665 patients that have done primary ESG, but unfortunately, just like any other interventions, some require revisional procedures due to adverse events, lack of weight loss/weight gain, or discomfort [11].
Hence, 20 patients have gone through revisional laparoscopic sleeve gastrectomy and have attained the appropriate positive results with %TWL at 6 and 12 months being 21±2.7 (n=11), and 25.6±4.1 (n=8), respectively [11]. Consequently, there were no adverse events that took place afterwards.11 This provides evidence that an LSG can work as a revisional operation for patients who have not been successful post-ESG [11]. A revisional ESG after a sleeve gastrectomy is another case which is investigated in a study that analyzes 34 patients who had primary sleeve gastrectomy and were required to do a revisional ESG (due to weight regain) to yield the intended satisfactory results [12]. Mean (SD) %EWL at 6 months and 1 year were 51.9% (19.1) and 69.9% (29.9), while the mean (SD) %TWL at 6 months and 1 year were 13.2% (3.9) and 18.3% (5.5), respectively [12]. No severe adverse events occurred with the 34 patients [12]. This represents how efficient of a revisional ESG after a failed sleeve gastrectomy is and how successful the outcomes are [12]. When taking into consideration our rate of revisional ESG of 0.9% and that no adverse events took place after those revisional operations, this shows the general low chance of the primary ESG being unsuccessful and of the revisional operation yielding adverse outcomes.
This minimally invasive weight loss intervention, used to treat obese patients, is safe and durable with satisfactory and well-maintained weight loss compared to the available literatures. When compared to results from other studies, our incidence rates of mild/severe adverse events and revisional ESG agree with the standard of satisfactory outcomes of a successful weight loss intervention. ESG provides an alternative endoscopic approach that is reversible and leaves no abdominal scars, while also having a decreased operative time, a better safety profile, and still giving acceptable weight loss outcomes over a long period of time. We appreciate further studies are needed on a larger cohort of patients with long follow ups at 2 and 5 years.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.


