Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Xi Deng and Xuemei Lin*
Received: March 21, 2023; Published: May 23, 2023
*Corresponding author: Xuemei Lin, Department of Anesthesiology, West China Second University Hospital, Sichuan University, No. 20, Section 3, South of Renmin Road, Chengdu 610041, Sichuan, People’s Republic of China
DOI: 10.26717/BJSTR.2023.50.007971
Dwarfism is a genetically related disorder and characterized by short stature. Pregnancy in women with dwarfism is uncommon. Here, we present a case of a 24-year-old pregnant woman who underwent the double-space technique in epidural anesthesia for an elective cesarean delivery. She was preoperatively diagnosed with dwarfism, scoliosis, C2-T10 syringomyelia, severely impaired lung function and multimalformations. After a multidisciplinary discussion, cesarean section was performed at 35 weeks of gestation. She received T12-L1, L2-L3 epidural anesthesia and epidural catheters were inserted upward and downward, respectively. In a word, we successfully performed cesarean section on the puerpera and discussed the risks and challenges of anesthesia presented by this kind of patients.
Keywords: Obstetric Anesthesia; Dwarfism; Cesarean Section
Abbreviations: ECG: Electrocardiograph; BP: Blood Pressure; HR: Heart Rate; NBP: Non-Invasive Blood Pressure; ICU: Intensive Care Unit
Dwarfism, defined as a failure to attain a height of 145cm in male or 135cm in female, is caused by a genetic disease [1]. The most common type of dwarfism is achondroplasia occurring in 0.5-1.5 per 10 000 live birth [2], accounting for approximately 70% of cases of dwarfism [3]. Pregnancies among women with dwarfism are rare and fertility rates are often low [4]. The clinical manifestations of these patients are short trunk and limbs, craniofacial and spinal anomalies. Due to small and deformed pelvis, parturients with dwarfism usually require delivery by cesarean section. However, scoliosis, impaired respiratory function, short neck and limited extension significantly increase risks of anesthesia administration and management. Here, we report a successful case of anesthesia management of a parturient with dwarfism.
24-year-old primipara with dwarfism at 32 weeks of gestation was admitted to our hospital on account of high risk pregnancy. She was 97cm tall and weighed 25kg. As shown in (Figures 1a & 1b). Her typical signs were severe scoliosis, shortening of both legs and inability to stand. A MRI scan of her spine showed obvious s-shaped scoliosis and C2-T10 syringomyelia. In addition, her trachea was running along the right front of spine, her thorax was asymmetrical, and her lung function was severely impaired. In the operation room, two veins of the patient were opened up. Standard monitors were applied, including Electrocardiograph (ECG), pulse oximetry (SPO2) and Non-Invasive Blood Pressure (NBP). Her baseline Blood Pressure (BP), Heart Rate (HR) and SPO2 were 116/69 mmHg, 108 times/min and 94%, respectively. We planned to administer the double-space technique in epidural anesthesia with a backup plan of general anesthesia, including the management of difficult airways.
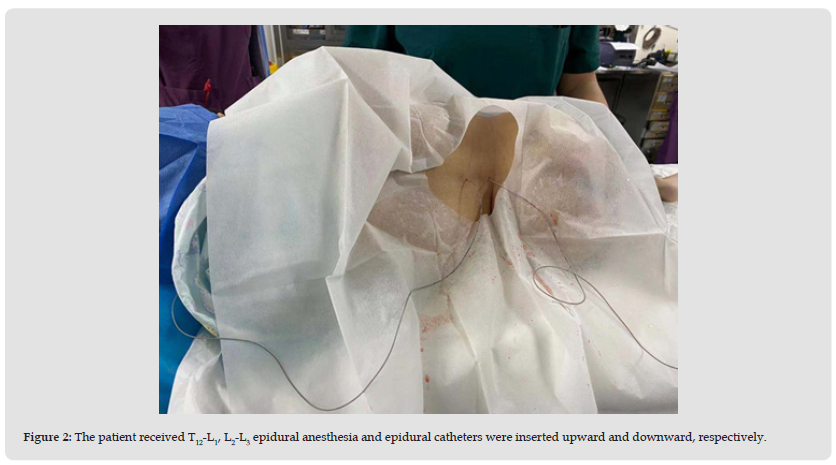
Assisting the patient in the left lateral position, we roughly located the T12-L1, L2-L3 intervertebral space under the guidance of ultrasound. The T12-L1 epidural catheter was placed cephalically while the L2-L3 epidural catheter was inserted caudally. As shown in (Figure 2). Then, 3ml of 2% lidocaine was given through the T12-L1 epidural catheter and 2ml of 1% lidocaine was administrated via the L2-L3 epidural catheter. 5 minutes later, the block height reached T8 bilaterally. 5ml of 3% chloroprocaine and 2ml of 1% lidocaine were further administrated the T12-L1 epidural catheter and the L2-L3 epidural catheter, respectively. At this stage, the block level reached to T4 and surgery was started. 3 minutes later, the fetus was delivered with Apgar scores of 10 at 1 minute and 5 minutes. After the operation, the patient was transferred to Intensive Care Unit (ICU) for further treatment. No complications or sequelae were observed. The next day, the patient returned to the general ward and discharged safely on the sixth day after surgery.
Figure 1 a) The patient was viewed from the back of the sitting position. b) The patient was seen from the back of the left lateral position.
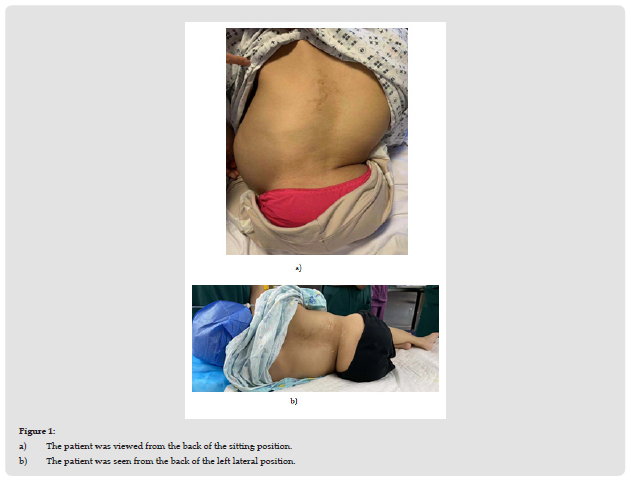
Figure 2 The patient received T12-L1, L2-L3 epidural anesthesia and epidural catheters were inserted upward and downward, respectively.
Pregnant women with dwarfism is rarely reported. The anesthetic management for such patients underwent cesarean section presents enormous challenges, including the pathophysiological diversifications of various forms of dwarfism, lack of bony landmarks, spine malformation and no standard guidelines for anesthetic management [5]. In previous reports, the anesthesia for such patients underwent cesarean delivery was performed partly under intravertebral anesthesia [5-7], partly under general anesthesia [3,8,9]. In our case, we chose intravertebral anesthesia: the doublespace technique in epidural anesthesia. General anesthesia for these patients is confronted with challenges. First, as a result of scoliosis and narrow chest cavity, lung function was severely damaged, like the patient in this case. A significant decrease in functional residual capacity and an increment in closing volume secondary to restrictive lung disease may cause atelectasis and ventilation/perfusion problems in pregnant women with dwarfism [6]. In addition, the patient is more likely to have a difficult airway due to a short neck, limited extension and displaced trachea. Futhermore, the patient was diagnosed syringomyelia and it has been reported that some of the patients had complications regarding general anesthesia including transient worsening of neurological symptoms postpartum, and prolonged muscle paralysis after atracurium [10]. Intravertebral anesthesia seems like a better choice for this patient. However, some special attention required to be paid. First, the specific termination plane of the spinal cord is not clear as a lack of MRI report. So, spinal anesthesia may injure the spinal cord. In addition, such patients are often association with spinal distortion and intravertebral canal stenosis, which makes the diffusion of the drugs in the subarachnoid space difficult to control, leading to a high spinal blockade, hypotension and even total spinal anesthesia.
Routine epidural anesthesia seems to be safer for these patients. And local anesthetics, without direct injection of cerebrospinal fluid, maybe beneficial for the patient with syringomyelia and there will be no large fluctuation of blood pressure in comparison with spinal anesthesia. However, epidural anesthesia is prone to block incomplete, unable to meet the needs of surgery. We choose the double-space technique in epidural anesthesia. Such patients often have limited growth and development, lower height and weight than the normal. There is no relevant guideline to recommend the type and dosage of anesthetics for intravertebral anesthesia. Therefore, on account of uncertain epidural volume, unpredictable diffusion of local anesthetics in the epidural space and severe scoliosis, we need personalized, small and repeated dose of medications via epidural catheters as well as continuous testing of the block level. There is no doubt that the difficult of anesthetic operation is considerable. An experienced anesthesiologist, assisted by ultrasound, successfully perforated the epidural space and placed tubes. In conclusion, pregnant women with dwarfism demand for a team approach in the perioperative period with comprehensive physical evaluation as it involves. If there are no contraindications, intravertebral anesthesia should be preferred for cesarean section in parturients with dwarfism.
The authors declare no conflicts of interest.
Authors state that the patient and her family have given their written informed consent to publish her case.


