Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Filipa Correia1, Beatriz Teixeira1-3* and Cláudia Afonso1-3
Received: April 20, 2023; Published: May 03, 2023
*Corresponding author: Beatriz Teixeira, Faculty of Nutrition and Food Sciences, University of Porto, Porto, Portugal
DOI: 10.26717/BJSTR.2023.50.007913
Caregivers’ nutritional status may be negatively affected due to their high emotional burden, which compromise the provision of care. The aim of this systematic review was to understand and summarize what is reported in the literature regarding the informal and formal caregivers’ nutritional status, namely 1) their current nutritional status, 2) the screening tools used and 3) the nutritional status’ related factors. A literature search was carried out on Medline, Scopus, and Web of Science from December 2021 to March 2022, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Only articles written in English or Portuguese were considered. A total of 18 articles were included. These results were obtained by ten different types of methodology, namely: Body Mass Index (BMI), waist circumference, body fat percentage, auto reported weight fluctuation, Cancer Survivor Web- Based Needs Assessment Survey, Mini Nutritional Assessment, Fried Frailty Phenotype, Healthy Eating Index, Health-Promoting Lifestyle Questionnaire II and Australian fruit and vegetable consumption guidelines. Of these, the one that was mostly used was BMI. Seventeen studies studied formal caregivers’ nutritional status and only one studied this issue on informal caregivers. Five factors were exposed in the reviewed articles as influential on caregivers’ nutritional status: sex, age, educational level, caregiving intensity and combining caregiving activities with a part-time/full-time job. Not enough evidence regarding the direct impact of being a caregiver on their nutritional status was found. Still, there’s a high prevalence of overweight, obesity, malnutrition, frailty and diet inadequacy among caregivers. The conduction of more studies (particularly prospective studies) focused in this thematic is essential to increase the level of evidence. This systematic review was registered at www.crd.york.ac.uk/prospero/ as CRD42022321620.
Keywords: Caregiving; Nutritional Status; Screening Tool; Systematic Review
Currently, in Portugal, about 230 to 240 thousand people have a disability or deficiency that makes them totally or partially dependent of someone’s care [1]. The World Health Organization (WHO) estimates that this event happens to over 142 million of people aged 60 years and above [2]. Therefore, the basic needs of people in these circumstances can be provided by formal caregivers, who are professionals that support the performance of the person’s daily activities and/or by informal caregivers who assure the physical and/or emotional care of a “spouse or common-law partner, a relative or similar” [3-5]. Taking this information into consideration and acknowledging that it’s still quite unknown whether older adults’ environments can compensate and allow them to live with dignity, continue to be active and able to thrive, WHO developed a strategy called “Decade of Healthy Ageing” [2]. Thus, the transition to “Decade of Healthy Ageing” shall include the step “to listen to diverse voices and enabling meaningful engagement of caregivers”, in order to be able to support them [2]. In fact, the role of formal and informal caregivers often implies a huge responsibility and, at the same time, an excessive pressure, since caregivers not only become the main strength and support of the care recipient, but also have to do all their routines with low material and financial resources [3-6]. As such, the needs of the people to whom they provide care are usually prioritized in favor of their own multidimensional needs, affecting the quality of life of the caregivers and, indirectly, the quality of the care provided [3]. For instance, dehydration is an example of a neglected caregiver’s need that can directly impact the safety of the care receipt, because it promotes fatigue and impairs visual, psychological (reduces short-term memory and enhance lack of attention and vigilance) and psychomotor skills in the caregiver [7].
Furthermore, not only optimal performance can only be achieved with balanced diets, but also, it’s known that overweight can negatively affect productivity, so poor food quality and inadequate body weight can also damage the care provided by caregivers [7,8]. Having the previous information in mind, although this isn’t an usual investigation issue, it is reasonable to believe that caregivers’ nutritional status may be negatively affected due to the high emotional burden it has on them [3-7]. To the best of the research team’s knowledge, no systematic review has yet summarized information regarding the nutritional status of formal and informal caregivers. Therefore, the aim of this systematic review is to understand and summarize what is reported in the literature regarding the informal and formal caregivers’ nutritional status, namely
1. Their current nutritional status,
2. The screening tools used and
3. The nutritional status’ related factors.
The present study was designed to answer to the Population, Indicator,
Comparator, Outcomes, and Study design (PICOS) question
(Table 1).
Note: 1Indicators and outcomes are different for each objective (1,2 and 3 respectively).
Study Design
This study was developed as a systematic review, in agreement with the Preferred Reporting Items for Systematic Reviews and Meta- Analyses (PRISMA) guidelines [9,10]. Its protocol was submitted and registered with the International Prospective Register of Systematic Reviews (PROSPERO), having the registration number CRD42022321620.
Search Strategy
This systematic review was conducted from December 2021 to March 2022 in three databases: MedLine (PubMed), Web of Science and Scopus. Keywords were selected according to the previous knowledge of the investigation team. Therefore the final search results were identified through the use of the following Boolean expression, in all databases: (Caregivers OR Carer OR Caring OR “Nursing Home” OR “Residential Homes” OR “Health Provider”) AND (“Nutritional Status” OR Nutrition OR “Body Composition” OR “Nutritional Assessment” OR “Body Mass Index” OR Weight OR Obesity OR Adiposity OR “Waist Circumference” OR “Hip Circumference” OR “Sagittal Abdominal Diameter” OR “Mid-upper Arm Circumference” OR “Calf Circumference” OR Skinfold OR Anthropometry OR “Food Consumption” OR “Food Habits” OR “Nutritional consumption” OR “Food Choice”).
Eligibility Criteria
The eligibility criteria used to establish which studies should be included is displayed at Table 1. Moreover, only articles that were already published in English and Portuguese were added to this systematic review. In this systematic review, the snowballing technique procedure was used by checking all the selected articles references in order to find more relevant information [11].
Two researchers screened titles and abstracts to apply the eligibility criteria and, in case of disagreement, a third one confirmed the process. Then, two reviewers extracted data and the other checked. None of the reviewers were blinded to the journal titles nor to the authors’ name. Finally, it wasn’t required to contact the authors of the reviewed articles to obtain extra information, since all the necessary data to answer the study objectives was already displayed in the published articles. The main results of the eligible articles were assembled in Table 2, to summarize them. This table describes the country, study design, types of caregivers and care recipient, methodology, scoring, sample characteristics and nutritional status’ outcomes of the included studies. Identified studies were de-duplicated via Systematic Review Assistant-Deduplication, followed by a manual search in Endnote [12,13]. As it’s shown in Figure 1, a total of 24 fulltext studies were assessed for eligibility and 17 matched the inclusion criteria and were included in the qualitative synthesis.
Cohort and case-control studies included in this systematic review were evaluated from 0 to 9 stars through Newcastle-Ottawa Scale (NOS) [14]. For the reviewed cross-sectional studies, it was applied the NOS adapted version, which has been previously used for this purpose, with a quality score that ranges between 0 and 8 stars [15-17]. In case of disagreement, reviewers debated until reaching a consensus.
The key results of the 18 selected articles (fourteen cross-sectional, three cohorts and one case-control) are displayed in table 2. Most of these studies were developed in America, specifically at United States of America [18-28], four were conducted in Europe [29-32], two in Asia [33,34]. and one in Oceania [25] The sum of all the samples comprised 152357 individuals (of which 40765 were caregivers), and the gender distribution differed between studies, with 0% [28] to 75% [35] males. Regarding the type of caregiver, 17 studies included informal caregivers and one [25] formal caregivers. As for the person that was being cared, seven were about people taking care of elders [19-30], three had adult care recipients [33-35], one included caregivers of children [20], and seven didn’t specify [21-34]. Regarding the reason for dependence, six articles mentioned people with dementia (particularly, Alzheimer’s disease) [18-29], two referred people with cancer [33-35], one about elderly spousal [30], one of children with Autism Spectrum Disease [20], one of people in nursing homes [25], one of people with intellectual and developmental disabilities [28] and the remaining six didn’t mention the cause of dependence [31- 34]. Respecting quality assessment, the mean ± SD quality score of cross-sectional studies was 5,00 ± 1,31 (min: 3; max: 7) and of cohort studies was 5,67 ± 0,47 (min: 5; max: 6). Lastly, the only case-control study had a quality score of 5.
Table 2. Characteristics of the included studies, evaluating the nutritional status of formal and/or informal caregivers.
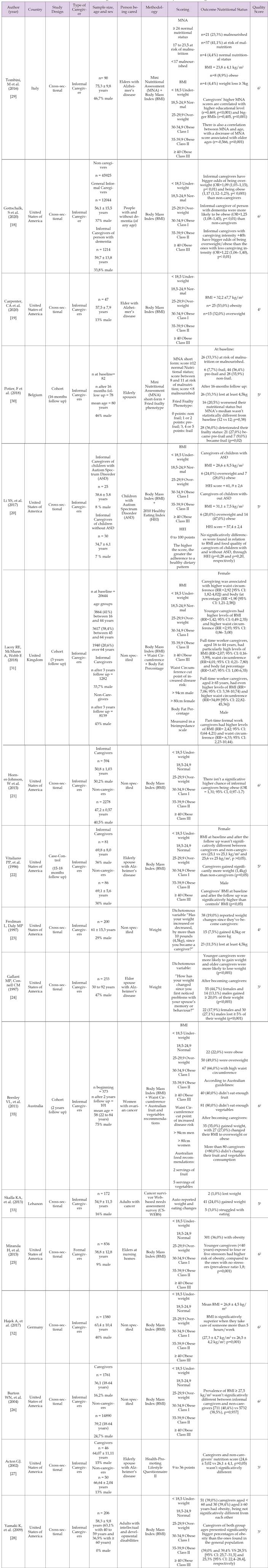
Note: 1Newcastle-Ottawa Scale adapted version for cross-sectional studies (0-8 points)
2Newcastle-Ottawa Scale for cohort studies (0-9 points)
3Newcastle-Ottawa Scale for case-control studies (0-9 points)
The majority (n=17) of the articles included in this systematic review targeted informal caregivers’ nutritional status and only one studied formal caregivers. This one indicated that 36% [25] of the formal caregivers where obese whereas informal caregivers’ obesity prevalence went from 8,9% [29] to 53% [19].
We observed 10 different types of methodology used to assess the nutritional status of caregivers, namely Body Mass Index (BMI), waist circumference, body fat percentage, auto reported weight fluctuation, Cancer Survivor Web-Based Needs Assessment Survey (CS-WEBS), Mini Nutritional Assessment (MNA), Fried Frailty Phenotype, Healthy Eating Index (HEI), Health-Promoting Lifestyle Questionnaire II and Australian fruit and vegetable consumption guidelines. However, the one that stood out as the mostly used was BMI, a math formula that describes the body weight-height relationship [36,37]. This indicator was used as the only source of information regarding the nutritional status, in 9 articles [18-34], and as a complement of other types of measures, in 4 articles [20-35]. In two articles, waist circumference was assessed with a tape measure, by a nurse [31] or by the study participants themselves [35], to establish adiposity levels (combined with other methods) in 2 articles. Furthermore, body fat percentage, estimated by a bioelectrical impedance digital scale, complemented the evaluation of adiposity in one of these articles [31]. Two of the studies had an auto reported weight fluctuation as a dichotomous variable, after a direct question, as an indicator of nutritional status variations after becoming a caregiver.
Plus, an adapted version of CS-WEBS, a questionary composed by 72 questions distributed in 4 domains (physical, psychological, social and spiritual), was the chosen method to assess weight and eating modifications in one article [33]. MNA was applied in 2 studies that had an older sample age. One article used the full form of MNA, with 18 questions regarding anthropometric, overall, diet and subjective assessment, and the other article used the MNA short-form that included 6 items related to diminishing appetite, weight loss, BMI, movement efficiency, emotional strain and neuropsychological complications [29,30]. Moreover, Fried Frailty Phenotype was also used in one elderly sample, thru the assessment of the following components: unintended weight loss superior to 4,5kg in the last 12 months, fatigue, sedentarism, slow walking pace and grip strength (used to measure weakness) [30]. Regarding food quality and/or dietary patterns assessment as an indicator of nutritional status, 3 distinct methodologies were executed in different studies. One study used the 2010 HEI, that assesses the adequacy of the usual consumption of 15 nutrients and 12 food groups, according to American guidelines [20], while another article used the Health-Promoting Lifestyle Questionnaire II, which is a 4-points scale that evaluates the frequency of 52 behaviors regarding six dimensions (nutrition, physical activity, spiritual improvement, social relations and health accountability), each one of them with their own score and a final score related to all domains [27]. Lastly, another study requested that participants recalled the number of fruit and vegetable servings they usually consume per day, to assess if they fulfilled Australian recommendations [35].
Of the 18 reviewed articles, seven compared caregivers with non-caregivers’ nutritional status [18-31]. Of these, four found significant relationships between being a caregiver and having a poorer nutritional status [18-31]. Considering BMI values, its mean ranged, in this systematic review, from 23,8 ± 4,1 kg/m2 [29] to 32,2 ± 7,7 kg/ m2 [19], and the prevalence of obesity and overweight rounded from 8,9% [14] to 53% [19] and from 20% [20] to 49% [35], respectively. Concerning the auto reported impact of caregiving on weight changes, the prevalence of weight gain, in five studies, ranged from 7,5% [23] up to 44,7% [24] and of weight loss prevalence, in four studies, varied between 1% [33] and 33% [30]. Moreover, one study determined that caregivers gained significantly more weight than non-caregivers [22]. In regards of waist circumference, one study established an association between caregiving and higher abdominal adiposity [31]. Another study presented a high prevalence (66%) of caregivers with unhealthy/big waist circumference values [35]. Through the MNA application in two studies, 33,3% (n=26) to 64,4% (n=58) of older caregivers were identified as malnourished or at risk of malnutrition, although there was no statistical evidence of getting minor MNA scores throughout the time [29,30]. Besides, one of the manuscripts found that caregivers’ MNA and BMI were positively correlated [29]. Concerning the use of the Fried Frailty Phenotype in one article, 7,7% (n=6) and 56,4% (n=44) of the elderly caregivers were, respectively, frail and pre-frail. Further, 36% (n=28) of the whole sample significantly deteriorated their frailty status, transitioning either to pre-frail or to frail [30]. Regarding food quality assessed in one study, although a large number of caregivers didn’t eat enough fruit (n=40; 40%) nor vegetables (n=81; 80%), this tendency wasn’t aggravated with the process of caregiving. Also, several caregivers didn’t meet the American recommendations of vitamins D and E, calcium, potassium, folate and fiber [20]. Another article stated that there was no evidence that caregivers’ nutrition score was different comparing with non-caregivers [27].
In this systematic review it was found that sociodemographic characteristics influenced caregivers’ nutritional status. Thus, caregiving was associated with higher levels of adiposity for women, particularly the younger women; also, when they worked full-time and their age was in the range of 16 to 44 years or over 64 years-old, they had even higher BMIs and waist circumferences; men combining part-time paid work with caregiving had higher levels of adiposity than non-caregivers of the same gender that were full-time workers [31]. Nevertheless, another article found that younger formal caregivers were more prone to weight gain, whereas older formal caregivers were more likely to lose weight [24]. Moreover, another study realized that caregivers with less than 40 years and that were exposed to four or five stressors had a higher risk of obesity, compared to the ones with no stressors [25]. Conversely, another study didn’t find significative differences in the prevalence of obesity according to caregivers’ age [28]. Furthermore, regarding the time impact of caregiving activities, it was found in one study that caregivers with tasks that lasted more than five hours per week had significatively higher BMIs [32]. Finally, one study found that two sociodemographic characteristics, level of education and age, also had an influence on malnutrition [29]. More specifically, it was found a positive correlation of caregivers’ MNA with their level of education and a negative correlation with caregivers’ age [29].
This study was designed to review and synthesize information about informal and formal caregivers‘ nutritional status and the corresponding nutritional status measures used described in the literature. To our knowledge, this is the first work that systematically reviewed this issue.
BMI is a broadly used method in public health to estimate mortality and morbidity, due to its convenience (it’s free, fast and simple to use) and trustworthiness [36,37]. Thereupon, it’s understandable that 70,6% (n=13) of the articles reviewed included this nutritional status screening method. However, BMI has the limitation of being incapable to distinguish body composition (in other words, percentage of adipose vs lean tissue) [37]. Consequently, the four articles that used BMI alongside one or two other instrument(s) were capable to reveal a more comprehensive perspective of caregivers’ adiposity levels. Waist circumference is a marker of abdominal adiposity commonly used in the literature, in combination with BMI [37]. In this systematic review, this nutritional status method was referenced in 11,1% (n=2) articles. This perimeter has two major assets:
1. Its simplicity (the only resource required is a non-stretch
tape measure);
2. Its ability to predict cardiovascular diseases risk [37].
Nevertheless, this measurement it’s only valuable in overweight/ obese people, otherwise its data won’t offer a relevant health input [37]. It is important to considered that this measurement has a standardized protocol. However, one of the studies used values obtained by untrained people (study participants), which reduces the reliability of the results [35-37]. Body weight, likewise as BMI, can’t identify fat and muscle mass [37]. Thereby, this isn’t the most accurate measure reported in this systematic review (n= 2 articles), since weight variations may be related to an increase/decrease of fat, muscle and/ or water [37]. Still, weight changes, particularly unintentional weight loss can be used as a health status predictor because of its association with a set of diseases, such as cardiovascular and liver complications, cancer, diabetes and arthritis [38]. The only informatic tool that appeared in the present systematic review was the CS-WEBS, which is an online questioner that addressed questions regarding weight and eating behaviors changes [33]. This tool main strengths are the following ones: [1] the fact that has really low complexity to answer and [2] the presence of an algorithm that only enabled the exhibition of questions that were relevant to the caregivers’ context, diminishing the response fatigue and abandonment of the survey [33-39]. On the other hand, since internet access it’s mandatory to conduct this method, it’s not available to everyone and, consequently, the study that used CS-WEBS may not be representative of the whole population [33-39]. MNA appears in 2 articles (11,1%) of this manuscript. In fact, this tool is the commonly used tool regarding older adults’ nutritional screening. Besides, both full and short MNA forms are validated and considered the standard to scientifically support rather than other nutritional assessment instruments [40].
Another vulnerable characteristic that is associated with aging is frailty, a clinical condition whose operational definition hasn’t yet been consensually defined [41]. Still, frailty is considered a process that changes over time (individuals’ frail status can be either improved or deteriorated) and it is characterized by difficult, or even impossible, recovery from numerous health traumas [30-41]. Currently there isn’t a recognized golden standard to assess frailty. However Fried Frailty Phenotype is one of the tools that has been widely used and acknowledge as an adequate method [30-41]. In this review, this tool is used in 1 article (5,6%). Further, one of the analyzed studies screened MNA and Fried Frailty Phenotype, which a good practice and is coherent with what is described in literature, because although there is a robust relationship between malnutrition and physical frailty, both parameters should be assessed separately to give a more meticulous overview of elders’ health status [40]. Diet quality was screened through HEI in one of the studies of this systematic review, what granted a total score that’s both reliable and valid for the American population [19-40]. This tool gives a broad information because not only it includes nine items that assess diet adequacy and three that evaluate the consumption of food groups with less nutritional value, but also, both individual component scores and the final (sum of all scores) score can give important information regarding the person’s diet [20-42]. In another article of this review, the adherence to a healthy dietary pattern was assessed through the recall of fruits and vegetables daily intake, to compare it with the Australian recommendations [35]. These two food groups may have been chosen due to their well-documented inverse association with the risk of all-cause mortality and certain non-communicable diseases, namely cardiovascular diseases, stroke and cancer [43]. However, self-report of fruit and vegetable consumption is usually overestimated, because this method is linked with social approval bias, i.e., people report food habits that are considered healthier, because that’s socially desirable [44]. Nevertheless, informal caregivers showed a deeply inadequate intake of fruit and, particularly, vegetables [35].
BMI screening is important to assess health outcomes, since an increased weight-height relationship is associated with a higher risk of, not only, noncommunicable diseases, but also all-cause and cardiovascular disease mortality [8-37]. Having this in mind, informal caregivers might be more vulnerable to this health problems, since one study showed that 35% of caregivers gained weight and 27% of them became overweight or obese after starting to care of someone [35]. On the other hand, overworked formal caregivers might also have superior health risks, because each extra hour/week of providing nursing care services was associated with an increase of around 0,01 kg/m2 of their BMIs in another study [32]. The remaining studies that measured BMI in this review only assessed overweight/obesity rates but did not establish any association with caregiving related factors. Although, 14 of the 18 manuscripts that explored BMI in this systematic review were cross-sectional (which makes it impossible to investigate cause–effect associations), the importance of monitor both informal and formal caregivers, to assure that they won’t get health complications inherent with a bigger BMI, it’s still noticeable. Additional anthropometric measures were described in the literature. One of them was waist circumference, an abdominal adiposity indicator, present in two of the 18 articles in this review. One of the studies included found an association of caregiving with an increasing waist circumference and body fat percentage [31]. Another study included presented a prevalence of 66% of caregivers with elevated waist circumference, according with WHO cut off points [35]. Therefore, although more studies are needed to explore the impact of caregiving in these indicators, it seems that caregiving is associated with higher adiposity.
Furthermore, weight changes after becoming caregivers were also assessed in six studies but the percentage values of either weight gain or loss were inconsistent within studies, which is explainable by the different criteria that was used, since studies established a cutoff- point: two of them considered an increase/decrease of at least 4,5 kg [23-30], another considered losing three or more kg [29] and another considered gaining more than 20% of their weight/losing more than 5% of their weight [24]. The remaining two articles didn’t specify their criteria of weight change. Malnutrition considering MNA and frailty were also evaluated in two articles. However, only of two of the five articles included that studied samples with older participants used tools to screen these characteristics. The obtained results were discrepant, with one of the samples having almost the double of caregivers malnourished or at risk of malnutrition than the other - 33,3% [30] vs 64,4% [29]. The main reason that may be behind this discrepancy is the type of care receipt. Caregivers of both articles were taking care of their elderly spouses. However, the ones belonging to the study with higher percentage of people without a normal nutritional status, were taking care of people with Alzheimer’s disease, having has a bigger impact on caregivers’ nutritional status [29], perhaps due to the great challenge posed to the caregiver. Nevertheless, all these values of caregivers’ malnutrition/risk of malnutrition are problematic and it’s crucial to supervise older caregivers’ nutritional status. Regarding frailty studied in 1 article, only 35,9% of caregivers were non-frail and it turns out there was a significant worsen frailty status throughout the time of 36% of the whole sample of caregivers [30]. This information is a red flag not only for the caregivers themselves but also to the people they’re taking care of, since frailty is associated with many negative health outcomes that interfere with caregiving performance, such as a higher chance of hospitalization and greater risk of physical handicaps [45]. Lastly, even though caregiving wasn’t associated with a worse diet in this review, the articles included shown that fruit and vegetable consumption was inadequate, and caregivers didn’t meet American recommendations of 6 nutrients. Having a nutritionally adequate diet pattern, not only is vital to better health outcomes, but is also a form of health-promoting self-care. As such, it is important to promote healthier diet habits within caregivers [27].
In this systematic review, five factors related to caregivers’ nutritional status were reported: sex (1/18 articles), age (4/18 articles), educational level (1/18 articles), caregiving intensity (1/18 articles) and combining caregiving activities with a part-time/full-time job (1/18 articles). Regarding sex, one study found that higher adiposity was associated with female caregivers, but not with male caregivers, which may have happened because most caregivers are usually women [31]. Concerning the three articles that studied age as a factor, two of them noticed an association of younger ages (less than 44 or 40 years-old) with higher parameters of adiposity [25-35]. On the other hand, another study found a negative correlation between caregivers’ MNA score and age, which means that older caregivers where more susceptible to malnutrition, which goes in line with what’s descript in literature regarding malnutrition and age for the over whole population [29]. Concerning level education, lower educational levels were associated with worse nutrition outcomes in two studies, concretely less educated caregivers presented minor MNA scores and had an enhanced risk of excessive weight gain [29-35]. These results are corroborated by a previously meta-analysis that found that malnutrition was associated with lower education levels in older adults [46]. Respecting the frequency of caregiving work, caregivers who have a higher caregiving intensity and those who cared for someone whose disease impacted on their usual daily activities were considered an overweight and obesity group risk, possibly since they have less time to cook healthy food and to exercise [18-35].
Lastly, combining caregiving with a job also had a nutritional impact on caregivers, concretely males that had a part-time job and younger and older females with a full-time job, had higher values of adiposity, perhaps because of the difficulty of balancing work-caregiving activities [31]. This systematic review has also some limitations. Firstly, there are few studies that address the theme of informal and formal caregivers’ nutritional status, which makes it difficult to extrapolate results with confidence. Secondly, 12 of the 18 studies were conducted in United States of America, which may reduce the geographic representativeness of the obtained results. Thirdly, 77,8% (n=14) of the reviewed articles were cross-sectional, meaning that, in these studies it is not possible to identify, in a concrete way, a cause-effect relationship. As such, it is considered mandatory to conduct more studies (particularly prospective studies) focused in this thematic in order to increase the level of evidence. Finally, it’s important to mention that three out of the 18 reviewed studies didn’t take into consideration common cofounding variables, such as sociodemographic characteristics (namely age, sex, ethnicity, highest educational level, income and marital status), general health indicators and behavioral risk factors. As for as we know, no systematic review has yet been written with the aim systematize the existing information relating to informal and formal caregivers’ nutritional status. As such, this is the first systematic review that addresses this important matter. The quality of the reviewed studies is also a strength as cross-sectional studies, cohort studies and the case-control study had a good and consistent quality score mean ± standard deviation (correspondingly: 5,00 ± 1,31; 5,67 ± 0,47; and 5,00 ± 0,00).
Ten different types of methodology were used to assess the nutritional status of caregivers, in this systematic review, such as: Body Mass Index (BMI), waist circumference, body fat percentage, auto reported weight fluctuation, Cancer Survivor Web-Based Needs Assessment Survey (CS-WEBS), Mini Nutritional Assessment (MNA), Fried Frailty Phenotype, Healthy Eating Index (HEI), Health-Promoting Lifestyle Questionnaire II and Australian fruit and vegetable consumption guidelines. Of these, the one that was mostly used was BMI. Regarding caregivers’ nutritional status, not enough evidence of the direct impact of being a caregiver on their nutritional status was found, however it appears to exist a high prevalence of excessive weight, malnutrition, frailty and diet inadequacy in caregivers. Sex, age, educational level, caregiving intensity and combining caregiving activities with a part-time/full-time job were the factors most described in this review as related to caregivers’ nutritional status.
The authors report no conflicts of interest.
None.
The authors’ responsibilities were as follows—FC, BT and CA designed the research and drafted the manuscript; FC, BT and CA conducted the research; FC, BT and CA analysed data; FC wrote this paper and had primary responsibility for final content; BT and CA reviewed and edited the paper. All authors have read and approved the manuscript.


