Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Parveen Kumar1, Arindam Chatterjee2, Gurpreet Singh3, Vivek Jain4, Ashutosh Pareek5, Ram Khandelwal6, Deepak Sharma7 and Madan Mohan Gupta8*
Received: October 16, 2023; Published: October 27, 2023
*Corresponding author: Madan Mohan Gupta, School of Pharmacy, Faculty of Medical Sciences, The University of the West Indies, St. Augustine, Trinidad &Tobago, WI
DOI: 10.26717/BJSTR.2023.53.008413
In the present scenario, combination drug therapy for enhancing anticancer effect becomes a standard approach due to its various benefits that include targeting of multiple critical molecular processes, low dose delivery resulting in lower toxicity, lesser chances of drug resistance, lesser side effects, and enhanced patient tolerance. Combination therapy is used to treat distinct types of cancer because of its characteristic of potential targeting. The other benefits are targeted via different signaling pathways to the tumors, but the actual results shown cannot exactly predict its utility with prior studies as the anatomic and evolutionary properties of solid tumors are quite different from liquid tumors like leukemia. One of the challenges faced when choosing the combination regimen is the multiple drugs used that results in difficulty to coordinate the pharmacokinetics of these drugs. In some cases, the healthy tissues may be harmed as each drug works by targeting different pathways. As such, drug resistance requirement of simultaneous target inhibition and accurate drug ratio are required to obtain effective results.
Keywords: Acute Lymphatic Leukemia; Combination Drug Therapy; Pharmacokinetics; Drug Ratio; Drug Resistance
Abbreviations: DNA: Deoxyribonucleic Acid; POMP regimen: Methotrexate, 6-Mercaptopurine, Vincristine and Prednisone; MTD: Maximum-Tolerated Dose; PTX: Paclitaxel; CL-1- Lung Cancer Cell Line; DMN: Dimethyl Nitrosamine; CSCs: Cancer Stem-Like Cells; TLR agonists: Toll-Like Receptor; STING Agonists: Stimulator of Interferon Response cGAMP Interactor 1; MAPK: Mitogen-Activated Protein Kinases; PI3K: Phosphatidylinositol 3-Kinase; Akt: Protein Kinase B; mTOR: Mammalian Target of Rapamycin; HCT: Human Colon Cancer Cells; CRC: Colorectal Cancer; 5-FU: Fluorouracil; HCC: Hepatocellular Carcinoma; EMT: Epithelial–Mesenchymal Transition
In the treatment of cancer, combination therapies which involve the combination of two or more therapeutic agents or therapeutic targets are widely used nowadays. Combination therapy aims to enhance the probability and magnitude of therapeutic responses in individuals, lowering the needed resistance. Combination therapy using anticancer drugs is highly promoted compared to single drug therapy because combination therapy targets key pathways in order to synergize and magnify the effect of drugs [1,2]. Apoptosis, a biochemical pattern consisting of the suicidal nature of cancer and normal cells, is gaining attention as this mechanism clears all cancer cells. Drugs that work by apoptosis, enhance apoptosis or antagonize antiapoptotic factors like survivin and retinoids that cause cytodifferentiation activity become the choice in combination therapy [3-5]. Similar to every other therapy, even with the various benefits, there are some limitations in using combination therapy, hence it has to be used accordingly. Intrinsic difficulties in the pharmacology of cancer suggest that before using any combination of drugs, the pharmacological profiles of these drugs must be studied in detail, from their kinetics to their interaction. This approach in itself is a highly challenging one [6,7]. Currently, combination drug therapy for enhancing anticancer effect becomes a standard approach because of its various benefits that include targeting of multiple critical molecular processes, low dose delivery resulting in lower toxicity, lesser chances of drug resistance, lesser side effects, and enhanced patient tolerance.
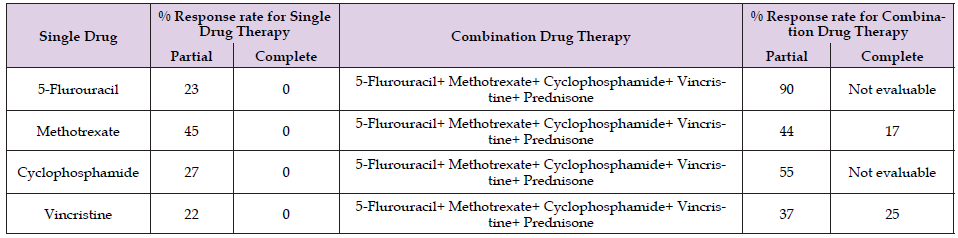
In cancer therapies, synergistic effects of drugs are observed when using combination therapy. Some combinations that show considerable results gain attraction for treating distinct types of cancers. A number of preclinical researchers have identified the combinations of anticancer drugs that are potent [7-11]. Therefore, with the various benefits, combination therapy becomes the routine strategy for treating various types of cancer as it demonstrates lower rates of treatment failure and drug resistance development. One example is the use of Celastrol in combination with chemotherapeutic agents, in which synergistic anticancer effects suppress the growth of cancer such as melanoma, hepatocellular carcinoma, breast cancer and lung cancer [12-15]. The advantages of using combination regimen for cancer treatment is presented in Figure 1. Combination therapy is the choice for treating distinct types of cancer because of its characteristics of potential targeting. The other benefits are targeted via different pathways to the tumors, but the actual results shown cannot exactly predict its utility with prior studies as the anatomic and evolutionary properties of solid tumors are quite different from liquid tumors like leukemia [16-19]. In studying cancer treatment among patients with high risk of developing metaphases, combination therapies show better results in killing the fraction of tumor cells. According to the studies of Greenspan and Cooper, combination therapy using alkylating agents, methotrexate, 5-fluorouracil and vinca alkaloids in treating breast cancer showed better results with 80-90% regression compared to single therapy with 20-30% regression. Table 1 shows the % response rate obtained from using single drug therapy and combination therapy for advanced breast cancer [20].
Table 1: Reported response of patients treated for advanced breast cancer by using single and combination therapy.
Combination therapy was first explained in 1965, where James F. Holland and Emil J. Freireich stated the possibility of using combination therapy to treat pediatric patients having acute lymphocytic leukemia. The drugs used were methotrexate, 6-mercaptopurine, vincristine, and prednisone. This combination was called the POMP regimen/therapy. The POMP regimen showed positive effects in pediatric patients and was found successful in reducing tumor burden and enhancing time period for remission. With the successful results obtained from POMP regimen, combination drug therapy became an option in treating cancer. Further studies were then done to identify more combinations that target distinct pathways to develop synergistic or additive effects [21]. However, some limitations of combination therapy are observed from various reported papers. It is found that the approved combination therapy can be explained by a simpler and older null hypothesis relating the independent action of the drug and the number of anticancer drugs targeting the specific genes. In other words, combination therapy may have biological rational depending on the drug action, interaction and molecular understanding [22,23]. A majority of combination therapy shows additive or synergistic effects that achieve responses superior to that expected from their single drug action. One example is the case of blood cancer, where mono therapies do not show significant results but the use of multi agents increases curable rate up to 80% [24].
Therefore, combination therapy is the long-term goal of translational cancer research and requires further research to identify more combinations with additive or synergistic effects in treating cancer. Data obtained on combination therapy with the help of computational modelling also suggests that the additive or synergistic and independent action can jointly bring more benefits to patients [25].
Benefits of Combination Therapies [26-28]
1. Improves efficacy by providing synergistic drug ratio to the
cancer cells/tissues for a prolonged period without harming
the healthy cells/tissues.
2. Lowers chances of developing drug resistance.
3. Identification and evaluation of synergistic combinations as
early as possible in the development process using technology
platforms like Combi Plex provide a way to increase efficacy,
improve safety, and decrease the time and patient resources
needed for developing effective combination therapies.
4. Enhances tolerance in patients.
5. Lowers the doses of a single drug as multiple drugs are provided,
hence reducing side effects produced from single drug.
6. Works on different pathways to target the tumor cells/tissues,
enhancing cure rate.
The pathway used for combination drug therapy including preclinical and clinical development is given in (Figure 2).
Challenges Related to Development of Combination Regimen for Cancer Treatment
A combination of two or more anticancer drugs forms the combination regimen used for disrupting multiple mechanisms related to the growth of cancer cells/tissues or tumor. There are a number of challenges in combination therapy including scientific, economic, legal, and regulatory barriers. Combination therapy enhances the treatment, gives good results, lowers toxicity to healthy cells, and coordinates drug pharmacokinetics and exposure to tumor by minimizing the development of multiple drug resistance [29-30]. The challenges faced while choosing combination regimen are:
1. Multiple drugs are chosen so it is difficult to coordinate pharmacokinetics
of these drugs.
2. Healthy tissues may be harmed as each drug works by targeting
different pathways.
3. Requirement of simultaneous target inhibition to get effective
results.
4. Requirement of accurate drug ratio to get effective results.
Facts that Need to be Focused
When developing a combination drug regimen, the facts that must be focused are:
Drug Ratio Dependency: Combinations of drugs may act synergistically, additively, or antagonistically, depending on the molar ratios of the individual drug making up the combination regimen. Additive drug ratio gives activity that is equivalent to the total effects of each contributed drug in the combination. Synergistic ratio results in activity that is higher compared to the added effects of each drug. Antagonistic ratio results in activity that suppresses the effects of other drugs and sometimes the individual drug. For example, in vitro studies conducted find strong antagonistic effects when irinotecan and cisplatin are used in 1:1 ratio, but the same drug combination used in 4:1 ratio shows synergistic effects. On the other hand, the combination of irinotecan and floxuridine exhibits synergistic effects when used at 1:1 ratio but shows strong antagonistic effects when used in 10:1 ratio. Considering the importance of drug ratio dependency, there are still challenges finding suitable ratios to be used in vitro and in vivo. Ratios showing synergistic effects in vitro may not exhibit the same effects in vivo. For instance, the 4:1 ratio of doxorubicin and vincristine liposomal formulation produces synergistic effects during in vitro studies but when the combination is encapsulated, vincristine leaks out from the liposome, resulting in an antagonistic effect due to the drug ratio of 20:1 that is less effective than the free drug [31-33].
Pharmacokinetic Profiles: As per the drug ratios concern, the constant change of dosing becomes difficult to maintain, however any particular drug ratio that enhances antitumor activity. To compensate for such problems, pharmacokinetic differences in combination regimen are exposed to the patient with high dosage of each agent to achieve simultaneous and prolonged inhibition of each target. However, these strategies expose more healthy cells/tissues to the drug, causing unnecessary toxicity that affects the utility of the combination therapy. As such, choosing the pharmacokinetic profile of the drug is crucial when preparing combination regimen [34].
The combination therapy, reduction in resistance towards the drug is observed, along with a number of anticancer therapeutic advantages like reduction in tumor growth, metastatic potential, and arrest of mitotically active cells, reduction of cancer stem-like cell (CSC) population and induction of apoptosis. The most noticeable benefits of using combination drug therapy are prevention of drug resistance, reduction of drug toxicity, and improvement of drug efficacy. Day by day, drugs are becoming more personalized and greater focus is being put into the development of therapies used to target the specific mutations that cause cancer. However, a number of these drugs show short term effects and tumors become resistant towards these drugs within a few months. Larger tumors are genetically diverse, where only a portion or small populations of tumor cells are resistant towards a particular drug effect. When the drug is provided to the patient during treatment, the resistant cells that are not affected by the drug survive, after which they multiply like any cancer cell, causing failure of the treatment. As such, the use of single drug therapy is highly avoided in cancer treatment and tumor removal. In this case, a combination of two or more drugs is preferred due to the high success rate in treating cancers like leukemia, colon cancer, breast cancer, hepatocellular cancer, etc. A number of researchers have also represented mathematical modelling design to predict the effects of combination targeted therapies on cancer cells. Bozic designed mathematical model using data from 20 melanoma skin cancer patients.
His results suggest that if 6.6 billion base pairs of deoxyribonucleic acid (DNA) present in a human diploid cell have undergone mutation and become resistant to each of the two drugs, such drugs will not benefit the sustained improvement in a number of patients. His modelling design proves that the choice of drugs is an important factor in combination therapy; hence it is important to always use drugs with distinct target pathways. These modelling designs confirm the benefits of using combination therapy compared to single drug therapy, as using two drugs simultaneously is observed to be more effective than using one drug after another. Bozic also concludes that there is very less or no chances of a cure in single drug therapy even if there is no cross-mutation present, but in combination therapy, there are hope for a cure even with the presence of cross-resistance mutations. His study provided a number of valuable results for developing drugs and designing clinical trials and practice in combination therapy for treating various types of cancer [18].
The combination therapy and its advantages have been published with promising results, as shown in the given below Table 2 and complete information in the below segment.
Pancreatic Ductal Adenocarcinoma
Pancreatic cancer is considered lethal and untreatable most of the times. Even with the advancements in research and therapy for treating pancreatic cancer for the past 15 years, the treatment of pancreatic cancer is still challenging due to its aggressive nature and the problems that occur while developing selective and effective therapeutics. Quinn et al., in his research, studied that the sabutoclax, a pan-Bcl-2 inhibitor, and minocycline, an antibiotic that has previously shown anticancer effects, in combination, acted synergistically on the intrinsic apoptotic pathway. This combination shows selective toxicity and lowers the growth of tumor when tested in vitro and in vivo on the ductal adenocarcinoma. While this combination produces a synergistic effect and yields potent results, pancreatic cancer still remains as a devastating disease with poor prognosis due to the lack of early diagnostic markers, delayed detection, diverse genetics, and rapid metastasis [35,36].
Leukemia in Children
Acute lymphatic leukemia in children is a good example of combination drug therapy yielding positive results in 1965.The rate of improvement increases from 22% with the use of methotrexate alone to nearly 100% when used as a combination of two or more drugs. The National Cancer Institute (NCI) reports that the median survival rate of acute leukemia in children improved from six months in 1956 when single agent is used (i.e., prednisone, methotrexate, and 6-mercaptopurine) to 36 months in 1965 following the development of around eight drugs and their use in distinct combinations. Unfortunately, there are no agents that can permanently revert all the leukemic bone marrow back to normal. By using combination therapy that targets different pathways, synergistic effects and potent results against particular cells can be obtained. A number of researchers that studied combination therapy for treating leukemia in children found drug independence and interaction as major points that should be evaluated when developing combinations [21].
Lung Cancer
Being one of the most prevalent diseases that is cured very slowly, lung cancer contributes to a large number of deaths worldwide. According to researches, combination therapy using low toxicity compounds and paclitaxel (PTX) shows good impact in treating lung cancer and helps to minimize the toxicity caused by PTX. Other benefits include the exhibition of synergistic action, prevention of drug resistance and minimum toxicity. Assay results suggest that PTX shows strong antiproliferative effects on CL1–5 cells when used in combination with other drugs like 5-dimethylnitrosamine(5-DMN), in comparison to when being used as a single agent. The anticancer action of PTX in combination therapy shows synergistic effects and higher proportion of cell cycle arrest that enhances ROS levels compared to using PTX alone. As such, the combination of PTX and 5-DMN is considered a potential agent to treat lung cancer that shows better effects and minimizes toxicity of PTX compared to PTX as a single agent [37- 39].
Breast Cancer
Unlike melanoma, lung cancer, and leukemia that have the highest somatic mutational load, breast cancer is not considered highly immunogenic cancer. Combination therapy exhibits potent results in treating breast cancer using combination of agents that target CSCs, cancer biology and chemotherapeutic. While PTX shows minimal effects on the proliferation and growth of breast cancer CSCs when used in monotherapy, good results in killing tumor cells can be obtained when using PTX in combination with salinomycin. As different subtypes of breast cancer react differently, designing combination therapies is crucial in the treatment of breast cancer. Targeted combination therapy enhances response by boosting immunogenicity and overcoming mechanisms of immune escape [40-43]. Combination therapy of treating breast cancer is presented as a flow chart in (Figure 3), while the combination regimen that shows positive effects by inhibiting the production of cancer progenitor cells is given in (Figure 4).
Colorectal Cancer
Combination therapy used in colon/colorectal cancer (CRC) shows more promising and effective results with durability compared to monotherapy in which resistance occurs rapidly most of the times. In clinical trials of combination therapies, different pathways like PI3K/Akt/mTOR and MAPK that are crucial for intracellular signaling cascades in cancer cells, are used to target cancer cells. In CRC cellHCT116, SN38 induces the activation of Akt and MEK, along with a rise in their phosphorylation by 2 folds in Akt and 7 folds in MEK. Akt and MEK activation are used by CRC cells to enhance their survival upon treatment. The synergistic action obtained in CRC cells by relating irinotecan with agents that block the Akt and MEK thus permits a significant decrease in drug doses. Analysis of phosphokinase changes induced by chemotherapy maybe helpful in eliminating the escape mechanism, moving towards potential targets for combination therapies with synergistic action, and evaluating doses and schedules of combination regimens containing targeted agents [44-46].
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is one of the cancers in which cases increase every day when observed over several years. Early diagnosis of HCC is mandatory to obtain the best treatment output. Combination therapy uses the combination of5-FU and salicylic acid to treat HCC. From a number of recent studies on CSCs, it is observed that if 5-FU is given as a monotherapy to treat this type of cancer, the results are not successful and there is chance of tumor relapse. However, when used in combination with salicylic acid, not only does it show synergistic effects, it also enhances the sensitivity of HCC cells to 5-FU and eradicates HCC cells. This is because salicylic acid potentiates the antitumor effects of 5-FU by down-regulating CSCs in HCC cells. Strategies to enhance epithelial–mesenchymal transition (EMT) by inhibiting the translocation of active β-catenin to the nucleus can show effective results in the down regulation of CSCs [47,48]. The combination drug therapy used to treat different types of cancers is presented in Table 3.
In 2020, Denis L. Jardim and group conducted a trial for comparing the efficacy and safety of anticancer agents (combination versus single cytotoxic) for the treatment of advanced/metastatic cancer by designing a randomized trial that includes 95 randomized comparatives for single versus combination therapies at59.4% and 41.6% for Phase II and Phase III trials respectively. There were about 28,704 patients enrolled in the trial and the combination of drug used for backbone treatment was erlotinib (20%), followed by letrozole (9%), and bevacizumab (7%). Erlotinib-20%, the most frequently used drug present in 5% of combination therapies, enhances the rate when used in combinations compared to in single doses. Compared to single dose therapies, combinations of non-cytotoxic agents enhance their efficacy, increase toxicity and treatment mortality of cells, and decrease patient death rates [49]. NCI reported Phase I/II trial studies for testing the combination of new anticancer drug Nedisertib with Avelumab, radiation therapy for advanced/metastatic solid tumors that have spread to other places in the body, and hepatobiliary malignancies. When used in combination, these drugs synergize into other effects, Nedisertib stops the growth of tumor cells by blocking the enzymes needed for cell growth, while. Avelumab, an immunotherapy with monoclonal antibodies helps the immune system to attack the cancer cells, interfering with the capability of tumor cells to grow and spread. This combination helps to treat patients with solid tumors and hepatobiliary malignancies by focusing on the combination of standard chemotherapy with hormonal, targeted, and immunotherapy medicines. Thirty patients were involved in these randomized clinical studies where the dose used was the MTD and recommended Phase II dose of Nedisertib (M3814) in combination with hypo fractionated radiation and avelumab (Phase I) [49-61].
From numerous studies, it can be concluded that combination therapy shows very effective results associated with anticancer effects. This is due to its ability to target multiple pathways, thus minimizing drug resistance as cancer cells become incapable of adapting to the toxic effects from two different therapeutic agents. Due to its mechanism of targeting distinct pathways, combination therapy increases the chance of curability and controlling the disease and lowers the chances of cancer cells becoming increasingly malignant. Also, in a number of cases, lesser dose is required compared to using the drugs individually as multiple agents are used to reduce toxicity and resistance. An additional advantage of combination therapy is that the multiple drugs in the combination regimen are capable of targeting the heterogeneous nature of tumors, enhancing the chances of killing all cancer cells including the CSC population which is mainly responsible for drug resistance and cancer recurrence after remission in later years. Combination therapies also enhance the efficacy and efficiency of treatment. Despite all advantages, there are still limitations in combination therapies, such as drug interaction which should be considered thoroughly.


