Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Luiz Eduardo Imbelloni1,2*, Bruno Basílio Cardoso3, Diana Borges Dock Nascimento4, Claudia Carrada Torres5, Sylvio Valença de Lemos Neto6, Ana Cristina Pinho7, Anna Lúcia Calaça Rivoli8 and Geraldo Borges de Morais Filho9,10
Received: May 03, 2023; Published: May 12, 2023
*Corresponding author: Luiz Eduardo Imbelloni, Researcher, Senior Nacional Cancer Institute (INCA) and Co-responsible for CET-SBA Hospital Clínicas Municipal de São Bernardo do Campo, Rio de Janeiro, Brazil
DOI: 10.26717/BJSTR.2023.50.007942
Background: The assessment of body composition in the pediatric population is essential for adequate
nutritional support during hospitalization. The Body Mass Index (BMI) classically classifies obesity in
adults, but its use in children and adolescents is inadequate, evaluated with percentiles/z-score. Several
methods are used to verify the amount of fat in patients, through CT and MRI, mainly in the lumbar spaces.
The aim of this study was to evaluate the distance between the skin and the end of the subcutaneous tissue
in three different thoracic segments in children aged 0 to 13 years.
Methods: Retrospective study with 105 children aged 0 to 13 years in the supine position underwent MRI,
and the 2nd, 5th, and 10th thoracic segments were measured. The following parameter was evaluated
the distance between skin and the subcutaneous tissue. Demographic characteristics included children’s
gender, age, weight, and height at the time of the MRI examination. BMI was calculated for each subject by
dividing weight in kilograms by square height in meters. The Kruskal-Wallis non-parametric test was used,
and the significance level adopted is 0.05.
Results: This study evaluated 29 female and 40 male children. There is no significant difference in BMI
between genders (p-value of 0.5313). The mean distance between Skin-SCT was 10.13±5.62 mm at T2,
8.08±5.24 mm at T5, and 7.61±5.96 mm at T10, with a significant difference (p=0,00023), being the
greatest distance found in T2. The Skin-SCT at T10 was shorter than the other two measurements. Using
the Z-scale most of the children were eutrophic.
Conclusion: The three thoracic levels (T2, T5, T10) to measure the Skin-SCT distance can be used to correlate with BMI, providing new studies and correlating with the most frequently used lumbar metameres.
Keywords: Anatomy; Magnetic Resonance Imaging; Body Mass Index; Childhood Obesity; Subcutaneous Adipose Tissue
Keypoints
Question: A retrospectively investigated of the distance from the skin and subcutaneous tissue (Skin-SCT) in
three intervertebral space thoracic, analyzing the MRI of children aged 0 to 13 years, without spinal or spinal
cord disease, since the measurement in the thoracic region correlates with fat.
Findings: The mean Skin-SCT was 10.13±5.62 mm at T2, 8.08±5.24 mm at T5, and 7.61±5.96 mm at T10.
The distance varied from 2.00 mm to 35.70 mm in the three segments. The lowest values found in the three
segments (T2=2.30mm; T5=2:10 mm; T10=2.00 mm) were observed in the 2-year-old child.
Meaning: The three thoracic levels (T2, T5, T10) to measure the Skin-SCT distance can be used to correlate
with BMI, providing new studies and correlating with the most frequently used lumbar metameres.
Assessment of the growing skeleton is the focus of growing interest in pediatric medicine. The assessment of body composition in the pediatric population is essential for adequate nutritional support during hospitalization. However, currently available methods have limitations. In a recent study with 262 healthy individuals aged between 6 and 18 years, they underwent magnetic resonance imaging (MRI) and anthropometric measurements [1]. MRI of the second lumbar vertebra was used by two radiologists to perform tissue segmentation. The frequent use of MRI scans in the pediatric population may allow assessment of body composition and adequate nutritional support, showing that the assessment of adipose tissue with this method is highly reproducible and suggests that MRI-derived reference values can be implemented in clinical practice [1].
The Body Mass Index (BMI) classically classifies obesity in adults, but its use in children and adolescents is inadequate. Volumetric visceral abdominal adipose tissue (VAT) and subcutaneous abdominal adipose tissue (SAT) as measured by computed tomography (CT) are associated with metabolic risk factors. With this approach, all adipose tissue measurements can be obtained from routine diagnostic protocol with a high correlation to MRI whole-body examination adipose tissue volumes. Recent studies, using MRI techniques, report that a single image 5cm to 10cm above L4-L5 better approximates total VAT mass than a single image taken at the level of L4-L5 [2-4]. A method that meets these requirements was already validated in adult population fat quantification from a single CT and MRI slice at the following levels T12-L1, L1-L2, L2-L3, L3-L4, and L4-L5 [4-8].
The prediction of total subcutaneous abdominal, intraperitoneal, and retroperitoneal adipose tissue masses in men by a single axial MRI slice [9]. Aiming to describe abdominal adipose tissue distribution in 170 children, determine the influence of gender, stage of maturation, and BMI on abdominal adipose tissue distribution, and compare the ability of BMI and waist circumference to predict abdominal adipose tissue, concluding that waist circumference and BMI offer a feasible alternative to the MRI estimation of intra-abdominal adipose tissue and subcutaneous abdominal adipose tissue, respectively, of children [10]. The adipose tissue of the human body can be obtained through the measurements of protocols with high correlation with MRI examination, mainly in the lumbar regions. Thus, the aim of this study was to correlate the distance between the skin and the end of the subcutaneous tissue (Skin-SCT) in three different thoracic segments (T2, T5, and T10) with the weight and height of children aged 0 to 13 years. The second objective was to evaluate whether measurements in the thoracic region can be considered for this correlation and if they present higher values than measurements in the lumbar region.
The Ethics and Research Committee approved a retrospective study under number 0867/2009 for the evaluation of the thoracic and lumbar spine by MRI in adults and extended to children between 0 and 13 years old. As this is a retrospective study, the waiver of the Free and Informed Consent Form was requested and approved. Between April 1, 2019, to June 30, 2022, selected to evaluate the MRI performed at the Cancer Hospital (HC 1) of the National Cancer Institute (INCA), and the MRI was evaluated in the database of the Department of Radiology. All healthy children were examined supine with the MRI 1.5-T superconducting system scanner (Gyroscan Intera, Philips Medical Systems, Best, the Netherlands) or Magneto Symphony 1.5-T Siemens. Each MRI exam complied with the protocol established by the radiology service and evaluated patients with different clinical conditions. The results obtained were stored in a digital imaging system.
The inclusion criteria for this research were child patients of both sexes, aged between 0 and 13 years, who did not present any cervical, thoracic, lumbar, and/or cord spine pathology. Demographic characteristics included children’s gender, age, weight, and height at the time of the MRI examination. BMI was calculated for each subject by dividing weight in kilograms by the square of the height in m2. Weight was measured to 0.01 kg and height to 0.01 cm using a digital scale. The images of the thoracic spine were performed using the Spin-Echo sagittal slice. The measurements were evaluated in the 2nd, 5th, and 10th thoracic vertebral segments (Figure 1). The distance between the Skin-SCT was measured in a horizontal position perpendicular to the cord spine in the three thoracic intervertebral spaces in a horizontal position perpendicular to the cord spine. Each space was measured three times and the mean value between these measurements was calculated.
BMI (kg/m2) is a measure of body fat determined by a simple calculation using height and weight. The Z score, the number resulting from the calculation, indicates where you fall in the body fat measurement range. The children were weighed in underclothes and measured to the nearest 0.1 kg on electronic step scales, and their height was measured to the nearest 0.1 cm with a wall-mounted stadiometer [11].
Kruskal-Wallis’s rank test or one-way analysis of variance at ranks is a non-parametric method for testing whether samples come from the same distribution. The significance level adopted is 0.05. Spearman’s correlation assesses the monotonic relationship between two continuous or ordinal variables. In a monotonic relationship, the variables tend to change together but not necessarily at a constant rate. The Spearman correlation coefficient is based on the ranked values of each variable, rather than the raw data. Spearman’s correlation is a non-parametric alternative to Pearson’s correlation.
In the period from April 1, 2019, to June 30, 2022, 21,392 MRIs were performed at the hospital. Using patients born between April 1, 2006, and June 30, 2022, we found 3,055 MRIs. Using the following terms as filters: dorsal column, thoracic column, total column, spinal cord compression, and neuroaxis 252 MRI exams were selected for the research. MRI exams that presented the following terms were excluded: intradural, intramedullary, or extramedullary lesions; and/or extradural injuries with spinal cord compression; and/or exams where the skin has been cut in the image; and/or patients over 13 years of age; and/or exams of the same patient, resulting in 105 selected exams. Of these 105 children, 36 were external and were not evaluated by the Department of Nutrition regarding weight and height, therefore, 69 children aged 0 to 13 years were evaluated (Figure 2).
In the study, the period was retrospectively evaluated, with 29 female and 40 male children. There is no significant difference in patients’ characteristics regarding age, weight, height, sex, and BMI (Table 1 & Figure 3). There is no significant difference in BMI between genders (Figures 4 & 5). Using the Kruskal-Wallis’s test returns a p-value of 0.5313, suggesting that there is no significant difference. There is no evidence to indicate that there is a significant difference in the Skin-SCT distances in the three segments between genders. Using the Friedman test with gender as a group and thoracic segments as a block, we found a p-value of 0.08326, suggesting that there are no significant differences in distances by sex (Table 2 & Figure 5).
Table 2. Minimum, mean (standard deviation), and maximum, in millimeters, skin to subcutaneous cell tissue distances. P-value = 0.08326 (Friedman test).
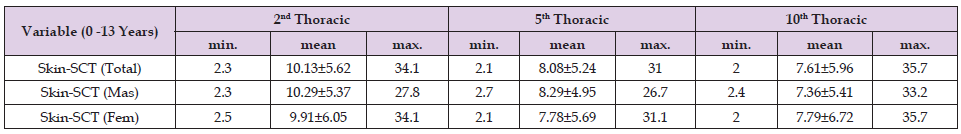
The distance between the Skin-SCT is significant in the upper thoracic region (T2=10.13 mm) than in the middle thoracic region (T5=8.08 mm), and lower thoracic level (T10=7.61 mm) (Table 2). The distance varied from 2.00 mm to 35.70 mm in the three segments. The Skin-SCT measurement at T2 has measurements greater than T5 and T10 (Figures 6 & 7). The BMI degrees found by the Z-score scale are shown in (Table 3). Practically half of the children evaluated by MRI were eutrophic. There is no significant correlation between the measurements and the Z-score scale. There is a significant correlation between the distances in the three thoracic spaces and BMI. Using the Kruskal-Wally’s test (p-value = 0.1892) there is no significant difference between the masses of individuals by gender.
Measurements of the subcutaneous tissue in the thoracic region have been used, mainly in adults, to correlate with cardiac massage, visceral adiposity, lung function, and even obesity in dogs. The assessment and consequences of visceral fat deposition in adults are extensively studied, but little attention has been paid to its measurement in children. This study with children aged 0 to 13 years evaluated the distance between the skin and subcutaneous tissue in three metamers (T2, T5, T10) and showed correlation. Visceral adipose tissue (VAT) is widely recognized as conveying the highest health risk in humans among the currently measurable adipose tissue compartments, traditionally measured between L4-L5. Computerized axial tomography (CT) and magnetic resonance imaging (MRI) provide an important opportunity to quantify VAT in vivo. In both men and women, the VAT slice area at the traditional L4-L5 level is not the best marker of obesity- related health risk [3,4]. Single slice VAT areas 5-10cm above the L4-L5 level have a higher correlation with health risk factors than the VAT area at the traditional L4-L5 level adjusted for age, race, menopause status, scan position, and measurement laboratory [3,4].
Of the available techniques, imaging methods such as CT and MRI provide the most precise estimates of internal adipose tissue deposition in children. Magnetic resonance plays a unique role in diagnosing and managing pediatric abdominal masses [12]. Due to the safety of using MRI to verify abdominal masses, we used the measurement from the skin to the subcutaneous cellular tissue in three intervertebral thoracic spaces to verify the correlation with the BMI of children aged 0 to 13 years. Few studies have documented abdominal adiposity parameters in samples of 11-year-old boys and girls demonstrating the normal BMI range, with small sample sizes [13]. This small population study showed that it is possible to correlate weight and height by measuring the Skin-SCT distances in three thoracic segments.
The onset of obesity may occur in childhood and may persist until adulthood. The early diagnosis of overweight or obesity is of great interest to public health because the treatment in this initial phase of life can be more efficient and less costly for the health system. In childhood it is difficult to assess obesity due to the intense modification of the body structure during growth, there is no systematic classification of childhood obesity universally accepted [14]. Thus, the aim of this study was to propose a new way of assessing children’s BMI by measuring the distances in the three thoracic segments. In 1996, a simplified method was developed in 49 men, to determine the masses of various compartments of abdominal adipose tissue, through axial MRI circles obtained at various intervertebral levels from the 12th thoracic vertebra to the 1st sacral vertebra calculated from contiguous slices of 10 mm thick MRI covering the entire abdomen [9]. And in 2000 the measured adipose issue was in a single image at the level of the umbilicus in 16 obese females [15]. With this possibility of measurements in the thoracic region, possibly new studies can be carried out correlating with the adiposity of children.
Visceral adipose tissue (VAT) is typically measured using a single MRI or CT image at the L3-L4 or L4-L5 intervertebral space, is used to represent abdominal subcutaneous and visceral adiposity [16]. These new thoracic measurements can be used to correlate adiposity and obesity in children. A study compared dual-energy x-ray absorptiometry (DXA) in measuring visceral and subcutaneous adipose tissue (VAT and SAT) with MRI in 309 children/adolescents showed that SAT by DXA reflects MRI measures in children [17]. To assess the relationship between anthropometry and VAT and subcutaneous adipose tissue (SAT), body mass index (BMI), and waist circumference (WC) by MRI in children aged 7-16-year-old, showed that WC can be considered a good predictor of VAT as well as BMI of SAT [18]. To determine the depth of thoracic (T3) for adequacy of chest compressions SAT and to correlate this with BMI, a study was carried out on 55 patients with a diagnosis of obesity or morbid obesity, demonstrating a clear and significant relationship between BMI and both previous and later SAT [19]. No study was found in children with this objective.
In a study with adults of both sexes with the objective of assessing the impact of thoracic adiposity on lung function in a population without respiratory diseases, it showed a significantly associated with decreased lung function [20]. Studying children and adolescents (aged 6-18 years) overweight and obesity in different populations, the references examined produce similar estimates of overall overweight prevalence but different estimates of obesity [21]. One should be cautious when comparing results based on different references [21].
Of the two axial images used in our comparisons, VAT area at L2- L3 was significantly better correlated with total VAT volume and explained a greater amount of the total variance compared to L4-L5 [8]. Likewise, our study showed great variation in measurements in the three intervertebral spaces.
In a recent review article on obesity imaging, MRI is ideally suited to the quantification of fat, since most of the acquired signal comes from water and fat protons [22]. Whole-body MRI is superior to dual- energy X-ray absorptiometry (DXA), having a T1 sequence, called T1 DIXON, which we obtain a fat map of the whole body [22]. In this way fat fraction quantification is becoming established as a clinical and research tool, and understanding the underlying principles will be helpful to both imaging scientists and clinicians [22]. To determine whether subcutaneous fat thickness measured on thoracic radiographs was associated with body condition score (BCS) in dogs, there was a significant association between BCS, and subcutaneous fat thickness measured on thoracic radiographs [23]. This study carried out in dogs encouraged us to use MRI instead of chest radiography in the same region in children.
Historically, L4-L5 was selected as a landmark as it represented the site most predictive of total adiposity, and not visceral adiposity. Various lumbar levels and 5 to 10 cm above L4-L5 have been used to assess obesity in men and women. However, few studies have evaluated this relationship in children. Most studies in medical literature are performed with obese children. In this study with children aged 0 to 13 years, 49.2% were eutrophic children, and the study was to correlate the distance from the skin to the subcutaneous tissue at three levels (T2, T5, T10) in the thoracic region. The three thoracic levels (T2, T5, T10) to measure the Skin-SCT distance can be used to correlate with BMI, providing new studies and correlating with the most frequently used lumbar metameres.


