Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Gitali Bhagawati*1 and Sania Paul2
Received: October 20, 2023; Published: November 01, 2023
*Corresponding author: Gitali Bhagawati Senior Consultant and Clinical Lead, Microbiology, and Infection Control, Dharamshila Narayana Superspeciality Hospital, Narayana Health, Delhi, India
DOI: 10.26717/BJSTR.2023.53.008421
Abbreviations: MDR: Multidrug-Resistant; FUS: Fungal Urosepsis; LIS: Laboratory Information System; MRD: Medical Records Department; NAAT: Nucleic Acid Amplification Test; SDA: Sabouraud’s Dextrose Agar; CLED: Cystine Lactose Electrolyte Deficient; WBC: White Blood Cells; ATCC: American Type Culture Collection; SPSS: Software Statistical Package for the Social Sciences; AFSP: Antifungal Susceptibility Pattern
India’s healthcare system was overburdened during the second wave of coronavirus disease 2019 (Covid-19) pandemic in India [1]. Fungal co-infections and super-infections were overloaded in this category of patients, leading to higher morbidity and mortality [2,3]. Superinfection by Multidrug-resistant (MDR) Candida, especially Candida auris made the situation worse with treatment failure and adverse clinical outcomes [4]. The aim and objective of this study is to evaluate the cases of fungal urosepsis (FUS) by Candida auris among admitted cases of Covid-19 infected patients.
Study Design
The retrospective study was carried out in India in the department of microbiology in a 200 bedded tertiary care hospital in Delhi, over a period of two months. Patients’ data were collected from Laboratory Information System (LIS), requisition forms, WHONET 5.6 software and files from the department of Medical Records Department (MRD) for a duration of 2 months- April, and May 2021 at the peak period of the pandemic. Approval was taken with no. DNSH/HR/ PER/D-110103.
Microbiological Testing
A. Covid-19 True Nat Real Time Polymerase Chain Reaction (RT-PCR)
Patients admitted with acute respiratory illness (ARI) were tested for Covid-19 by Truenat real time PCR method.) using nasopharyngeal swabs. Confirmatory gene used was RdRP gene or ORF1a gene. (Molbio diagnostics Pvt., Ltd., Goa, India). A person with a positive Reverse transcription polymerase chain reaction (RT-PCR) as Nucleic Acid Amplification Test (NAAT) were considered as confirmed Covid-19 infection (CC19I)
B. Blood Culture
Paired blood culture bottles were processed by automated blood culture machine (BACTEC FX40, Becton Dickinson, Heidelberg, Germany). Based on Gram stain finding for budding yeast cells, sub-culture was done on Sabouraud’s Dextrose Agar (SDA); SDA tubes were incubated at both 370C and 250C for 24-72 hours.
C. Urine Culture
Non-duplicate urine samples with wet mount showing ≥ 10 White blood cells (WBC)/cubic mm [5] were inoculated on Cystine Lactose Electrolyte Deficient (CLED) agar. Significant growth with colony count ≥ 100,000 Colony Forming Unit (CFU)/ml in clean catch midstream urine were considered for Yeast and Yeast like fungus (YYLF). Pure growth of suspected non-lactose fermenting colonies was inoculated on two SDA slants, one was incubated at room temperature whereas, other was kept at 37°C for 24 - 72 hrs [6].
D. Final Identification of YYLF Identification
The growth on the slope was processed for identification by colony morphology, Gram stain and/ Lactophenol cotton blue (LPCB). To differentiate between Candida albicans and Non-albicans Candida (NAC), germ tube test was done. Final identification and antifungal susceptibility testing were done by Vitek 2 Compact system. (bioMérieux, Inc. Durham, North Carolina/USA). Control strains for Candida auris included Candida parapsilosis American Type Culture Collection (ATCC) 22019 and Candida krusei ATCC 14243.Statistical analysis was done by Chi-square test using Software Statistical Package for the Social Sciences (SPSS) version 22.0. The outcome was determined to be statistically significant difference if p-value was found to be <0.05.
Total patients admitted with CC19I during the peak period of Covid-19 pandemic were 487.Out of total 487 admitted patients with CC19I, C. auris related fungemia was found in 5 (1.03%) patients while C. auris related urinary tract infection (UTI) was detected in 12 (2.46%) patients. [p value 0.7730]. Out of 12 patients with C. auris related of UTI, 5 patients had line related UTI prior to blood stream infection (BSI); they were together labelled as fungal urosepsis (FUS).
Antifungal Susceptibility Pattern (AFSP) Among C. auris Related FUS [7]
C. auris isolates were 100% resistant to fluconazole (Minimum inhibitory concentration, MIC >=32 mg/L); however, 100% sensitive to caspofungin (MIC 0.25) and micafungin (MIC <0.06) (Table 1).
Demographic Profile of Patients C. auris Related FUS
All the 5 cases of FUS were of elderly age group >=60 years with male to female ratio -4:1. All the patients had history of prolonged intensive care unit (ICU) stay (>10 days) with comorbid condition like DM (60%) and hypertension (HTN) (40%). All of them (100%) were catheterized and were on central lines. Out of the 5 patients, 3(60%) were on mechanical ventilator. All the FUS patients were on prolonged broad-spectrum antibiotics, steroids and immunomodulators. The mortality rate was 60% (3/5) among these patients (Table 1).
Table 1: Demographic profile, Laboratory parameters and Antifungal Susceptibility Pattern in Patients with Confirmed COVID-19 Infection with MDR Candida auris related Fungal Urosepsis.
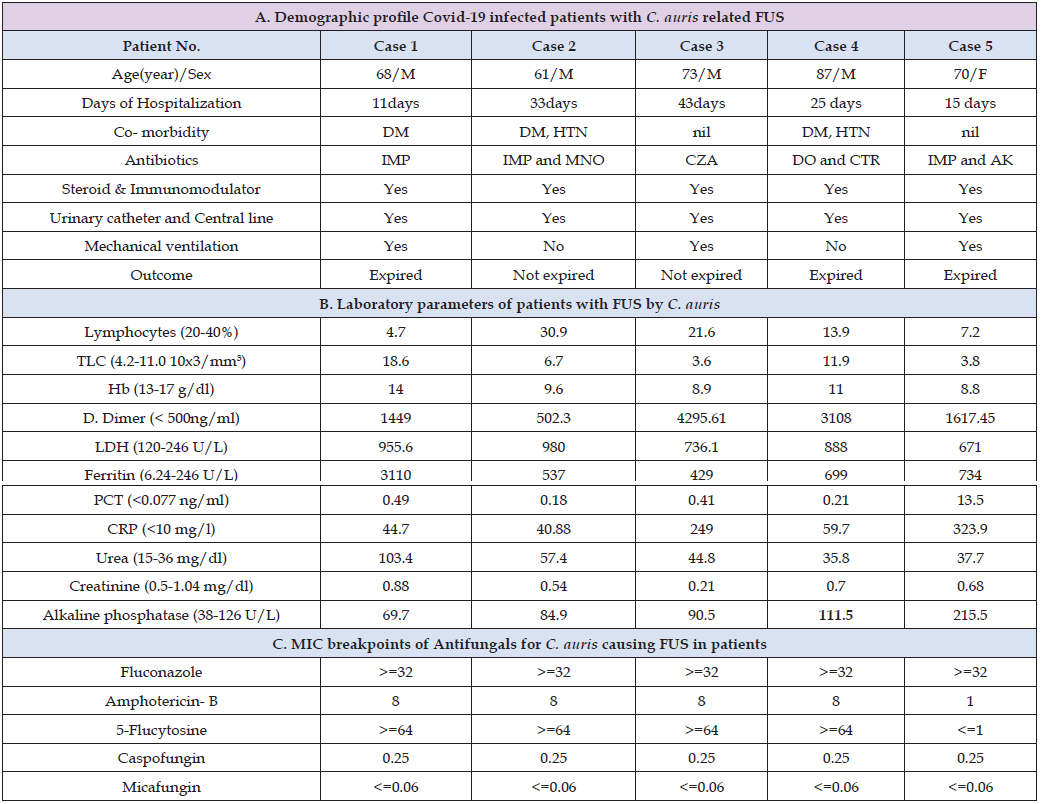
Note: FUS: Fungal Urosepsis; MIC: Minimum Inhibitory Concentration; DM: Diabetes Mellitus; HTN: Hypertension; IMP: Imipenem; MNO: Minocycline; CZA: Ceftazidime-Avibactum; DO- Doxycycline; CTR: Ceftriaxone; AK: Amikacin; TG: Tigecycline; TLC: Total Leucocyte Count; LDH-Lactate Dehydrogenase; CRP- C-Reactive Protein
During the peak period of 2nd wave of COVID-19 pandemic in India, patients with CC19I who were admitted with severity had succumbed to secondary infections. The aim was to evaluate the cases of fungal urosepsis (FUS) by Candida auris among the patients. Among 487 admitted cases with CC19I, we found 5 (1.03%) cases of MDR C. auris related FUS. Studies are extremely rare in relation to FUS in Covid-19 infected patients. However, literature on C. auris related fungemia and candiduria are available to some extent. In our study, fungemia by C. auris was found in 1.03% (5/487) patients of Covid-19 infection which was in concordance with another finding, 1.67% (10/596) [8] but in contrast to other literature, 0.63% (2/314) [9]. Cases of UTI in post-Covid stage by Candida tropicalis, Candida glabrata and C. auris were mentioned in one article [10]; candiduria by T.asahii [11] and C. auris [12] are available in literature. Covid-19 opened a pandora’s box for all opportunistic infections because of altered immune mechanism leading to decreased phagocytic function, steroid related neutrophil dysfunction etc. [10]. Simultaneous high-risk factors like mechanical ventilation, central lines, indwelling catheters, steroids, monoclonal antibodies, broad-spectrum antibiotics etc. play a major role in invasive fungal infections (IFI) [13,14]. MDR Candida auris is a global threat due to its limited susceptibility to antifungals such as echinocandins [9,15]. Table 1 explains the MDR status with high MIC of C. auris. During 2nd wave of pandemic in India, many HCWs were also down with Covid-19 infections for which they were kept on isolation and the contacts were on quarantine leading to limited working staff in patient care areas. With overloaded burden of work, there was probability of breach in infection control practices (ICP) leading to transmission of MDR C. auris. Moreover, screening for C. auris colonization has also been limited in healthcare facilities [16]. C. auris-urosepsis related mortality rate was found to be 60% (3/5) (Table 1) like other literature, (53.33%) [8]. Prolonged hospital stays, high “Candida score” and septic shock were associated with increased mortality within 30 days of positive culture for C. auris [17].
Literature has limited evidence on FUS in Covid-19 infected patients. C. auris related FUS was really a matter of concern among the immunocompromised patients with high risk factors and comorbid condition. Stringent ICP along with diagnostic stewardship, antibiotic stewardship is the basis of prevention of C. auris related secondary infections. This study can help in near future for the preparedness of any kind of viral infections which can have a sequential effect of secondary infections by the deadly MDR pathogens like C. auris. Healthcare of any country should be prepared for any kind of pandemic beforehand with the availability of resources and pooling of manpower in health-care institutes providing mandatory and continuous ICP training for the same.
Our acknowledgement goes to the team of management of Dharamshila Narayana Superspeciality Hospital, Delhi for their immense support to carry out this study.


