Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Monica Zuluaga Quintero1* and Adriana Margarita Maria Trejos Tenorio2
Received: May 26, 2023; Published: June 05, 2023
*Corresponding author: Mónica Zuluaga Quintero, Internist, Epidemiologist Hospital Pablo Tobón Uribe Medellín, Colombia
DOI: 10.26717/BJSTR.2023.50.008017
Introduction: A myocardial bridge is a congenital abnormality in which a epicardial coronary artery segment is intramyocardial, it decreases the diameter of the vessel in systole and less coronary flow in diastole, producing in some cases angina and is confused with acute ischemia.
Objective: to describe the presence of a myocardial bridge as a differential diagnosis of acute chest pain.
Clinical Case: patient admitted for acute coronary syndrome without ST elevation, in whom angiography demonstrated intramyocardial bypass without evidence of obstructive coronary lesions.
Results: medical management with beta-blocker was defined, patient had excellent clinical evolution after two years of follow-up and he did not have recurrence of angina.
Conclusions: An intramyocardial bridge is an infrequent cause of acute chest pain that can be confused with acute ischemia and its treatment varies according to risk factors, symptoms, comorbidity, and atherosclerotic coronary obstruction.
Keywords: Chest Pain; Angina Unstable; Myocardial Bridging
A myocardial bridge is a congenital abnormality in which a segment of the epicardial coronary artery is intramyocardial, which causes a decrease in the diameter of the vessel in systole and less coronary flow in diastole, producing in some cases angina and is confused with acute ischemia. The prevalence is variable and depends on the diagnostic method, in autopsies described in a range of 5 to 86%, but it is now rare in coronary angiography to 4.9% of study [1]. Its relationship with structural abnormality, ischemia or myocardial infarction, major cardiovascular outcomes, and mortality is controversial and therefore treatment must be individualized.
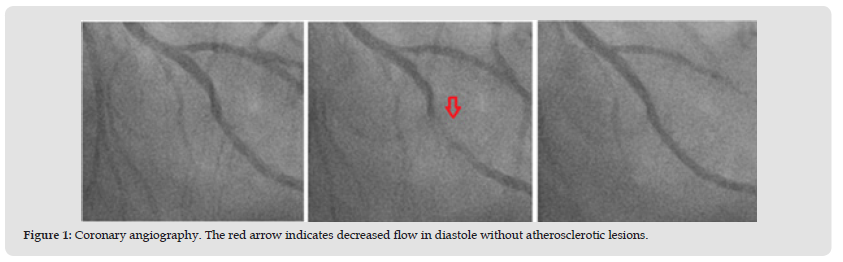
We present the case of an 82-year-old man, hypertensive, with ex-smokers, a family history of coronary artery disease and stable angina of 4 months evolution without previous stratification. He was admitted to the emergency room due to a change in the characteristics of the pain being of greater intensity and at rest. Blood pressure of 213/88 mmHg, heart rate 62 beats per minute, cries in the lung bases and grade II edema in the extremities. Electrocardiogram (EKG) was performed with evidence of left bundle branch block present in previous studies and left ventricular hypertrophy. In serial EKG, dynamic changes of the ST were observed, and ultrasensitive troponin was performed, which was negative. It was classified as intermediatehigh risk unstable angina, GRACE 136 points. The echocardiogram found signs of hypertensive heart disease, asynchronous movement of the interventricular septum, without alterations in contractility with an ejection fraction of 60%. Coronary angiography documented an intramyocardial bridge in the middle third of the anterior descending artery with reduction of the lumen of up to 80% in systole, but healthy coronaries (Figure 1). Given the absence of coronary obstruction, medical management, antihypertensive medication adjustment and clinical follow-up were defined, without recurrence at the date of pain.
Figure 1 Coronary angiography. The red arrow indicates decreased flow in diastole without atherosclerotic lesions.
A myocardial bridge is a congenital abnormality in which a segment of the epicardial coronary artery is intramyocardial, mainly affecting the middle portion of the anterior descending artery and less frequently other branches, with a variable incidence of 15% to 85% [1,2]. During systole, there is a decrease in the diameter of the vessel and less flow in diastole, producing microvascular dysfunction, endothelial trauma, platelet activation and vasospasm with the formation of atherosclerotic plaques; 80% of patients are asymptomatic, but occasionally produces angina that mingles with acute ischemia and in these cases, 50% present with coronary disease [3]. Generally, the diagnosis is made during angiography in which the constriction of the vessel is observed in systole and a lower diastolic flow is known as the milking phenomenon, although most cases have been described in autopsies [1,3]. There is controversy as to whether in the absence of coronary obstruction, it should be considered a benign condition or if it can cause acute myocardial infarction, arrhythmias and sudden death, and therefore define the need for intervention. The probability of ischemia depends on the size of the bridge at greater length and thickness, the dominance of the coronary circulation, the presence of ventricular hypertrophy and a lifestyle that increases cardiovascular risk [2,3]. It is proposed to evaluate the hemodynamic impact with stress echocardiography, myocardial perfusion imaging and measurement of fractional flow reserve to define the therapy to be followed, although validation studies in this regard are still lacking. Therefore, the recommendation of the treatment of these patients depends on the symptoms and concomitant conditions such as: atherosclerotic coronary disease, hypertrophic heart disease or stress heart disease.
Beta-blockers are the first line since they reduce tachycardia and greater contractility involved in the reduction of diastole time and allow control of angina in 89% of cases, being an alternative nondihydropyridine calcium antagonist and as a second line ivabradine [1,3,4]. When symptoms persist despite medical management and there is systolic compression greater than 60% of the vessel diameter, interventionism with percutaneous revascularization or surgery is considered if there is proximal coronary obstruction. Nevertheless, the first is debated, since higher rates of restenosis, thrombosis, and stent fracture have been described, although there are no data regarding the new generation; but it is the choice in situations that contraindicate the second. And if the compromise is limited to a single vessel, a myotomy [2,4,5] can be considered. Echeverry, et al. [3] They report a series of 11 patients with myocardial bridges and non-ST AMI. Most underwent medical management, only in three cases angioplasty and stent implantation given that they had associated coronary obstructive lesions: presenting symptom control and excellent clinical evolution [3]. In our patient there was no increase in cardiac biomarker, nor evidence of atherosclerotic obstruction, so possibly the angina was caused by the presence of the myocardial bridge added to poor blood pressure control, with optimal antihypertensive and antiaginous treatment has had excellent evolution.
An intramyocardial bridge is a benign condition with a good prognosis, in most cases it is asymptomatic, or the angina resolves with medical management, and few require revascularization therapy or intervention with myotomy. More studies are required to determine the best diagnostic and treatment strategy for these patients.
No funding received.
The authors declare that they have no conflicts of interest.


