Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Silvia Rota1,2#*, Ornella Spagnolello1,3,4#, Lucia Batzu2, Oliviero Francesco Valoti1, Gina Portella4 and Martin Langer4
Received: May 08, 2023; Published: May 23, 2023
*Corresponding author: Silvia Rota, MD Consultant in Neurology, Maurice Wohl Clinical Neuroscience Institute, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London,125 Coldharbour Lane, Brixton, SE5 9NU, London, United Kingdom
DOI: 10.26717/BJSTR.2023.50.007970
Introduction: To investigate safety self-perception and compliance to infection prevention and control
(IPC) measures of health care workers (HCWs) employed at the Bergamo field hospital (BFH) (Italy) during
the first Sars-CoV2 outbreak.
Materials and Methods: We delivered an online survey. Three scores were created: Risk Perception Score
(RPS), Compliance Score (CS), and Safety Score (SS).
Results: A total of 132 (88.7%) HCWs took part in the survey. Overall, RPS was intermediate [median 8
(Interquartile Range 7-11)], while CS was high [6 (5-7)], especially in less experienced HCWs ([CS 7 (5-7)]
vs [CS 6 (5-6.2)], p=0.022) and “non-clinical HCWs” ([CS 7 (7-8)] vs [CS 6 (5-7)], p<0.001). SS was high
[26 (23-29)], particularly in HCWs more used to personal protective equipment ([SS 27 (24-30)] vs [SS
25 (22-29)], p=0.038). Safety pathways and the IPC measures were clear for 98.4% of participants. Those
who needed less than 3 shifts to become confident with IPC measures scored higher in the SS item “did you
feel calm and without any anxiety while working inside the BFH?” [3 (2-4) vs 3 (2-3), p=0.004] and those
who found the safety procedures in place at BFH “a lot clear”, had a higher SS [27 (23-29) vs 23 (17-28.25),
p=0.029] and scored higher in the aforementioned SS anxiety-related item [3 (2-4) vs 2 (2-3), p=0.002].
Conclusion: Getting more experienced with IPC measures may reduce compliance. Clarity in pathways,
space organizations, and protocols improves safety self-perception. Staff training and IPC supervision are
fundamental to increasing HCWs’ safety perception.
Keywords: COVID-19; Infection Prevention and Control Measures; Safety Self-Perception; Health Care Workers; Field Hospital; Survey
Abbreviations: IPC: Infection Prevention and Control; HCW: Healthcare Workers; BFH: Bergamo Field Hospital; RPS: Risk Perception Score; CS: Compliance Score; SS: Safety Score; PPE: Personal Protective Equipment
The COVID-19 pandemic has put a strain on healthcare systems across the world, with a dramatic impact on frontline healthcare workers’ (HCWs) physical and mental health, with increased incidence of depression, post- traumatic stress disorder, sleep issues, and anxiety [1,2]. Besides the stress associated with the risk of getting infected by SARS-CoV-2 and the long working hours spent to care a high number of critically ill patients, additional stress load has derived from the difficulty in accessing appropriate Personal Protective Equipment (PPE), the fear of wearing it incorrectly, the awareness of being a risk for their loved ones and the occurrence of taking care of their own colleagues [3-5]. In this scenario, HCWs might become reluctant to work and develop moral injury, a psychological distress that may contribute to developing mental health illness [6-8]. With the first wave of the pandemic spreading out in Bergamo (Northern Italy) local hospitals were heavily overstretched by the unprecedented demand of patients requiring admission simultaneously [9,10]. As result of poor infection prevention and control (IPC) measures adopted to face the outbreak in the first instance, many HCWs in Bergamo were infected by SARS-CoV-2. According to regional data, 24.1% of the total positive swabs performed in Bergamo on the 15th of May 2020 referred to HCWs (https://www.lombardianotizie.online accessed on the 15th of May 2020). Moreover, several HCWs’ deaths due to COVID-19 were reported in the province since the beginning of the epidemic, especially among physicians (mostly general practitioner doctors) [9].
In order to meet the high demand for health assistance and limit in-hospital infection, an only-COVID-19 field hospital was set up in the Bergamo fair building at the end of March 2020. A detailed description of the hospital has been published [11]. The BFH was an ancillary facility of Papa Giovanni XXIII Hospital, a referral hospital throughout the province of Bergamo. It offered 142 additional beds, half of which were intensive care ones. Its first period of activity, the one to which this survey refers, was from the 6th of April to the 23rd of May 2020. In this hospital, HCWs with different backgrounds operated to provide a high standard of care to patients affected by COVID-19. Moreover, a group of volunteer-trained IPC officers, with no previous clinical background, secured the correct use of the PPE by the workers closely in contact with the patients, especially while entering or exiting the red zone. Despite the dramatic and confusing scenario of the first hit of the pandemic in one of the hardest hit cities by COVID-19, one of the main goals of the Bergamo Field Hospital (BFH) was to deliver to HCWs a safe workplace to confront the outbreak minimizing the stress load related to the ineluctable fear of getting infected. The main aims of this survey were to investigate the safety self-perception of HCWs employed at the BFH during the first hit of the COVID-19 pandemic and to explore their compliance with IPC measures while performing their working activities.
Study Design
This was a cross-sectional study, consisting of the administration of an online survey. An anonymized questionnaire was distributed through text message or email to staff members at the end of their duty at the BFH. It consisted of 17 multiple choice questions grouped into 6 sections: background, COVID-19 risk perception, social habits during the working period at the BFH, working activities inside the BFH, compliance, and efficacy. In order to increase the survey participation rate, only some questions were compulsory.
Study Setting and Study Population
A broad contingent of HCWs, with different backgrounds, staffed the BFH. Overall, 150 HCWs aged from 26 to 68 years took part in this project. Among them: different professionals from Papa Giovanni XXIII Hospital, three contingents of nurses of the Italian Civil Protection, a medical and technical team from the humanitarian nongovernmental organization EMERGENCY, volunteer physiotherapists, and IPC officers. A Russian team, composed of doctors, nurses, and interpreters, served at BFH for several weeks too. The questionnaire was administered to Italian speakers only.
Ethical
Electronic informed consent was shown on the initial page of the survey. Participants were not asked to clarify demographic data, such as sex and age, in order to keep the results anonymized. Participants were enrolled on a voluntary basis and were not economically rewarded.
Data Analysis
Descriptive statistics have been used to report questionnaire results’ proportions and frequencies. The answer to a question was included in the analysis when at least 80% of the interviewees replied to it. When the answer required a degree of qualitative variables, a relative number from 0 (=very little) to 4 (=very much) was assigned for the analysis. Three scores were created, the Risk Perception Score (RPS, range 0-16, made by 4 items), the Compliance Score (CS, range 0-8, made by 8 items), and the Safety Score (SS, range 0-36, made by 9 items).The RPS (range 0-16) was made by 4 sub-scores (range 0-4): risk related to the COVID-19 pandemic for the self, family, community, and humankind. The higher the risk related to the COVID-19 pandemic was perceived the higher the score was. The CS (range 0-8) was created based on the recommended behaviors adopted inside the BFH. If a specific recommended behavior was followed, a point was added to the score. The SS (range 0-36) assessed the perception of safety inside the BFH. Each question was marked from 0 to 4, according to the degree of safety perception, with the higher score assigned to the answer corresponding to the perceived safest one.
For the scores’ calculation, only participants who answered all the scores’ items were considered. For the scores’ evaluation, an arbitrary division in thirds has been applied: the RPS was considered low for score range from 0 to 5 (COVID-19 considered not dangerous), average from 6 to 11, and high from 12 to 16 (COVID-19 considered really dangerous); the CS was considered low for score range from 0 to 2 (poor compliance), average from 3 to 5, and high from 6 to 8 (high compliance); the SS was considered low from score range from 0 to 12 (low level of safety perception), average from 13 to 24, and high from 25 to 36 (high level of safety perception). Correlations between ordinal variables were assessed using Spearman’s Rank-Order Correlation and differences between groups, chosen from 4 of the 6 sections (background, social habits during the working period at the BFH, working activities inside the BFH, efficacy) were investigated using Mann-Whitney or Kruskall-Wallis tests as appropriate. COVID-19 risk-perception and compliance sections were not considered in the differences between group analyses as they only included the RPS and the CS. To test whether the three scores or specific SS’s sub-scores, chosen according to their consistency with the analysis performed, were different between specific groups, only subjects who replied to both items were included. A p-value of less than 0.05 was considered statistically significant. SPSS Statistics 25.0 (IBM Corp., Armonk, NY, USA) was used for the analyses.
Work Background
A total of 132 (88.7%) HCWs employed at BFH replied to the survey. The main characteristics of the population are shown in Table 1. Of them, the majority were nurses (40.2%), followed by IPC officers (18.9%) and medical doctors (12.1%). 73.5% (97/132) of the participants were “clinical HCWs” (professionals directly in contact with patients, such as nurses, doctors, and physiotherapists), while 26.5% (35/132) of the interviewed were “non-clinical HCWs” (which includes the professionals not at direct contact with patients, mainly but not only volunteer ICP officers). 66.7% of staff members had no previous experience with COVID-19 patients and 55.3% did not have any experience at all with highly infectious patients, whose assistance requires the use of PPE. 48.8% of those who had previous experience with COVID-19 patients did not feel safe in their previous job.
Note: aThis number refers to the number of people who replied “yes” to the question: Did you have previous experience with COVID-19 patients?.
COVID-19 Risk-Perception
For the RPS the median was 8 [interquartile range (IQR) 7-11] [minimum-maximum 0-16]. COVID-19 epidemic was considered dangerous in any sub-scores: the median was 2 (1-2) for them-self, 2 (2-3) for the family, the community, and humankind (Table 2).
Note: aScore results were expressed in median (IQR 25-75).
bin order to make the scoring system easier to understand some of the score questions have been rephrased.
Social Habits During the Working Period at the BFH
56.1% of HCWs were sharing accommodation during their stay in Bergamo, while the remaining were living in a private house (shared or not with the household). 61.4% had extra-hospital contacts with other HCWs and 58.3% had contacts with non-HCWs outside working hours (data were partially collected during the lockdown) (Table 1).
Working Activities Inside the BFH
Most of surveyed BFH staff members worked for a period of 0-30 days (44.7%) or 0-45 days (43.9%), while the remaining (11.4%) for 0-15 days. The most frequent shift was 6-9 hours a day (84.1%). 65.9% changed their PPE once each working shift, 28% twice, three times or more the remaining 6.1%. Access to the red zone for at least one emergency happened in 27.3% of the cases (Table 1).
Compliance
The median of the CS was 6 (IQR 5-7) [minimum-maximum 0-8]. 69.7% of HCWs reported having a shower inside the BFH at the end of the shift. Inside the red zone, 44.7% of HCWs never lifted or removed their shield, 65.2% never touched their mask, goggle, or glasses, 74.2% never put their hands behind the protective gowns, 57.6% never used their phone, and if so, 78% cleaned it once outside the red zone. 89.4% always changed or cleaned their gloves after touching a patient or a contaminated surface and 81.8% used to correct the others when spotting inappropriate or unsafe behavior (Table 2).
Efficacy
59.1% of the HCWs employed at BFH became confident with the PPE donning and doffing process in less than 3 shifts, 30.3% in 3-6 shifts, 6.9% required more than 6 shifts, while 1.5% were still not confident with the process at the time of administration of the survey. Safety pathways and the IPC measures in place at the BFH were enough (13.6%) or a lot (84.8%) clear for the participants who answered the question (Table 1). The SS median was 26 (IQR 23-29) [minimummaximum 0-36]. Overall, the self-risk of contracting the disease was perceived as low [3 (3-4)] and the BFH structure was considered safe to contain COVID-19 spreading [3 (3- 4)], despite reduced confidence in performing maneuvers on patients while wearing PPE [2 (2-3)] and meeting other people outside the hospital because of possible contagiousness [2 (1-3)]. However, HCWs declared a low level of anxiety both during working hours [3 (2-4)] and outside the working hours [3 (2-4)], and the quality of sleep was considered satisfactory [3 (2-4)]. Moreover, the feeling of being completely healthy without complaining of any stress-related COVID-19 symptoms was high [4 (3-4)]. Finally, the supervision of IPC officers during the donning and doffing procedures was highly appreciated [4 (3-4)] (Table 2).
Association Between Items and Scores
The groups included, chosen from the sections background, social habits, working activity inside the BFH and efficacy, and the differences between them in the scores or specific SS’s sub-scores are reported in Tables 3-6. Regarding the “background” groups, when comparing clinical HCWs and non-clinical HCWs groups, no statistically significant differences were found in the RPS and SS. However, non-clinical HCWs had a higher CS (p<0.001). There was no significant difference in the RPS and SS between those who had already worked with COVID-19 patients and who did not, while the CS was higher in the group of HCWs who did not have previous experience with these patients (p=0.022). Among the HCWs who had previous experience with COVID-19 patients, those who felt unsafe in their previous job had a higher RPS (p=0.041), while no differences were found in the CS and the SS between those who felt safe and who felt unsafe in their previous job experience with COVID-19 patients. The RPS and CS were not statistically different between HCWs who had previous experience with PPE compared to HCWs who never worked with PPE, while the SS was higher in the group who had previous experience with infectious patients requiring PPE (p=0.038) (Table 3).
Note: an: numbers of people who completed the full score
bRSP: Risk Perception Score
cCS: Compliance Score
dSS: Safety Score
eScore results were expressed in median (25-75).
fDifferences between groups were investigated using Mann-Whitney test. A p-value of less than 0.05 was considered statistically significant.
Note : an: numbers of people who completed the full score
b*n: the number of people who completed the SS is the same of the people who completed all the SS’s sub-scores
cRSP: Risk Perception Score
dSS: Safety Score
eMeet: Did you feel comfortable in meeting people outside the hospital, without feeling to put them at risk?
fAnx IN: Did you feel calm and without any anxiety while working inside the BFH?
gAnx OUT: Did you feel calm and without any anxiety for the rest of the day?
hSleep: Did you use to sleep well during your working period at BFH?
iScore or sub-score results were expressed in median (25-75).
jDifferences between groups were investigated using Mann-Whitney test. A p-value of less than 0.05 was considered statistically significant.
kNo statistically significant differences in the Compliance Score were found (data not shown).
Table 5. Differences in the RPS, CS, SS and SS’s sub-scores between the “working activities inside the BFH” groups.
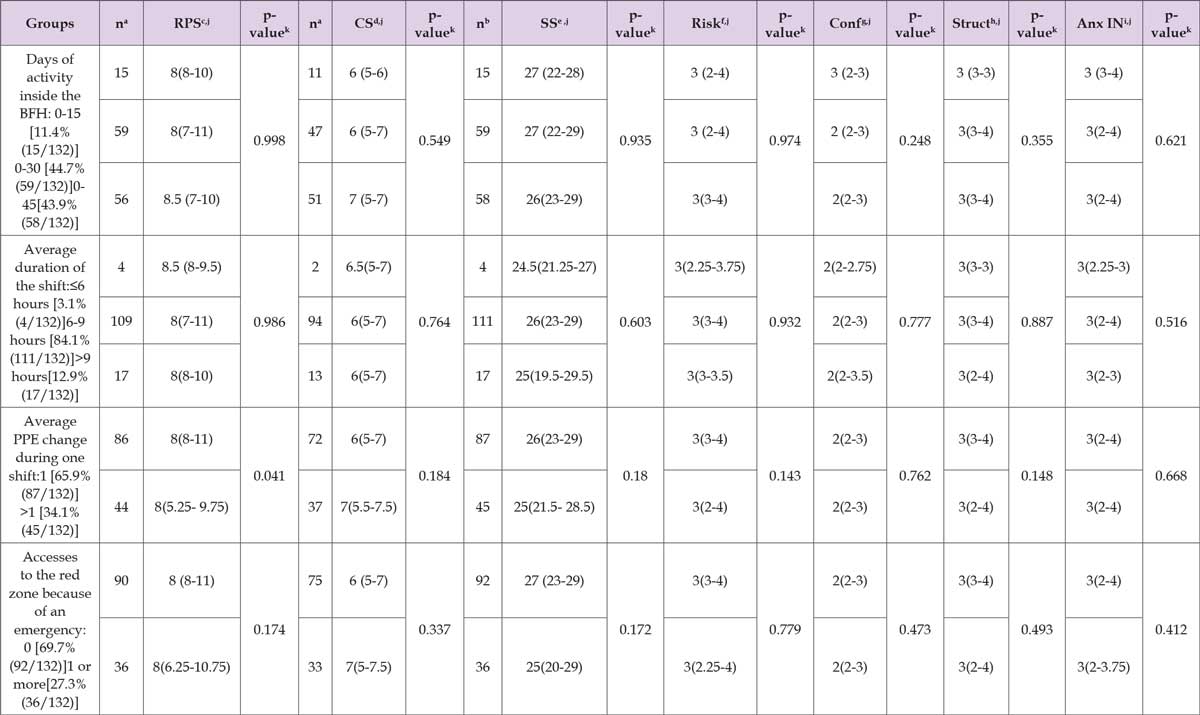
Note: an: number of people who completed the full score
bn: the number of people who completed the SS is the same of the people who completed all the SS’s sub-scores.
cRSP: Risk Perception Score
dCS: compliance score
eSS: Safety Score
fRisk: Did you consider yourself protected from the risk of contracting COVID-19 inside this hospital?
gConf.: How confident do you feel to work with patients wearing the PPE?
hStruct.: Do you think that BFH’s structure is effective in reducing the risk related to COVID-19 infection?
iAnx IN: Did you feel calm and without any anxiety while working inside the BFH?
jScore or sub-score results were expressed in median (25-75).
kDifferences between groups were investigated using Mann-Whitney or Kruskall-Wallis tests. A p-value of less than 0.05 was considered statistically
significant.
Note: an: numbers of people who completed the full score.
bn: the number of people who completed the SS is the same of the people who completed all the SS’s sub-scores
cRSP: Risk Perception Score
dCS: Compliance Score
eSS: Safety Score
fConf.: How confident do you feel to work with patients wearing the PPE?
gAnx. IN: Did you feel calm and without any anxiety while working inside the BFH?
hScore or sub-score results were expressed in median (25-75).
iDifferences between groups were investigated using Mann-Whitney test. A p-value of less than 0.05 was considered statistically significant.
In the “social habits” groups, those who lived in a private house had a higher SS (p=0.048) and a better quality of sleep (p=0.007) compared to HCWs living in a shared accommodation. No significant differences in the three scores or SS’s sub-scores were found between those who had social contacts with other HCWs outside the BFH and those who did not. Regarding the group of HCWs who used to have social contacts with non-HCWs, such as family or friends outside the hospital, their quality of sleep was better (p=0.011) compared to those who avoided meeting non-HCWs outside the hospital. As expected, the previous group had a higher score in the SS’s sub-score “did you feel comfortable in meeting people outside the hospital, without feeling to put them at risk?” (p=0.003) (Table 4).
No correlations were found in the “working activities inside the BFH” groups, with the exception of a higher RPS in the group of HCWs who used to change their PPE just once during their shift, compared to the HCWs who used to change their PPE more than once (p=0.041) (Table 5). Regarding the “efficacy” groups, no statistically significant differences were found in the scores between HCWs who needed less than 3 shifts to become confident with the safety procedures in place at the BFH compared to those who needed more shifts or were still not confident at the time of the survey. Interestingly, who needed less than 3 shifts to become confident had a higher score in the SS’s sub-score “did you feel calm and without any anxiety while working inside the BFH?” (p=0.004). Finally, who found the safety procedures in place at BFH “a lot clear”, had a higher SS (p=0.029) and a higher aforementioned anxiety sub-score (p=0.002), compared to HCWs who found the safety procedures just “enough clear” (Table 6). No correlations were found among the three scores.
The COVID-19 pandemic heavily impacted HCWs’ physical and mental health [1-3,6,8], therefore their perception of working in a safe environment should be taken into account as a matter of the utmost importance, especially in planning healthcare facilities’ preparedness to disasters response. Staff’s well-being should be the priority in any workplace, especially in facilities where patients with contagious respiratory diseases with similar transmissibility and mechanisms of transmission of COVID-19 [12] are hospitalized. This survey explored HCWs’ perceived risk confronting COVID-19 at the BFH during the first hit of the pandemic, raising some interesting points regarding staff safety self-perception and compliance with IPC measures taken in place.
The percentage of HCWs replying to the survey was high and in line with other similar published surveys [13-15]. The results of our survey showed how previous job experience influenced compliance with IPC measures in the workplace and the safety perception of it. Even if the overall compliance to IPC measures was high, less experienced staff were keener on following more strictly the safety suggested behaviours compared to their more experienced colleagues, who, on the other hand, had a higher safety perception. We believe that these findings are particularly relevant considering future COVID-19 pandemic waves. The more the HCWs get experienced with the use of PPE, the higher the risk of being less compliant with safety measures might be. Therefore, we strongly recommend providing constant supervision in PPE use, especially in delicate procedures such as donning and doffing.
Social habits adopted while working in such an overwhelming situation are important too, in order to relieve stress [16-18]. According to our survey, living in a private accommodation (alone or with the household) together with meeting family or friends outside working hours might have helped with coping, as proven by a better quality of sleep in these groups of HCWs compared to HCWs who lived in a shared accommodation with other HCWs and HCWs not used to meet non-HCWs outside the BFH. In the context of a pandemic, this may be linked to a higher fear of getting infected when living and sharing common spaces with other HCWs and a bigger sense of loneliness resulting from the lack of social interactions outside working hours. To support this, our survey showed that living in a private accommodation helped to have a higher safety perception of working at BFH. While HCWs’ background and social habits had an impact on the survey results, the organization of the shifts (number of worked hours or worked days) at the BFH didn’t significantly influence staff behaviours or safety perception inside the workplace.
Regarding the efficacy of the BFH organization in increasing HCWs’ safety self-perception, our survey showed that HCWs who felt confident with the safety procedures in place, had a higher safety selfperception at the workplace, which was associated with a reduction in the level of anxiety. In fact, BFH HCWs who became confident with the PPE donning and doffing procedures in a few shifts and had a very clear understanding of protocols in place, felt more secure and calm while experiencing their work at BFH compared to HCWs who felt less confident. However, a noteworthy result is that all the HCWs found BFH’s structures and procedures clear. More interestingly, the global SS was high, a result that underlines the strengths of BFH in terms of structure, use of space, protocols, and procedures. This is particularly relevant when considering that half of the HCWs with previous experience with COVID-19 patients reported having felt unsafe in their previous workplace. These results stressed the importance of staff training and supervision in the use of PPE and the need for clarity in space divisions and pathways which should be in place in any COVID-19 ward, to secure a higher perception of safety.
This study has several limitations. Its results might have been influenced by other factors not investigated, such as circumstances linked to the unprecedented situation or other social and working activities not explored in the survey and might have suffered recall bias because of the self-reported nature of the information. Moreover, some of the results might have been affected by the fact that data were partially collected during the Italian lockdown. Not all HCWs reply to all the questions, as the survey was ideated partially compulsory. Consequently, some data was missed, and the sample size might have been affected. Even with these limitations, we believe that BFH has proven its efficacy in increasing the staff safety self- perception, and therefore it ensured a better quality of life for the employed HCWs. In fact, despite the severity of the COVID-19 outbreak in Bergamo and the serious physical and mental consequences on local HCWs, the results of our survey showed that the BFH represented a valuable example of an emergency field hospital preserving staff safety selfperception.
The use and organization of BFH spaces, the adopted IPC protocols, the constant surveillance by IPC officers, and HCWs’ training in the use of PPE resulted as key elements in increasing HCWs’ safety selfperception and, therefore, can be a source of inspiration in addressing HCWs’ perceived risk in futures emergencies.
We thank all the staff employed at the BFH for the amazing work done for the city of Bergamo and for taking part in the survey.
All authors report no conflicts of interest relevant to this article.


