Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Verhaz Antonija1,2* and Panic Ognjen1
Received: August 05, 2023; Published: August 18, 2023
*Corresponding author: Verhaz Antonija, Clinic for Infectious Diseases, University Clinical Center of the Republic of Srpska, Banja Luka, Banja Luka, Bosnia & Herzegovina
DOI: 10.26717/BJSTR.2023.52.008235
Introduction/Aim: Acute brain dysfunction, commonly diagnosed as encephalitis or encephalopathy, occurs in association with influenza. The diagnosis is always difficult to establish due to the absence of characteristic clinical symptoms and valid diagnostic criteria. Acute influenza-associated encephalopathy/ encephalitis (AIE) mainly occurs in the pediatric population, while it is a rare complication in adults. We present an overview of acute cases of IAE in patients treated at the Banja Luka Infectious Diseases Clinic in the 2019 flu season.
Methods: Patients with suspected encephalitis were prospectively identified in the Clinic for Infectious Diseases of Republika Srpska Banja Luka. The primary neurological complications associated with influenza are classified into 3 groups: encephalopathy, encephalitis and meningitis. For this analysis, we excluded cases associated with laboratory identification of the influenza virus; among these cases, specific IAE syndromes where clinical and radiological features were consistent with descriptions in the published literature were identified.
Results: We included a total of 8 patients. Confusion and seizures were the most common neurological symptoms, present in 8 (100 %) patients. Magnetic resonance or computed tomography was performed in 4 patients, and anomalies were found in 4 with lesions throughout the brain. Laboratory diagnostics consists of proving the RNA of the influenza virus in respiratory samples, which was detected in all patients. Three of the eight patients died.
Discussion: The results show that many different neurological symptoms can be present in patients with acute onset of IAE. Therefore, the diagnosis should be considered in patients with fever and neurological symptoms, especially during the flu season. Laboratory diagnostics consists of proving the RNA of the influenza virus in respiratory samples.
Conclusion: Vaccination plays an important role in preventing not only influenza, but also severe neurological complications during influenza.
Keywords: H1N1 Virus; Neurological Complications
Abbreviations: IAE: Influenza-Associated Encephalopathy/Encephalitis; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; RT-PCR: Reverse Transcriptase Polymerase Chain Reaction
Some CNS diseases have been reported to accompany influenza infection, including Reye’s syndrome, influenza-associated encephalitis/ encephalopathy, myelitis, and acute necrotizing encephalitis [1]. Patients with encephalopathy show a disturbance of consciousness that lasts more than 24 hours, and patients with encephalitis have a high temperature and focal neurological signs. Neurological complications of influenza infection are a rare but well-known cause of morbidity and mortality in children and adults worldwide, and their incidence appears to have increased following the 2009 influenza A H1N1 pandemic [2-4]. Influenza-associated encephalopathy/encephalitis (IAE) is a neurological condition associated with influenza virus infection. The diagnosis is difficult because there is no unique clinical picture, the influenza virus is rarely detected in the cerebrospinal fluid (CSF), and it can no longer be detected in respiratory samples when the patient presents with neurological symptoms. Furthermore, there are no validated diagnostic criteria for this condition in adults [1,2]. Influenza virus is the most important cause of acute encephalopathy. In Japan, 100-500 cases of encephalopathy caused by influenza occur each year. Influenza virus A/H3 shows a higher incidence of encephalopathy compared to viruses A/H1 and B [5]. In particular, influenza-induced encephalopathy accounts for 40-50% of patients with Reye’s syndrome and acute necrotizing encephalopathy [3]. The overall death rate from influenza-induced encephalopathy was about 30% before 2000, but after 2000 it dropped to about 15% [4-6]. Recently, reports of influenza-associated encephalitis/encephalopathy have increased in Japan, particularly in children under 5 years of age. During the winter of 1997-1998. and in 1998-1999, when the influenza A (H3N2) epidemic broke out, many pediatricians reported cases of influenza-associated encephalitis/encephalopathy [4-6]. In the case of a sudden onset of seizures a few days after the development of elevated body temperature in the course of influenza infection, one should think about involvement of the central nervous system.
In this study we present prospectively collected surveillance data on the neurologic complications of influenza A (H1N1) 2019 in adults. The clinical, laboratory and virologic findings for these cases are reported.
The diagnosis is difficult because there is no uniform clinical presentation. Influenza virus is rarely detected in cerebrospinal fluid and may no always be detectable in respiratory samples when the patient presents with neurological symptoms. The database included age, gender, medical and vaccination history, clinical presentation, diagnostic test results, treatment, clinical course, and outcome. Neurologic complications were defined as symptoms or signs associated with laboratory-confirmed influenza A (H1N1) 2019 infection that affected the central or peripheral nervous system including seizures, encephalopathy, encephalitis, or any focal neurologic symptom. A diagnosis of encephalitis was made either clinically or laboratory as per standard definitions. Encephalopathy was defined as altered level of consciousness for more than 24 hours, including lethargy, irritability, or change in personality and behavior [1,2]. Patients admitted to participating hospitals with signs and symptoms of influenza routinely had nose and throat swab for influenza testing (PCR). The diagnosis was based on clinical and laboratory findings, magnetic resonance imaging (MRI) or computed tomography (CT) imagining, isolation of influenza A virus from nasopharyngeal aspirate. The information collected included demographic characteristics, clinical signs and symptoms, history of chronic illnesses, and onset and duration of respiratory and neurological symptoms. Electroencephalographic and neuroradiographic findings (by CT and MRI) were obtained and selected blood chemical values determined at the time of admission to the hospital. The cerebrospinal fluid (CSF) with pleocytosis and total protein level were analyzed [7].
In the 2018/19 season, a total of 78,328 ARIs (acute respiratory infections) and 20,877 ILIs (influenza-like infections) were reported in the Republic of Srpska. Most cases of ILI are in the age group 30- 64 and 5-14 years. years. Hospitals of Republika Srpska reported 772 cases of SARS (severe respiratory infections). During the influenza A (H1N1) epidemic in the Republic of Srpska, from January 2019 to April 2019, in the Clinical Clinical Center of the Clinic for Infectious Diseases of the Republic of Srpska, we treated five patients with encephalitis, two with encephalopathy and one with acute meningitis. Banja Luka. The patients had not received a vaccine against influenza A and B, nor had they previously suffered from any neurological disorder. The clinical picture and epidemiological data indicate influenza. Influenza-related encephalitis/ encephalopathy was diagnosed in 8 patients (5 men and 3 women). Of these 8 patients, one was 7 years old. Patients ranged in age from 7 to 82 years, with a mean age of 54.5 years. In two patients, the symptoms of encephalitis appeared in the first 48 hours, and in five patients, on the 4th to 7th day after the onset of the flu. In one patient, acute meningitis manifested itself on the 10th day after the first symptoms of influenza as a secondary bacterial infection.
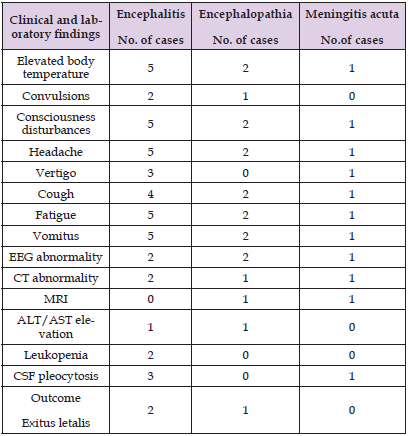
A very severe manifestation of encephalitis was noted in patients who developed in the early course of the underlying disease, influenza A. In two patients, the initial sudden manifestation of encephalitis included focal seizures and deep coma. The main clinical signs reported are loss of consciousness, convulsions, cough and vomiting (Table 1). One third of patients had convulsions or coma on the day of fever onset. All our patients (100%) had elevated body temperature (> 40 °C) (Table 1), and previously had headache and generalized fatigue. Dizziness and cough are present in four and seven, disturbances of consciousness up to deep coma in all patients. Two patients had marked leukopenia without granulocytopenia. Elevated serum levels of aspartate aminotransferase and alanine aminotransferase were noted in two patients. Electroencephalogram (EEG) was normal in three patients. For five patients, EEG findings were abnormal. Brain CT revealed abnormalities in four patients. The most common findings observed in patients were brain edema and low density in localized areas, such as the thalamus, brainstem, and parenchyma. Magnetic resonance imaging studies were performed for two of the eight patients. CSF was performed in 7 patients, and three patients had normal findings. EEG = electroencephalogram; CT = computed tomography; ALT = alanine aminotransferase; AST = aspartate aminotransferase; CSF = cerebrospinal fluid Reverse transcriptase polymerase chain reaction (RT-PCR) analysis of nasal secretions confirmed H1N1 virus infection; cerebrospinal fluid was not tested for H1N1 viral RNA. All of them had positive RT-PCR on a nasopharyngeal swab tested for virus influenza A (H1N1) pdm09.
Table 1: Clinical and laboratory findings of encephalitis during Influenza A.
Note: Data are weight and FBG parameters and are expressed as mean ± standard error of mean (SEM, n = 5).
The clinical picture and epidemiological data pointed to influenza, whereas encephalitis of another etiology (Leptospira, tick-borne meningoencephalitis, cytomegalovirus, herpes simplex virus 1 and 2, and enteroviruses) were ruled out in six patients. Chronic diseases known to be risk factors for severe influenza were present in 7 of the 8 patients. None of the patients had a history of neurological disease. Three patients had diabetes. There were no patients with basic immune disease. Two patients had heart disease, and two patients had lung disease in the previous period. One had alcoholic liver disease or history of alcohol abuse. Chronic diseases were reported more often in patients who died than in patients who recovered. Treatment with oseltamivir was initiated. Initial antimicrobial therapy consisted of acyclovir and broad-spectrum antibiotics aimed at the most prevalent microorganisms causing infectious encephalitis. Four of these 8 patients received therapy with corticosteroids, and their conditions significantly improved. Of the 8 patients for whom outcomes were noted, three patients died due to rapidly progressing multiple-organ failure that occurred ⩽2 days after the development of neurological signs. Three patients died, five patients were discharged from the hospital as recovered.
In Influenza virus infection, in addition to upper respiratory tract diseases, there may be a complication in the form of an infection of the central nervous system. However, a number of authors in America, and especially in Japan, have described neurological complications in patients infected with H1N1 influenza. Neurological complications include encephalitis, encephalopathy, Reye’s syndrome and other neurological diseases [1-6]. Patients with encephalopathy have a disturbed state of consciousness for longer than 24 hours, and patients with encephalitis with a disturbed state of consciousness have a high temperature (over 38 °C), focal neurological signs and pathological cerebrospinal fluid [5]. Electroencephalographic changes can be indicative of encephalitis, and a pathological neuroimaging result is often present. In our eight patients, RT-PCR analysis of nasal secretions confirmed H1N1 virus infection; cerebrospinal fluid was not tested for H1N1 virus RNA. Prominent indicators of influenza-related encephalopathy are the sudden onset of seizures and coma within a few days of developing a high fever. These patients often develop multiple organ failure and have high morbidity and mortality. The pathogenesis of influenza-associated encephalopathy remains unclear. Because not all patients with influenza develop encephalopathy, influenza virus infection is necessary, but not sufficient, for the development of influenza-associated encephalopathy. Viral RNA is rarely detected in cerebrospinal fluid, and the presence of viral antigen in the brain has not been proven. Pathological findings, including the lack of detectable viral antigen and inflammatory cells in brain tissue, suggest that direct viral invasion and inflammation are probably not the causes of this disease [1,6].
In influenza-associated encephalopathy, serum and CSF concentrations of several proinflammatory cytokines and cytokine receptors-- such as interleukin (IL)-6, IL-1beta, and soluble tumor necrosis factor (TNF) receptor-1 (sTNF-R1) are elevated a are related to the clinical severity of the disease. Its pathogenesis is not fully elucidated; symptoms may be the result of an inflammatory response or viral neuroinvasion of the brain [7,8]. Neurological complications of influenza virus infections are relatively rare and affect mostly children [4]. The incidence is difficult to determine because there are different definitions, but it is estimated at 0.21 per million inhabitants per year [4]. The incidence of IAEs appears to have increased following the 2009 influenza A H1N1 pandemic, from an estimated 12 per million symptomatic H1N1 cases in 2009 [2,3,5]. In studies reporting >100 patients with infectious encephalitis, influenza virus was identified as a possible causative agent in 5–9% of cases [2,9]. In adulthood, all age groups are equally affected. Clinical syndromes of neurological diseases associated with influenza in adults are not always easy to diagnose. Based on the onset of influenza infection in relation to the onset of neurological symptoms, IAE is classified as acute, subacute, or late [2,3,5,7]. Patients with IAE are often prescribed antiviral drugs and corticosteroids, but their effects are unclear [10].
For the diagnosis of IAE, it is necessary to combine the findings of laboratory detection of the influenza virus or serological evidence of recent infection with the influenza virus, clinical picture with neurological symptoms along with brain imaging findings on MRI and intrathecal antibody formation. Approximately 60% of patients recover without sequelae. It seems urgent to promote influenza vaccination to prevent influenza and its severe complications. This work is aimed at refreshing the understanding of influenza after the dominance of COVID-19 during the previous three years.


