Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Si Zhang, Yue Wang, Lixin Guan and Cuihong Lian*
Received: September 04, 2023; Published: September 11, 2023
*Corresponding author: Cuihong Lian, Department of Dermatology, Shenzhen Second People’s Hospital, No.3002 Sungang West Road, Shenzhen, 518025, China
DOI: 10.26717/BJSTR.2023.52.008309
Abbreviations: BD: Behçet Disease; ESR: Erythrocyte Sedimentation Rate; CRP: C-Reactive Protein; HSV: Herpes Simplex Virus; JAK: Janus Kinase; ACR: American Criteria of Rheumatology; MHC: Major Histocompatibility Complex; TNF: Tumor Necrosis Factor; eNOS: Endothelial Nitric Oxide Synthetase; STAT: Signal Transducer and Activator of Transcription; PBMCS: Peripheral Blood Mononuclear Cells
A 41-year-old male presented with recurrent oral and genital ulcers, erythema of proximal extremities, polyarthralgia and fatigue for three years. Over two years ago, he was diagnosed with Behçet disease (BD) at another hospital, based on the manifestations of orogential ulcerations (frequency of oral ulcers was greater than three times per year), erythematous and papulopustular skin lesions, a positive skin puncture, and arthritis. During dermatological examination, scattered aphthous lesions on the oral mucosa and erythema on the scrotum and penis were observed. Annular and reticular darkred patches were observed on the proximal extremities, axilla, groin, and buttocks, which had a well-defined border with crusted pustules on the surface (Figures 1A-1D). There were no ocular symptoms or other systemic conditions. The patient denied family history of any diseases, and there were no other physical illnesses. Laboratory tests revealed leukocytosis (13,400/L) with a dominant neutrophil classification (81%), an erythrocyte sedimentation rate (ESR) of 57 mm/h [<5 mg/l], C-reactive protein (CRP) of 69 mg/l [<5 mg/l], and elevated serum globulin-γ. Liver function, renal function and urine analysis were unremarkable. Autoantibody profiles were negative, including antinuclear antibodies, anticardiolipin antibodies, rheumatoid factor, antineutrophil cytoplasmic antibodies, and lupus anticoagulants.
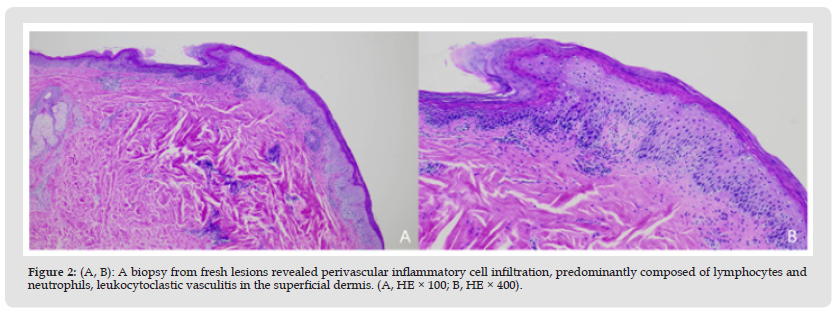
Initial examination for infectious diseases, including blood cultures, human immunodeficiency virus screen, herpes simplex virus (HSV)-1, and two nucleic acid amplifications, hepatitis B, hepatitis C, and varicella zoster virus directly-labeled fluorescent antibody were negative. Cultures for fungi and bacteria obtained from mucocutaneous lesions were negative. No abnormalities were found on chest radiographs, electrocardiograms or abdominal ultrasound. A biopsy from fresh lesions revealed perivascular inflammatory cell infiltration, predominantly composed of lymphocytes and neutrophils, leukocytoclastic vasculitis in the superficial dermis (Figures 2A & 2B). Despite long-term administration of corticosteroids plus colchicine, recurrent oral ulcerations, erythematous lesions, and arthralgia were observed. Because of the efficacy of Janus kinase (JAK) inhibitors for refractory BD, Abrocitinib 100 mg was given once daily, and glucocorticoids and colchicine were discontinued. Two weeks after treatment with Abrocitinib, the patient’s symptoms improved, and the erythema, oral ulcerations, arthralgia and fatigue gradually disappeared. The patient has been receiving Abrocitinib for three months, and his original lesions have disappeared, leaving pigmentation, with normalized leukocyte counts, CRP levels and ESR (Figures 1E & 1H). The patient is currently under follow-up.
Figure 1 (A-D): Dermatological examination showed scattered aphthous lesions on the oral mucosa and erythema on the scrotum and penis. Annular and reticular dark-red patches were observed on the proximal extremities, axilla, groin, and buttocks, which had a well-defined border with crusted pustules on the surface. (E-H). The clinical pictures after treatment. The patient has received Abrocitinib for three months without any new lesions and the original lesions have faded, leaving pigmentation.
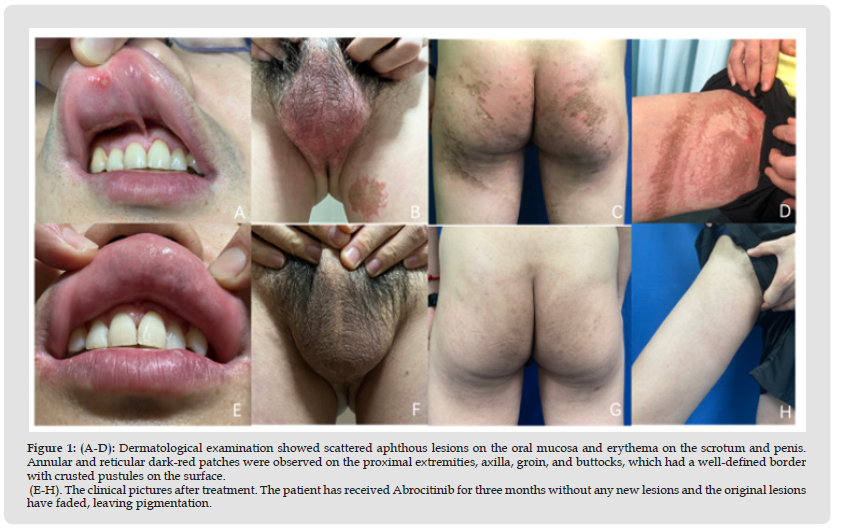
Figure 2 (A, B): A biopsy from fresh lesions revealed perivascular inflammatory cell infiltration, predominantly composed of lymphocytes and neutrophils, leukocytoclastic vasculitis in the superficial dermis. (A, HE × 100; B, HE × 400).
BD is known as a chronic systemic inflammatory disorder with widespread vasculitis, characterized by oral aphthae, genital ulcerations and uveitis, as well as several systemic manifestations. The disease affects men more than women, with a peak incidence in the third decade [1]. Cutaneous manifestations are a feature of BD and are classified as a major diagnostic criteria. The American Criteria of Rheumatology (ACR) proposes five diagnostic criteria for BD, which include the presence of recurrent oral ulceration accompanied by any two of the following symptoms: recurrent genital ulceration, ocular lesions, cutaneous lesions, or positive pathergy test results. Several cutaneous manifestations have been described, including erythema multiforme-like lesions, palpable purpura, Sweet syndrome-like lesions, infiltrated erythema, hemorrhagic bullae, extragenital ulcerations, and thrombophlebitis [2]. The etiology and pathogenesis of BD are unclear, however, it is believed to be due to an autoimmune process triggered by environmental or infectious agents, such as herpes virus or streptococcus in a genetically predisposed individual. Previous genetic studies have identified the HLA-B51 allele, located in the major histocompatibility complex (MHC) locus on chromosome 6p, as the genetic risk factor most closely associated with BD. Several other genes have been proposed to be involved in BD pathogenesis, including HLA-B5701, HLA-A26, tumor necrosis factor (TNF) polymorphisms, genes related to interleukin-1 (IL-1), coagulation factor V, intercellular adhesion molecule-1 (ICAM-1), and endothelial nitric oxide synthetase (eNOS) [3].
BD is also known to be associated with gender, smoking, and exogenous factors, such as diet, stress and infections (especially herpes simplex virus-1 and Streptococcus sanguis) [4]. An imbalance in the number of T cells (especially Th1, Th2, and Th17 helper cells), natural killer cells, and inflammatory cytokines have been shown to contribute to the pathogenesis of BD. Previous studies have shown Th1-type polarization of immune responses in BD, the intensity of which is related to disease activity. Cytokines such as IL-1, IL-4, IL-6, IL-12, IL-13, IL-17, IL-23, and TNF- have been implicated in the pathogenesis of BD [5]. The Janus kinase (JAK) and signal transducer and activator of transcription (STAT) pathway are important in BD. Tulunay, et al. [6] performed whole-genome microarray profiling using human U133 (Plus 2.0) chips to investigate this canonical STAT pathway in peripheral blood mononuclear cells (PBMCs) from patients with BD. They observed that JAK-1 was upregulated and JAK/STAT signaling was activated in both CD14+ monocytes and CD4+ T lymphocytes of BD patients [6]. The Th1/Th17 cell responses are upregulated in BD. The JAK-1/STAT3 signaling pathway is derived from the activity of Th1 and Th17 cytokines, such as IL-2, interferon (IFN-γ), IL-6, IL-17, and IL-23 [7]. JAK-1 signaling has been shown to play an important role in the pathogenesis of BD, and currently, JAK inhibitors are available for treatment.
In a recent pilot study, Liu and colleagues reported the efficacy and safety of tofacitinib (a small-molecule pan-JAK inhibitor) in refractory BD patients with active vascular/cardiac, gastrointestinal, and joint involvement [8]. Moreover, Wang et al. reported a 27-yearold woman who was diagnosed with refractory BD and successfully treated with tofacitinib [9]. However, although no reports on JAK-1 inhibitors (highly selective JAK inhibitors) for BD treatment are available, the clinical observations from this study implicated the therapeutic efficacy of Abrocitinib (a JAK-1 inhibitor) in controlling the disease activity of BD.
None.
None.
All authors have contributed significantly, and that all authors are in agreement with the content of the manuscript. On behalf of all the contributors I will act and guarantor and will correspond with the journal from this point onward.


