Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Rodríguez Gómez Carmen María* and Saumench Perramon Roser
Received: May 29, 2023; Published: June 06, 2023
*Corresponding author: Carmen M Rodríguez Gómez, Department of Thoracic Surgery, Hospital Universitario Dr. J Trueta de Girona, Avenida França, s.n, CP: 17007 Girona, Spain
DOI: 10.26717/BJSTR.2023.50.008018
Background: Intrathymic bronchogenic cysts are extremely rare anterior mediastinal tumors in adults. Complete resection is mandatory. The routine surgical procedure has traditionally been removal of the lesion by thoracotomy approach.
Case Presentation: We present a 69-year-old male patient who was found to have an incidental thymic mass on the computer tomography scan of the chest. Non-invasive thymoma was suspected and a subxiphoid thoracoscopic thymectomy was performed. Histopathological examination revealed a unilocular intrathymic bronchogenic cyst.
Conclusions: Intrathymic bronchogenic cysts are uncommon. A complete excision can be performed by subxiphoid thoracoscopic approach providing the final diagnosis and offering clear postoperative advantages. Thoracoscopic excision should be considered the primary therapeutic option and furthermore, the subxiphoid thoracoscopic approach can be safely performed and has not been published before elsewhere.
Keywords: Intrathymic Brochogenic Cysts; Subxiphoid Thoracoscopic Thymectomy; Anterior Mediastinum
Abbreviations: IBC: Intrathymic Bronchogenic Cyst; CT Scan: Computer Tomography Scan; PET/CT: Positron Emission Tomography with Computer Tomography
Bronchogenic cysts are rare congenital anomalies that develop due to a foregut abnormal budding located in the mediastinum or in the lung parenchyma. In the mediastinum they are usually located in the middle or posterior mediastinum and anterior location is uncommon. Thymic cysts are relatively rare pathologies representing 1-3% of mediastinal masses. They can contain proteinaceous or hemorrhagic material which shows soft tissue attenuation on CT and creates a diagnostic dilemma. Intrathymic bronchogenic cysts (IBC) are extremely rare. Unilocular IBC is a rare entity in adults’ patients, but they should be considered in the differential diagnosis of anterior masses of the mediastinum.
A 69-year-old male patient with a previous history of heavy smoker, chronic obstructive pulmonary disease, rheumatoid arthritis in the childhood and peptic ulcer, was referred to our department because of an incidental mediastinal mass detected on chest X-ray. He had no clinical symptoms, and his physical examination and laboratory test results were normal. The computer tomography scan (CT) showed an 18 x 22 mm well-defined oval shaped enhancing soft tissue anterior mediastinal tumor (Figure 1A). A positron emission tomography with computer tomography (PT/CT) was performed and did not show any hypermetabolic activity (Figure 1B). Based on the high index of suspicion of non-invasive thymoma a subxiphoid thoracoscopic thymectomy was performed. Under general anesthesia and single lung ventilation the patient was placed in decubitus supine position. A subxiphoid thoracoscopic port was used with insufflation of pleural space with CO2 (flow of 6 l/m, pressure of 3-5 mmHg). Completely excised thymus and adjacent mediastinal fat was carried out. The postoperative course was uneventful, and the patient was discharged home 48 hours after the procedure. Macroscopically, our case was unilocular thymic cyst that contained yellowish fluid and histopathological examination confirmed a 1.5 cm diameter cyst lined exclusively by ciliated epithelium that confirmed the diagnosis of IBC.
Figure 1 Multi-slice CT and PET/CT showing the IBC. CT is used to delineate the IBC shape, size, location, attenuation and relation to the adjacent structures (A). IBC has no fludeoxyglucose (FDG) uptake on the PET/CT (B).
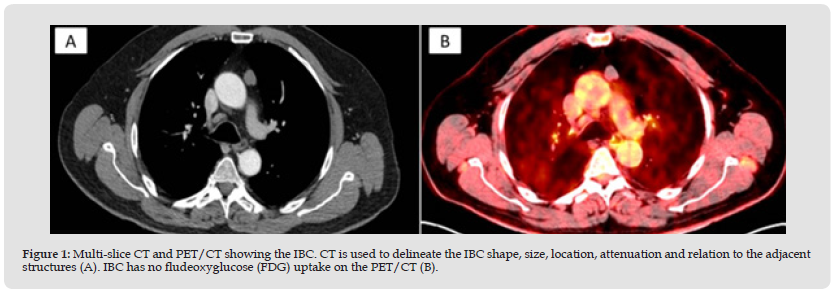
There are few studies focused on the benign thymic pathologies such as hyperplasia or thymic cysts. The most common mediastinal cysts are bronchogenic cysts, which usually occur in the posterior and middle mediastinum [1], and they are related to the tracheobronchial tree near the tracheal carina. Rarely bronchogenic cysts can occur within the thymus gland. The first reported case was published in 1997 by Taniwaki [2]. It is also known that multinodular IBC lesions are more common in adults while unilocular IBC lesions are more common in the pediatric age group [3]. These cysts are asymptomatic and discovered incidentally in imaging studies done for another reason. Multi- slice CT is used to delineate IBC shape, size, location, attenuation and relation to the adjacent structures. Soft- tissue attenuation caused by protein-rich cyst fluid can make the diagnostic preoperative very difficult and it has been reported in only 45% of the cases [4]. IBC has no fludeoxyglucose uptake on the PET/CT. The most important point for preventing recurrence of the cyst is the complete resection. Routine surgical procedure has traditionally been complete cyst removal by thoracotomy however minimally invasive surgery has enabled a less traumatic approach in the treatment of mediastinal lesions.
Mouroux reported the removal of a posterior mediastinal bronchogenic cyst by video-assisted thoracoscopy with three trocars through small incisions [5]. In our knowledge the subxiphoid approach has never been used before. The main advantage of this approach is less trauma (just one incision) and discomfort for the patient. The lack of intercostal muscle incision and no risk of rib fracture reduce the postoperative pain and length of hospital stay. A subxiphoid incision with the retractor and a hermetic three port Gelpoint Mini® (less than 3 cm) was placed which allowed insufflation of pleural space with CO2. The final diagnosis IBC is usually made after complete excision and histopathological examination. Macroscopically, unilocular thymic cysts that contained fluid. Histologically unilocular thymic cysts lined by a pseudostratified ciliated epithelium with adjacent thymic tissue in the form of lymphocytic component. Unilocular thymic cyst with the caveat of the cysts being exclusively lined by ciliated epithelium (Figures 2 & 3).
Figure 2 The image showing the surgery field: Subxiphoid incision with the retractor and a hermetic three port Gelpoint Mini® was placed which allowed insufflation of pleural space with CO
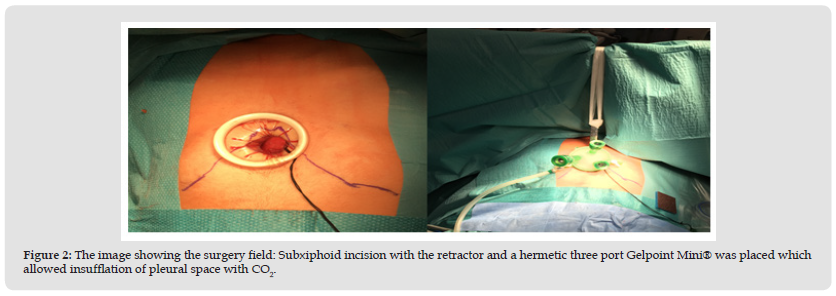
Figure 3 Microscopic image: Unilocular well circumscribed and thin walled intrathymic cyst and cyst lined by respiratory type epithelium (ciliated pseudostratified columnar cells) (A, B). Macroscopic image: well delimitated lipomatous thymic lesion with an adyacent cystic lesion (C).
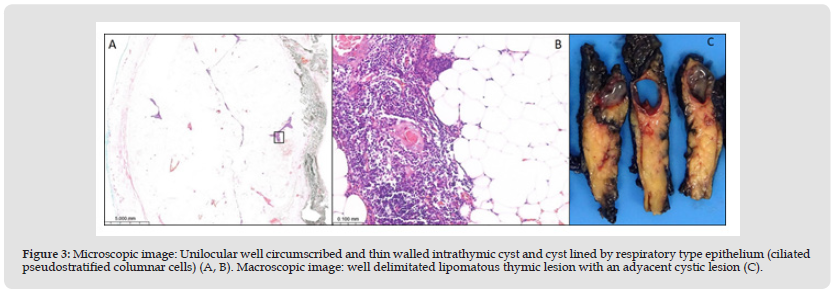
Unilocular intrathymic bronchogenic cysts occurring in adult patients are unusual in the thymus gland. The complete excision is the gold standard and can be performed by subxiphoid thoracoscopic approach. The final diagnosis is given after surgical complete excision of the cyst and histopathological examination.
Not applicable.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor - in - Chief of this journal.
Not applicable.
I declare that the work is original and has not been previously published or is in the process of being reviewed by any other journal. In the same way, written informed consent has been obtained for the authorization of its publication, reproduction and dissemination in the scientific community. The patient has given informed consent to have this case published.
Not applicable.
All the authors have contributed intellectually to the work, meeting the authorship conditions, have approved the final version of the work and assigned the publication rights.
Not applicable.


