Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Hening Tirta Kusumawardani1, Farid Yudoyono2, Eko Budi Prasetyo3 and Sudadi1*
Received: April 13, 2023; Published: May 09, 2023
*Corresponding author: Sudadi, Anesthesiology and Intensive Therapy Department, Gadjah Mada University/ dr. Sardjito National General Hospital, Yogyakarta, Indonesia
DOI: 10.26717/BJSTR.2023.50.007930
Background: Prognostic models are important tools for heterogeneity adjustment in traumatic brain injury (TBI). Prognosis of TBI has been particularly challenging to predict, with limited availability of robust prognostic models. Recently, however, some new prognostic models specifically designed for patients with TBI were introduced. Still, the optimal type of prognostic model in TBI remains unknown.
Methods: This is a retrospective study, using data obtained from outpatient registry at our hospital, Dr. Sardjito National General Hospital, a tertiary hospital in Yogyakarta Indonesia. Data was collected in January 2017 to June 2021. Potential prognostic factors were analyzed by STATA 15.0. Roctab analysis is used to determine the cut-off value of each numerical variable. Retrospective analysis with cox proportional‐hazard was used to measure the contribution of each variable to the treatment’s outcome.
Results: We enrolled a total of 426 patients diagnosed with TBI with intracranial hemorrhage who treat emergency surgery at emergency department. Based on retrospective analysis, hypotension condition (HR 4.61, 95% CI 3.78-7.64, p = <0.001), blood glucose (HR 3.08, 95%CI 2.10-4.53, p = < 0.001), anemia condition (HR 2.99, 95% CI 2.05-21.99, p value < 0.001), Glasgow Coma Scale (<8) (HR 2.64, 95% CI 2.33- 3.73, p value < 0.001), male (HR 2.47, 95% CI 2.05 –21.99, p value 0.001). The prognostic scoring model has sensitivity value of 83.93%, specificity 84.73% respectively.
Conclusion: This study shows that these changes were as a result of several factors to predict mortality. Inadequate perioperative management can cause brain cell death and increased intracranial pressure, resulting in increased event of herniation, so the consequent has led to worsening the patient’s prognosis.
Keywords: Traumatic Brain Injury; Prognostic Factors; Anesthesia; Perioperative
Abbreviations: PH: Proportional Hazard; HR: Hazard Ratio; CI: Confidence Interval; GCS: Glasgow Coma Scale; CT: Computerized Tomography; BP: Blood Pressure; PR: Pulse Rate; RR: Respiration Rate; SBP: Systolic Blood Pressure; TBI: Traumatic Brain Injury
TBI is a global healthcare and socioeconomic issue [1]. If one in every two of these patients dies or is left with significant lifelong disability, TBI has a terrible prognosis [2,3]. It has historically been difficult to establish an early and reliable prognosis in people with TBI [4]. More precise prognoses are now possible thanks to advancements in statistical modeling and big patient datasets [5,6]. Prognostic models are statistical models that use two or more variables to compute the probability of a predetermined result [7]. Although patients with TBI are found in trauma and intensive care units, there have been few similar applications of prognostic models in TBI research, probably due to the poor quality of earlier models [5-8]. Because of the vast illness heterogeneity, including differences in origin, pathophysiology, therapy, and outcome, developing an adequate predictive model for TBI patients remains difficult [7]. As a result, the researchers wanted to see if prognostic trauma models might be used to predict long-term outcomes in TBI patients. A secondary goal was to figure out if there was a link between risk factors and result.
Study Design and patients
We reviewed all medical records of patients diagnosed as traumatic brain injury who admitted to emergency unit and immediately surgery between January 2017 to June 2021 from medical record registry of Dr. Sardjito Mangunkusumo National General Hospital, a tertiary hospital in Yogyakarta, Indonesia. The inclusion criteria were complete medical records, Indonesian citizen at any age, has provided a documented consent for participants ≥ 14 years old, willing to comply with the study procedures, diagnosed as TBI ICD X, (S06.0 and S02.0). Exclusion criteria in this study were: incomplete medical records, having comorbid diseases such as hemorrhagic shock, trauma on thorax, abdomen, and extremity region, especially long bone, multiple traumas, and irreversible shock patient who had resuscitation before. The total number of patients with clinical TBI 647, it is not known exactly how prevalence of patients with traumatic brain injury in Dr. Sardjito National General Hospital Yogyakarta. The number of samples selected and set as the sample of the study was 269 (Figure 1). This study was approved by Research Ethics Committee of Faculty of Nurse, Public Health, and Medicine, Gadjah Mada University, Yogyarta, Indonesia.
Outcome
There are 3 outcomes to be achieved, estimate and interpretation of hazard function and survival function, compare 2 survival function, and get relationship between explanatory variable with survival time by controlling all covariates. With survival expected to be done estimation and interpretation of survivor and hazard of survival data.
Statistical Analysis
All data were analyzed using STATA version 15.0. Analysis of association between variables and the duration of follow‐up during treatment can be seen from mathematic model between one variable and others using multivariate analysis cox proportional‐hazard. All independent variables will undergo tests, that is proportional hazard (PH) assumption test through representation or global statistical test.
The total patients with clinical TBI 647, it is not known exactly how prevalence of patients with traumatic brain injury in Indonesia. The number of samples selected and set as the sample of the study was 426. Flow algorithm patient enrollment showed in (Figure 1). Univariate baseline of patients’ characteristics presented in (Table 1) and Kaplan Meier of incident of death based on two of the most influencing factors are presented in (Figures 2 & 3). Kaplan‐Meier survival curve is used to determine the characteristics of survival. The following will explain the characteristics of traumatic brain injury patients based on the dominant factors suspected. This analysis was continued with the log rank test to find out whether there are differences between survival curves.
Table 1: Sociodemographic characteristic traumatic brain injury patients at Dr. Sardjito National General Hospital in 2017-2021 and mortality predictors based on time at risk length of stay (number of patients = 426).
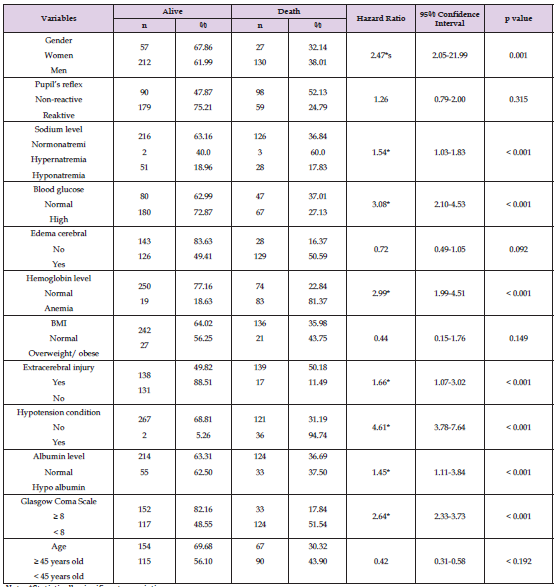
Note: *Statistically significant association.
In the multivariate analysis, several main factors which played significant roles associated with poor prognosis of survival rate were hypotension condition [hazard ratio (HR) 4.61; 95% confidence interval (CI) 3.78-7.64; P = < .001], blood glucose (HR 3.08; 95%CI 2.10- 4.53; P = < .001), anemia condition (HR 2.99; 95%CI 2.05-21.99; P = < .001), Glasgow Coma Scale (<8) (HR 2.64; 95%CI 2.33-3.73; P = < .001), and male gender (HR 2.47; 95%CI 2.05 –21.99; P .001). While pupil’s reflex, incidence of cerebral edem, body mass index, and age history were not significantly associated with survival outcome.
The hazard ratio will determine the amount of risk of patients who can cause death. Hazard Ratio of incident deaths in TBI patients is summarized in (Table 2).
Based on global analysis, variables of hypotension condition, blood glucose level, Glasgow Coma Scale (<8), anemia condition, male gender were the most influential variables in determining prognosis of TBI patients and meet the proportional hazard assumption, thus entering multivariate analysis for prognostic models. From (Figure 2), Kaplan‐Meier curve showed that hypotension condition is one of the most dominant factors suspected to affect the survival outcome of patients with traumatic brain injury. Based on (Figure 2), the survival and recovery curves of normal condition of blood pressure are above the survival curve of hypotension patients’ groups. This means that traumatic brain injury patients in hypotension group tend to have worse prognosis on survival, so maintaining hemodynamic state prior to treatment can affect patient’s outcome.
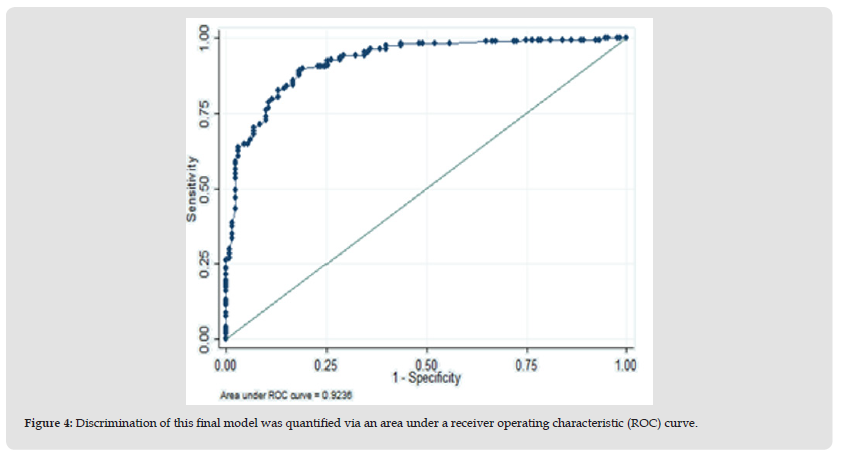
The level of blood glucose is also strongly suspected to affect the survival of patients with traumatic brain injury. Based on (Figure 3), it can be seen that the survival and recovery curves of patients with normal blood glucose is above the survival curve of high level of blood glucose. This means that traumatic brain injury patients with high level of blood glucose (>200 mg/dl) tend to have worse prognosis on survival. Maintain blood glucose with insulin and or oral hyperglycemic drugs prior to treatment can affect patient’s outcome. TBI score of ≥7 maximized the ability to predict death with on the other hand. Furthermore, a cut-off of all total patient TBI scores was determined using the roctab curve and the area under the ROC curve for predicting death was 0.92 (95% CI: 0.839, 0.847) and this model has a sensitivity value of 83.93%, specificity 84.73% respectively. (Figure 4) showed the discrimination plot of sensitivity versus 1-specificity roctab prognostic models of TBI by the curved line. The diagonal line described the non-informative line where sensitivity is equal to specificity and represents the discriminative ability to the test to correctly differentiate between 2 individuals.
Figure 4 Discrimination of this final model was quantified via an area under a receiver operating characteristic (ROC) curve.
Hypoxia:
Hypoxia is more common after trauma and TBI, especially if the patient is not treated right once. This disorder can lead to secondary brain injury, exacerbating the patient’s condition. It has been demonstrated that the neuroprotective impact may be responsible for the better outcomes in preventing hypoxia. Extracranial comorbidities, changes in brain plasticity, or alterations in clinical care associated with rising hypoxic conditions are all plausible causes [7,8].
Glasgow Coma Scale (GCS):
There is considerable evidence for the predictive significance of the GCS on admission to hospital and the GCS motor score, according to the literature [7-9]. Poorer outcomes were linked to lower entrance GCS and GCS motor scores. The GCS revealed a consistent linear relationship between morality and intelligence [10].
Intracranial Pressure:
Following traumatic brain injury, computerized tomography (CT) scanning allows an objective assessment of structural damage to the brain and associated outcomes, as well as determining how far intracranial pressure should be increased. The outcome is linked to the CT classification and individual CT characteristics [7-9]. The independent category of mid-line shift was found to have strong evidence, and the extent of the shift was found to be associated with a worse outcome. Patients with an epidural haematoma had a better prognosis, while those with an acute subdural haematoma had a worse prognosis.10 The evidence for subdural haematoma’s prognostic significance was strong [8]. Traumatic subarachnoid haemorrhage, obliteration of the basal cistern or third ventricle, and non-evacuated haematoma were all linked to a worse 6-month outcome. There was substantial evidence that there was no relationship between intraventricular.haemorrhage and outcome [8,9].
Vital Signs:
Blood pressure (BP), pulse rate (PR), respiration rate (RR), temperature, muscle tone, decorticate or decerebrate posturing, and excessive sweating are all symptoms of TBI [7,8]. Dysautonomia affects 10% of people who survive severe TBI and has been linked to poorer outcomes. The majority of these characteristics were assessed onehalf hour after the patient arrived in the emergency room. Following a TBI, hypotension and hypoxia have been identified as a substantial secondary insult linked to poor outcomes [10,11]. The systolic blood pressure (SBP) and TBI outcome have a distinct U-shaped connection. The best results were shown when SBP was between 135 and 90 mmHg. SBP readings of more than 135 or less than 90 mmHg were linked to poorer health. Outcome. Both increase and decrease in RR beyond normal range is associated with a poor outcome in TBI. In patients with TBI, similar findings about the relationship between PR and morality have been discovered [11].
Laboratory Parameters:
This study describes the predictive value of various laboratory parameters routinely recorded on admission following TBI. Hyperglycemia is a common cause of secondary injury in TBI patients, and it’s linked to a worse result [10]. In patients with traumatic intracranial bleeding, coagulopathy is a key predictor of disability and death. Coagulopathy, particularly prothrombin time and platelets, is linked to patient outcomes following TBI [10-12]. There was a positive linear connection between glucose and prothrombin time and result (increase value associated with poorer outcome) [10,11]. Anaemia is a prevalent condition in critically ill patients, and it has been linked to a worse TBI result [12,13]. The inverse linear relationship between hemoglobin, platelets, and pH and the outcome was discovered (low values associated with poorer outcome). Although both hypo- and hypernatraemia are linked to a worse prognosis, hyponatraemia is a rare occurrence on admission after a TBI [13,14]. The result and sodium had a U-shaped connection. Although sodium has a U-shaped connection with outcome, hyponatraemia is more strongly linked to a worse outcome. Hypernatraemia and outcome, which was predominantly related to death, have a poor association [10,13,14].
This study had already been partially presented at Symposium on Anesthesia Complication, Indonesia in August 2021.
The author and co‐authors of this study declared no conflict of interest.
HTK, FY, and SU conceived the ideas; HTK collected the data; HTK, FY, and EBP analyzed the data; and HTK, FY, EBP, and SU led the writing.


