Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
K Karavdić1*, A Firdus1, N Džiho1 and A Brković2
Received: July 06, 2023; Published: July 18, 2023
*Corresponding author: K Karavdić, Clinic for Pediatric Surgery, Clinic Center of University Sarajevo, Bosnia, and Herzegovina
DOI: 10.26717/BJSTR.2023.51.008125
Introduction: Varicocele is the abnormal tortuosity and dilatation of the testicular vein within the
spermatic cord. The incidence of varicocele is approximately 16% in the normal adult population, 6%
in10-year-old boys,15% in13-year-old boys and about 30% in men in infertile couples. There are different
treatments for varicocele, as open surgery, microsurgery, laparoscopy, sclerotherapy, and other techniques.
We describe the effective use of the bipolar vessel-sealing device: Liga Sure for the division of the internal
spermatic vessels in a laparoscopic varicocelectomy.
Material and Methods: Between 2012 and 2022, 50 patients were treated because of varicocoele, 17
patients were treated minimal invasive surgery,9 patients using a metal clip and 8 by laparoscopic Palomo
varicocele ligation using Liga Sure vascular sealing. Patient ages ranged from 9 to 18 years (mean, 14.1
years). Indications for surgery included grade III varicocele, ipsilateral testicular hypotrophy, or complaints
such as pain or discomfort during physical activities. We placed a 5-mm umbilical port for access (open
Hadson procedure) and kept pneumoperitoneum below 12 mm Hg. Under laparoscopic guidance, two
additional ports of 5 mm were inserted in the lower right quadrant and supraumbilical, respectively.
Oncethe vessels were isolated, the vascular sealant was applied 3–4 times to ensure coagulation of the
spermatic vessels; the vessels were then divided with laparoscopic 5-mm scissors.
Results: Mean follow-up time was 18.8 ± 1.1 months. Open procedure had next complications: hydrocoele
5/33 (15,15%) and recurrence 3/33 (9.09%), laparascopy procedure (using methal clips) hydrocoele 1/9
(11,11%) and recurrence 1/9 (11,11%) and laparascopy procedure (using LigaSure device) did not have
complications hydrocoele 0/8 and recidive 0/8.
Conclusions: Laparoscopic Palomo varicocele sealing is a safe, effective, and simple method for correcting
varicoceles in young males. This method seems to take less time than clip application and open procedure.
The advantage of this procedure is also the possibility to correct the associated inguinal hernia or patent
processus vaginalis.
Keywords: Vericocole; Laparascopy; Ligasure
Varicocele is the abnormal tortuosity and dilatation of the testicular vein within the spermatic cord. The incidence of varicocele is approximately 16% in the normal adult population, 6% in10-year-old boys,15% in13-year-old boys and about 30% in men in infertile couples. [1] Testicular blood vessels come from the abdomen and pass through the inguinal canal as part of the funiculus. Ascending vein flow is ensured by small, one-way valves that prevent the return flow of venous blood. Disruption of the valvular system or vein compression to surrounding structures can cause dilatation of the testicular veins. The tortuosity and dilatation of the veins of the pampiniform plexus is the result of the incompetence of the valvular mechanism of the spermatic vein from the hydrostatic pressure of the venous blood transmitted from the large veins. The fact that over 90% of the varicocels are left-sided indicates the fact of venous drainage of the testicular veins, right in the v.cava inf. and the left in v.renalis. The presence of varicocele raises the temperature of the scrotum (temperature- sensitive test strip). Testicular biopsy in patients shows spermatogonia reduction, seminiferous tubule atrophy, endothelial cell proliferation, and Leydig cell abnormalities. Changes found in patients up to 18 years of age are potentially reversible, more extensive histological changes of change found in older men (reason for varicocel treatment during adolescence) - cell abnormalities [2]. The examination should be done in a lying and standing posture with and without the Valsalva maneuver. The size and volume of the testicle should be evaluated with Prader orchiometer or callipers and with Ultrasound evaluation. Absolute indications for surgery are presence of symptoms and decreased values in testicular size and volume. Correction of the varicocele improves the semen parameter in over half of the men. With the development of modern endoscopic surgery, the technique of laparoscopic varicocelectomy has progressively improved [3]. The Palomo technique, which involves high division of the testicular vein and artery, results in a significant lower recurrence rate than artery-sparing techniques [4]. The laparoscopic ligation of the vascular bundle varies based on whether the ligation is performed with absorbable or nonabsorbable suture, absorbable or nonabsorbable clips, or bipolar coagulation. The LigaSure™ (Valleylab, Boulder, CO, USA) sealing device uses an optimized combination of pressure and energy to create seals by melting the collagen and elastin in the vessel walls and reforming it into a permanent, plastic- like seal. It fuses vessels up to and including 7 mm in diameter and tissue bundles without dissection or isolation. Furthermore, when the instrument determines that the seal is complete, a tone sounds and output to the handpiece is automatically discontinued. Lateral thermal spread is minimal (1-2 mm) and the unique energy output results in no sticking or charring (Figure 1). Aaberg, et al. reported the Laparascopic Palomo procedure in 1991[5].
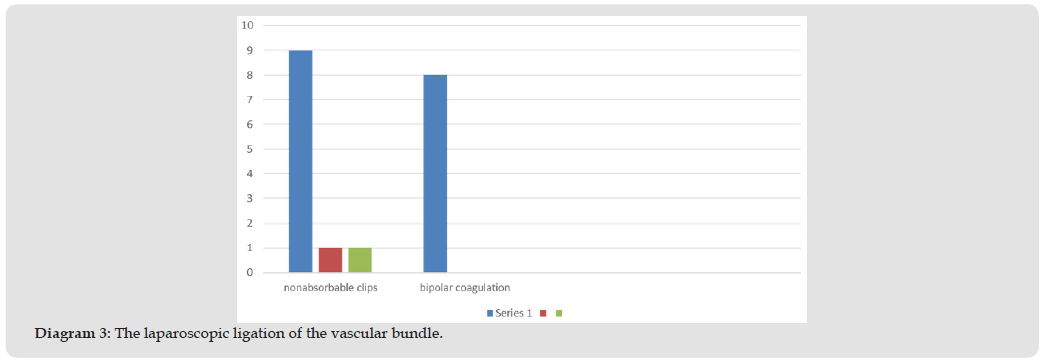
Between 2012 and 2022, 50 patients were treated because of varicocoele, 17 patients were treated by minimal invasive surgery, (9 patients using a metal clip and 8 by laparoscopic Palomo varicocele ligation using Liga Sure vascular sealing). Patient ages ranged from 9 to 18 years (mean, 14.1 years). Indications for surgery included grade III varicocele (Figure 2) or ipsilateral testicular hypotrophy. We placed a 5-mm umbilical port for access, and pneumoperitoneum was established at 12 mm Hg using Hadson open procedure for placement of first troacar. Under laparoscopic guidance, two additional ports of 5 mm were inserted in the lower right quadrant and supraumbilical, respectively, which allowed the insertion of a Liga Sure LS 1000 vessel sealing probe. The patient was then placed in the Trendelenburg position. Ectasia of the spermatic vessels was corrected with the Palomo technique. Once the vessels were isolated, the vascular sealant was applied 3–4 times to ensure coagulation of the spermatic vessels; the vessels were then divided with laparoscopic 5-mm scissors (Figures 3-7). Follow-up ranged from 6 to 24 months and included clinical, echocolor Doppler ultrasound assessment, and ultrasonographic orchimetry corrected with the Palomo technique. The procedure required a 5-mm grasping forceps, a pair of scissors, and the LS 1000, which also functions as a Maryland grasping forceps.
The following diagram represents the representation of minimally invasive procedures in the field of pediatric urology at our Clinic in the specified period. Varicoceles were operated on in 17 patients, orchdopexy in 23 patients and herniectomies in 19 patients. The following diagram represents patients operated on over a period of 10 years for varicocele in our Clinic. 33 (66%) patients were operated on by an open procedure and 17 (34%) patients by laparoscopic surgery. The following diagram represents patients who underwent minimally invasive surgery. 9 patients were operated using metal clips and 8 patients with the Ligasure technique. The following diagram represents the age structure of the operated patients. Patient ages ranged from 9 to 18 years (mean, 14.1 years). The most represented age was 13 years. Mean operative time was 18 minutes (range, 15–23 minutes) and was significantly shorter than in the laparoscopic clip ligation group. The following table represents the complications we verified through patient follow-up. No patient had testicular atrophy. Patients who were operated on with an open procedure had reactive hydrocele in 15.15% (puncture was performed in 3 cases and reactive hydrocele surgery in 2). Patients who were operated with a laparoscopic procedure using clip applicators had 11.1% recurrence and 11.1% hydrocele. Patients who were operated on using ligature did not have the mentioned complications (Diagrams 1-4) (Table 1).
Diagram 3
The LigaSure device has been demonstrated to be safe. The first published studies illustrating the safety of the LigaSure device was in 2002 in a laparoscopic splenectomy [6]. The study demonstrated the increased safety of the operation when compared to those done using conventional knot tying techniques. Developments in surgical instruments have advanced dramatically during recent years. Various instruments such as vessel sealing systems Liga Sure, the ultrasonically activated scalpel, and the Hemoclip are used in many surgical manipulations such as hemostatic cuts [7]. Liga Sure has the following advantages: it can be used in deep locations with safety and ease; it does not require vessels to be exteriorized during sealing; it is convenient to use when it is difficult to make a space between 2 vessels; and it is easy to use [8]. The Liga Sure vessel sealing device utilizes both electrical energy and pressure to liquefy and reform the collagen and elastin in vessel walls and tissue up to 7 mm in diameter to provide hemostasis [9]. The device has incorporated a feedback control that automatically stops further energy transmission once a seal has been achieved [10]. There is also an advantage that clips can be left in the body in these methods. Palomo varicocelectomy is a popular method, which involves ligation of the internal spermatic veins together with the testicular artery [11]. This method results in a significant decrease in the operative failure rate compared with the artery-sparing procedures, with no increase in the incidence of testicular atrophy more cases of hydrocele testis after surgery were seen in Liga Sure surgery, but this may be due to involvement of causes not directly associated with the surgery, such as lymph flow in the underdeveloped scrotum [12]. Hydrocele formation is the second most common complication after varicocelectomy and has been reported to have a rate of up to 39% [13]. The testicular lymphatic system consists of 2 plexuses, the deep plexus that drains the substance of the testis and epididymis and the superficial plexus that commence beneath and drains the tunica vaginalis. These lymphatic trunks ascend to collect in the spermatic cord accompanying the testicular vessels to end in lateral aortic lymph nodes. Postoperative hydrocele occurs in a minority of cases in which the testicular lymphatics are ligated by means of Palomo procedure. In our series of patients with varicocele, performing the Palomo procedure using the open method, we had hydrocoele formation in 5 patients 5/33 (15.15%), with the laparoscopic procedure using metal clips only in 1 patient 1/9 (11.11%), while in 8 patients in whom we used laparoscopic liga sure did not have a single hydrocoele formation. Recurrence is the most common complication after varicocelectomy. Persistent or missed small collateral veins at the time of ligation are the main cause of recurrence after varicocelectomy. In our series of patients with varicocele, by performing the Palomo procedure using the open method, we had recurrence formation in 3 patients 3/33 (9.09%), with the laparascopic procedure using a metal clip only in 1 patient 1/9 (11.11%), while in 8 in patients in whom we used laparoscopic liga sure, we did not have a single recurrence formation. In our approach, we cut the vascular bundle, although other groups seal without cutting the bundle [14]. Some hypothesize that ligating but not dividing the internal spermatic vessels may significantly decrease the rate of postoperative hydrocele [15]. The LS 1000 probe works very well as a dissector forceps and does not need to be replaced during the subsequent sealing, which facilitates and shortens the procedure. Moreover, Liga Sure offers the advantage of very low thermal damage to contiguous tissues and only mild smoke production. The operative time is significantly reduced compared to the method using clips, which was done before the development of this kind of device. In the other experiment to examine the effect of vessel sealing, it was confirmed that the Liga Sure has performance comparable to the clips.
Laparoscopic Palomo varicocele sealing is a safe, effective, and simple method for correcting varicoceles in young males. This method takes less time than clip application and open procedure. The advantage of this procedure is also the possibility to correct the associated inguinal hernia or patent processes vaginalis.


