Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Burak İncebeyaz1, Elif Polat Balkan1*, Hatice Ahsen Deniz1, Abulfaz Isayev2 and Kıvanç Kamburoğlu1
Received: September 26, 2023; Published: October 06, 2023
*Corresponding author: Elif Polat Balkan (DDS), Department of Dentomaxillofacial Radiology, Ankara University, Faculty of Dentistry, Besevler, Ankara 06500, Turkey
DOI: 10.26717/BJSTR.2023.53.008363
Background: Which imaging systems should be used during student education is a matter of debate. We compared complementary metal oxide semiconductor (CMOS) and photostimulable phosphor plate (PSP) image receptors for time efficiency and incidence of artifacts using phantom jaws.
Materials and Method: The current study compared CMOS and PSP image receptors in terms of time efficiency and artifact incidence using phantom jaws. A total of 62 fourth year students participated and took images from 8 different regions using the Manikin Set. PSP and CMOS receptors were used for the right and left regions of the jaws.
Results: The time required for sensor placement, cone and phantom head positioning, and image formation, along with time required for the entire procedure, was recorded for each region. Thereafter, various artifacts were identified through the consensus of the same three researchers, with P < 0.05 indicating statistical significance. In general, CMOS detectors showed better time efficiency than did PSP detectors. Both detectors performed equally well in terms of artifact formation during student training. When using the CMOS detector, students spent the most amount of time placing the sensor in the upper premolar region. Analysis of variance was used to compare the regions according to detector type.
Conclusion: The clinical utility and educational significance of the findings presented in the current should be carefully evaluated.
Keywords: Digital Imaging; Photostimulable Phosphor; CMOS; Detector
Abbreviations: CCD: Charge-Coupled Device; CMOS: Complementary Metal Oxide Semiconductor; PSP: Photostimulable Phosphor Plate; FMS: Full Mouth Series; ANOVA: Analysis of Variance
Intraoral radiography remains the most widely used radiographic technique in dentistry despite the development of new diagnostic methods [1]. With the advancement of technology, digital radiography techniques, which are now being used as an alternative to conventional imaging methods in routine clinical applications, have almost replaced film imaging and is widely popular among dentists [2]. The most important reasons for the widespread use of digital radiography systems in dentistry include time efficiency in image acquisition, high image quality, reduction of repetitive images, good contrast resolution, and easy storage and transmission of images [3]. Digital intraoral receptors have been widely popular in dentistry for the last 20 years due to their advantages, which include a 50%–95% reduction in patient radiation dosage compared to conventional techniques, the nonrequirement of bathroom and dark room procedures, and image enhancement that enables brightness and contrast adjustment according to the clinician's needs [4,5]. Digital radiography differs from traditional radiography in the receptors and methods used to obtain the image. In conventional systems, the image is created directly on a film, whereas in digital systems, the signal detected by the sensors is digitized [3]. Currently, three intraoral digital sensors are available for purchase, namely a charge-coupled device (CCD) with a direct digital receiver, a complementary metal oxide semiconductor (CMOS), and a photostimulable phosphor plate (PSP) with an indirect digital image receiver [6].
CMOS detectors are silicon-based semiconductors that contain a silicon-based chip sensitive to X-rays and light. The chip consists of rectangular arrays of pixels and atoms in silicon forming covalent bonds with each other. These covalent bonds are separated by X-rays, which creates an electrical charge. Each pixel is connected to the transistor independent of the neighboring pixels. The electrical charge applied to the pixel is directly proportional to the absorbed X-rays and is transmitted to a converter as a small voltage. The voltage generated in each transistor is stored separately, read, and displayed as a digital gray value [7-11]. The primary advantage of solid-state sensors is that the image obtained can be viewed immediately; however, these sensors are expensive and difficult to place within the patient’s oral cavity [12]. CMOS sensors consume less power, are cheaper to manufacture, and contain sensors that are built into the circuit, which is beneficial for clinical dentistry. Nonetheless, it does have some disadvantages, which include a more stable model noise and a smaller active area due to the integrated circuit [13]. The PSP system, which uses photostimulable phosphor luminescence plates, functions by transferring the analog image to digital media with the help of a scanner and can therefore be classified as a semi-direct technique [2]. PSPs contain europiumdoped barium fluorohalide. The plaque, which can be used repeatedly, absorbs, and stores the photonic energy generated when excited by the X-ray. When the excited fluorohalide complex is scanned with red and green laser lights, fluorescent light proportional to the absorbed X-ray dosage is produced and then converted into an amplified electrical signal.
This analog signal is converted to a digital signal and transferred to a computer where it can be visualized [14-16]. The biggest disadvantage of CMOS detectors is that they are hard and thick, which can cause placement errors and discomfort for the patient. PSP detectors consist of imaging plates that have the same shape and dimensions as conventional films but are placed in a sharp-edged plastic envelope to avoid inter-patient contamination, which can cause placement problems for the practitioner. Furthermore, the receptors are quite expensive [17-19]. The advantages of PSP systems are that only a minimal change in technique is required to switch from film-based imaging and that PSPs are as thin as conventional films. However, PSPs require longer imaging times than CMOS detector while also having a shorter receptor lifetime owing to their lack of resistance to physical bending and twisting [12]. An important benefit of PSP systems is that they require no cable connection between the sensor and the computer. Phosphorus plates have the same imaging area as periapical film No. 2 (31 × 41 mm) in the mouth, which is wider than that in CCD sensors [5,12]. In addition, the size and flexibility of the plates used in PSP systems introduced in recent years are similar to those used in periapical films, which makes its manipulation easier [20]. Although the radiation risk associated with dentomaxillofacial region imaging might be considered low for individual patients, such a risk becomes a major concern when extrapolated to a large patient population exposed to diagnostic dental imaging. Reducing radiation exposure to “as low as diagnostically acceptable” has become an important objective in radiology.
Although digital imaging systems considerably decrease patient radiation dosages, a full mouth evaluation might be necessary in order to obtain adequate diagnostic imaging. Full Mouth Series radiographs provide images of all teeth. When cysts or tumors are suspected in the mouth, a full mouth examination, as well as important dental examinations such as root canals, extractions, and gum disease treatment, can be performed. In terms of radiation protection, full mouth examinations should be performed only when necessary indications are apparent. Periodontal diseases and dental caries are among the biggest public health problems in many countries of the worldwide. In low- and middle-income countries, oral hygiene habits are not optimal, which promotes various oral problems such as periodontal disease and caries. These problems make full mouth radiological evaluation inevitable [21]. Several published studies have compared the duration of imaging procedures and imaging errors between CMOS/CCD and PSP systems [22-24]. However, to the best of our knowledge, no previous study has compared different digital detectors using radiological phantom models for teaching dentistry students. Considering the importance of possible differences between various intraoral detectors in terms of time efficacy and artifacts that might cause repeats, we compared CMOS and PSP image receptors on phantom jaws used for teaching dental faculty students. Our secondary was to determine the regions in which students needed the most practice and emphasis during their education based on calculated placement and positioning times.
Helsinki Declaration and Ankara University Dentistry Faculty Ethical Committee approval was obtained for the present study (IRB No: 69/2022). A total of 62 fourth-year graduate dental students participated in the present study. Students took images from eight different oral regions (anterior, maxillary canine, mandibular ca-nine, maxillary premolar, mandibular premolar, maxillary molar, mandibular molar, and bitewing radiographs) using a Nissin Model 403072 Tripod X-Ray Manikin Set (Nissin, Tokyo, Japan; (Figure 1)). Images were obtained using the Kavo Gendex Expert DC (Des Plaines IL, USA) periapical Roentgen Unit at 65–70 kVp, 4–7 mA, and 0.05 s with the paralleling periapical technique and Rinn aiming devices. Two different im-age receptor types were used for the right and left regions of the jaws to ensure an equal number of usages for each receptor type. The two image receptor types selected were size 2–3 PSP plaque (scanned with Kavo Gendex GXPS-500 phosphor plate device, Helsinki, Finland) and a CMOS sensor (Kavo Gendex GXS-700 model, Helsinki, Finland; (Figure 2)). The time required for sensor placement, cone and phantom head positioning, image formation, and the time required for all procedures were calculated and recorded for each region using a stopwatch by consensus of three oral and maxillofacial radiology residents (EP, AD, and BI). Graduate dentistry students who voluntarily participated in the study were instructed regarding the study design, materials, and usage of radiological devices in a prior pilot session conducted by three oral and maxillofacial radiology residents (EP, AD, and BI). Thereafter, artifacts were classified as cone cut, positioning errors, and horizontal/vertical angulation errors by consensus of the same researchers.
Statistical Analysis
Descriptive statistics for each variable were calculated and presented as: “mean ± standard error of mean.” For hypothesis testing, data were subjected to two-way analysis of variance (ANOVA) to compare the time for different regions to the different sensor types. The model included “region” and “sensor type” as the main effects and “region*sensor type” interaction effects. Post-hoc testing was performed using simple effect analysis with Bonferroni adjustment. The frequency of artifacts among different regions for each sensor type were determine using Chi-squared analysis. Tests were adjusted for all pairwise comparisons within a row for each innermost comparisons using Bonferroni correction. To evaluate insertion and positioning times for different sensor types according to gender, data were subjected to two-way ANOVA. The model included “gender” and “sensor type” as the main effects and “gender*sensor type” interaction effects. Post-hoc testing was performed using simple effect analysis with Bonferroni adjustment. A probability value of less than 0.05 was considered significant, unless otherwise noted. All statistical analyses were performed using SPSS version 21.
A total of 992 intraoral digital periapical and bitewing digital radiographic images (496 CMOS and 496 PSP) were assessed. (Table 1) compares the time required for various procedures (detector placement/cone positioning and image formation) for CMOS and PSP sensor types and for different regions (Figure 3). The longest detector placement time for CMOS was observed in the maxillary premolar region (51.9 ± 3.43 s), whereas the shortest for the same detector was observed in the mandibular molar region (24.23 ± 1.99 s). Although significant differences in detector placement times were observed among regions, no significant difference in detector placement times were observed between the two detectors (Table 1a; P ≥ 0.05). For both CMOS and PSP detectors, the longest time for positioning and aiming was found for the mandibular canine region (CMOS: 27.53 ± 2.33 s; PSP: 37.63 ± 3.02 s), whereas the shortest time was found in the mandibular molar region (CMOS: 14.83 ± 1.48 s; PSP: 22.96 ± 1.94 s). Positioning and cone aiming times were significantly shorter for CMOS detectors than for PSP detectors considering all regions imaged (Table 1b; P < 0.001). Image formation times were significantly shorter for the CMOS detector than for the PSP detector in periapical radiographs taken from all regions (Table 1c; P < 0.001).
Table 1: Comparison of the times (placement/positioning/image formation time by regions for different detector types (CMOS/PSP). Data were subjected to two-way ANOVA (analysis of variance). The model included “region” and “detector type” as the main effects and “region*detector type” interaction effects. Post hoc testing was performed using simple effect analysis with Bonferroni adjustment.
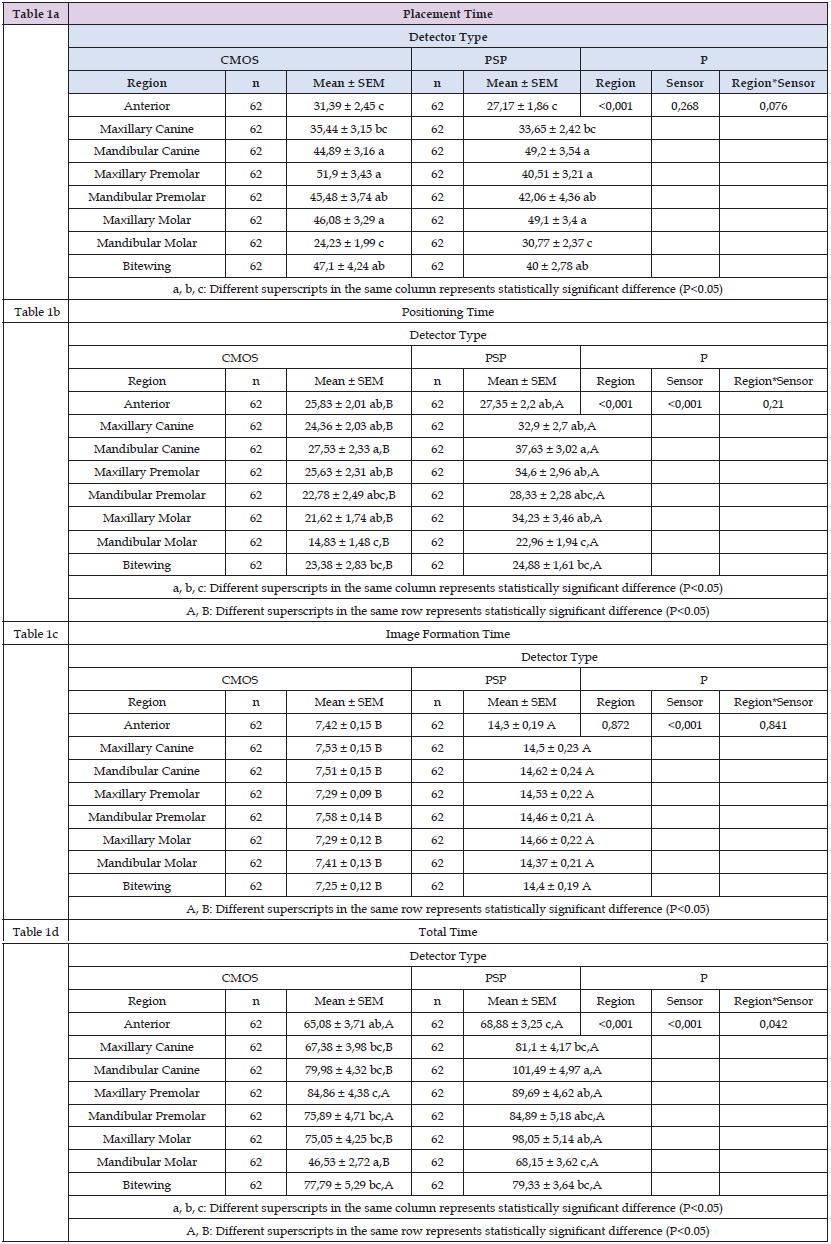
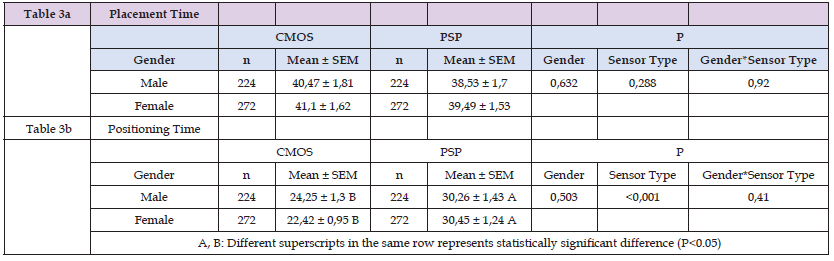
The total time was shortest for both CMOS and PSP detectors, the total time was shortest in the mandibular molar region (CMOS: 46.53 ± 2.72 s, PSP: 68.15 ± 3.62 s). For the CMOS detector, the total time was longest in the maxillary premolar region (84.86 ± 4.38 s), whereas for the PSP detector, the total time was longest in the mandibular canine region (101.49 ± 4.97 s). The total time for the radiographs taken from the maxillary canine, mandibular canine, maxillary molar, and mandibular molar regions was found to be significantly shorter in the CMOS detector than in the PSP detector (Table 1d; P < 0.001). Comparison of various artifacts (cone cut: 1, placement error: 2, horizontal angulation: 3, and vertical angulation: 4) according to the two detector types and region (Table 2 & Figure 4). For both detector types and all regions, the most common type of artifact was positioning error, whereas the most common region where positioning errors were observed was the maxillary premolar region (CMOS: 16.4%; PSP: 17.8%). The region where all artifacts were least observed was the anterior region. Significantly fewer placement errors were found in bitewing radiographs taken with the CMOS detector than in periapical radiographs taken from all other regions (8.4%). More horizontal angulation errors were found in radiographs taken from the maxillary canine region with the CMOS receptor than in those taken in other regions (26.9%). Bitewing radiographs taken with the CMOS detector showed a lower rate of vertical angulation error compared to the PSP. (1%; P = 0.018). No significant differences in placement and positioning times were observed among different detector types according to gender (Table 3; P ≥ 0.05).
Table 2: The incidence and comparison of various artifacts 1. Cone cut, 2. Placement Error, 3. Horizontal Angulation, 4. Vertical Angulation, for different detector types (CMOS/PSP) according to regions. Frequency of artifacts among different regions for each detector type were investigated using a Chi-square analysis. Tests were adjusted for all pairwise comparisons within a row of each innermost sub table using Bonferroni correction.
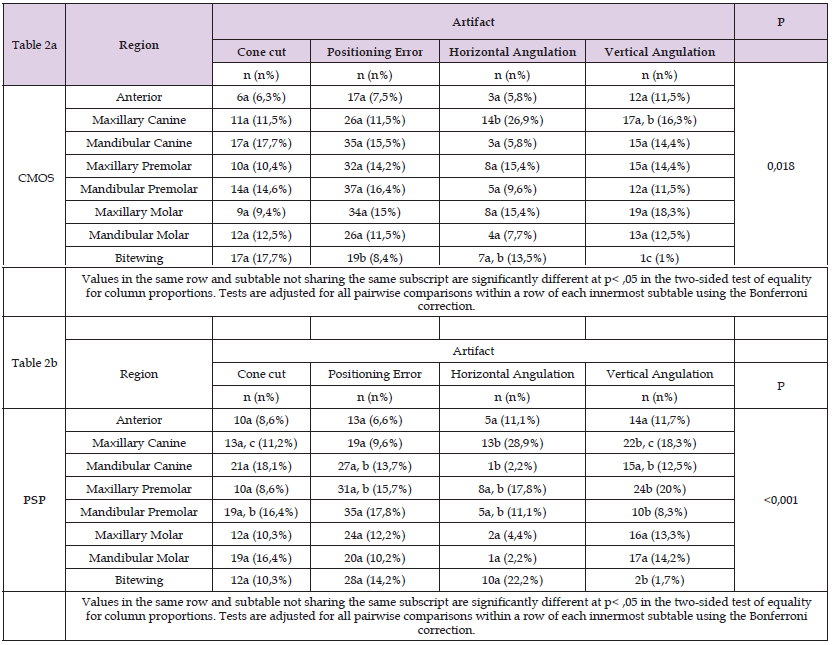
Table 3: Evaluation of placement and positioning times for different detector types according to gender.
Improving the image quality of digital intraoral X-ray imaging is necessary for accurate diagnosis. Various characteristics, such as pixel value, noise, low contrast resolution, and spatial resolution, have been used to objectively evaluate image quality. Physical performance measurements eliminate changes that might result from observers or samples; however, although these measurements provide quantitative results, they are insufficient for assessing observer performance [25,26]. The potential limitations associated with the imaging of patients were not relevant for the current study given that we used phantoms for imaging procedures. Therefore, patient-related problems, such as movement artifacts, gag reflex, superficial floor of the mouth, limited mouth opening, and lack of manipulation, were eliminated by using phantom models, allowing for a more objective comparison of PSP and CMOS detectors. In recent years, CMOS or PSP detectors have been used routinely for intraoral imaging in dental practice. Our results found that for imaging during student teaching, CMOS detectors were less time consuming than PSP detectors while having the advantage of simultaneous image acquisition. No difference in artifact formation was observed between both detectors. During image acquisition using these detectors, various artifacts can appear on the image depending on the characteristics of the user, patient, and detector.
The clinical diagnostic capacity of the acquired image and the occurrence of these errors can be affected by several variables, including central X-ray angle, exposure time, detector sensitivity, image acquisition, imaging conditions, superposition of teeth and anatomical structures, and practitioner- and patient-dependent factors [19,23,24,27-29]. Given the potential differences in clinical efficacy between available detectors, the current study compared the commonly used CMOS and PSP detectors manufactured by the same company in terms of insertion and positioning time, image formation time, and resulting artifacts. Comparisons were made using phantom models, which eliminated patient-related factors that could affect insertion time and artifacts. To strengthen the education provided to dentomaxillofacial radiology students, the current study was conducted on fourth-year intern dental students. The inexperience of these student practitioners with the use of the two detector systems ensured the objective assessment of procedural times and artifacts. Ramamurthy, et al. [30], who compared two PSP systems using phantom models, similar to our study, in terms of plate erasure, packaging, positioning/exposure, un-packing, loading processor, scanning, and image transfer to virtual full mouth series (FMS) times, found no significant difference in the total time spent when producing the FMS. The current study found that the artifact ratio in the images created using PSP and CMOS detectors was the same. However, more placement-related errors were observed in images created using CMOS than in those created using PSP, albeit not significantly (Table 3a & 3b). Farrier, et al. [31] reported more repetitions for CCD than for PSP.
They attributed this to the fact that CCD detectors were larger and stiffer than PSP imaging plates, CCD had an attached cable, and patients had difficulty tolerating CCD detectors in the mouth [31]. In addition, two surveys conducted among dentists noted significant problems with the positioning of CCD detectors, which promoted more repetitive images with CCD than with PSP systems [27,28]. Although patient tolerance of CMOS detectors was not an issue given our use of phantom models, the occurrence of more placement errors in some regions of the mouth when using CMOS detectors suggests that placement errors might be largely caused by volume and hardness differences between detectors. Kamburoglu, et al. [24] found that the mean value of the total time for all imaging procedures was significantly shorter with a CMOS detector than with the PSP detector (P < 0.05). No significant differences in detector insertion time and positioning time were found between PSP and CMOS detectors (P > 0.05). Wenzel et al. compared students' attitudes toward digital radiography and measurement accuracy in intraoral radiographs obtained using a CCD detector and PSP plate system in conjunction with root canal treatment. Accordingly, students stated that they saved more time (P < 0.001) when using CCD detectors than when using PSP detectors; however, they stated that PSP detectors were easier to place in the oral cavity than were CCD detectors (P < 0.01). Although the current study found no significant difference in insertion time between the two detectors, our comparison of the total duration for all imaging procedures found that CMOS detectors had better time effectiveness than PSP detectors in accordance with previous studies [23,24]. Due to the physical disadvantages of CMOS detectors, higher insertion times were expected compared to PSP, but this difference was not statistically significant.
Several studies have also evaluated the effects of sensors on image quality. In-deed, Aydin et al., who compared image quality between PSP and CMOS systems by evaluating contrast resolution between four different exposure times, found that the PSP system had a higher contrast resolution. Another report also showed that the PSP system had significantly higher pixel values than did the CMOS system (P < 0.05). However, no subjective assessment of image quality was conducted in the mentioned study [32]. Aziman et al., who compared subjective image quality between CCD and CMOS detectors, found no significant difference between the two systems [33]. Wenzel et al. compared digital and conventional imaging in terms of time used in their survey. For general dentists using digital imaging, they reported that using digital imaging saved approximately half an hour per day in time spent on radiographic procedures [22]. Russo et al. stated that pediatric dentists obtained images faster with sensors than with phosphor plates. They also reported that although the sensor technology produced images faster than did phosphor plates, sensors were less tolerated by younger children due to its size and thickness. In contrast, phosphorus plates have been recognized as more child-friendly and less expensive but less durable [34]. Although a few studies have compared digital receptors with films in terms of time efficiency or working time, it seems reasonable to conclude that digital imaging systems save time when used in routine dental practice [1].
Results of various survey studies comparing reimaging and imaging errors between conventional and digital image formation have found that dentists working with digital receptors performed more reimaging procedures with digital sensors than with films [22,28]. Furthermore, another study of images sent to an insurance company showed that digital images had much more positioning errors than did film-based images [35]. However, we should note that the mentioned studies were conducted in the early years of the transition to digital systems. Today, however, most radiographers and clinicians are considerably more experienced in the implementation and application of digital intraoral systems. Anissi, et al. explored the distribution and application of digital intraoral radiographic techniques by comparing them with film-based systems in terms of patient dose reduction. Accordingly, CCD system users noted difficulties in positioning the detector and retakes due to poor images. Users of the PSP system mentioned faster image generation and lower radiation dose during diagnosis compared to the CCD system. There appears to be little to no problem with detector positioning in PSP systems, thereby resulting in only a few retakes [36].
Although CMOS and CCD sensors are more radiation sensitive than PSP plates for a single exposure, this advantage is negated due to the need for more retakes in daily clinical situations [25].
Golçalves, et al. evaluated patient comfort during the simulation of the periapical radiographic examination using a CCD sensor, photostimulatory phosphor plate, and conventional radiographic film. Accordingly, they found that the bilateral lower premolar and lower right molar regions were the least comfortable, regardless of the type of imaging receptor used. These findings were attributed to the location of the lower premolar region in the curvature of the adjacent dental arch, where the floor of the mouth was relatively small. In addition, overall patient comfort was similar for other regions [37]. The current study also compared PSP and CMOS detectors in terms of intraoral insertion time, cone positioning time, image formation time, and emerging artifacts according to the region where the image was taken. Considering that our study had been the first to compare PSP and CMOS detectors from the same manufacturer using phantom models, a direct comparison with an identical study could not be made. The results of the current study are novel and could contribute to the practical training of dental students during clinical apprenticeship in the dentomaxillofacial radiology department. The limitations of the current study include our inability to evaluate patient-related artifacts and image quality. One significant finding of our study was that students spent a considerable amount of time placing the detectors in the maxillary premolar region when using the CMOS detector. Notably, students spent most of their time positioning both detectors in the lower canine region. Considering the placement-related error rates of the students in the images created using the PSP and CMOS detectors, students were more comfortable using a PSP detector than a CMOS detector. The findings of the current study, which used both CMOS and PSP detectors, should be carefully considered with regard to applicability in routine clinical use.
Training on phantom models ensures that students are best prepared for clinical practice. This training helps students learn the regions in which they should most accurately position the detectors in the patient's mouth. In addition, phantom models provide the students with the opportunity to practice on the regions where they make mistakes during imaging. However, these procedures should be carefully monitored by the instructor. Although the radiation received by the patient is not an issue, the practitioner might be affected by scattered radiation during this process. A study by Basah, et al., which examined the level of knowledge of recent dental graduates on radiation protection, found that participants had moderate knowledge [37]. A survey-based study in Poland by Furmaniak et al., which assessed the aware-ness of radiation protection among 301 dental students who returned their questionnaires, found that students had limited knowledge regarding radiation protection [38]. Considering that dentists are at risk of radiation exposure and its associated hazards throughout their careers, it is important that dentists are aware of the parameters of radiation exposure and protective measures to minimize the undesirable effects of radiation.
Instructors need to provide the students with the appropriate level of training in radiation protection and application of the “as low as reasonably achievable” and “as low as diagnostically acceptable” recommendations. Nevertheless, training on phantom models will minimize student errors on patients, thereby reducing the number of repetitions in films and the possibility of being affected by indirect radiation. Considering the deterministic and stochastic effects of radiation on cells, accurate use of diagnostic techniques is of paramount importance. Therefore, during practical dentomaxillofacial radiology training, specific attention should be directed toward regions where students require more training.
Despite the limitations of the current study, our findings revealed that CMOS detectors showed generally better time efficiency than did PSP detectors. Both detectors performed equally well in terms of artifact formation during student training. After examining the students' performances on both detectors, we found that the most noticeable errors were those related to positioning. We also found that students made placement errors mostly in the maxillary premolar region. Considering these results, we recommended that practical exercises be conducted as part of training programs and be directed toward specific regions in an attempt to minimize errors.
This research was supported by Ankara University Scientific Research Coordination Unit Project No: 19A0234002.
The authors declare no conflict of interest.


