Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
K Suresh*
Received: April 10, 2023; Published: April 27, 2023
*Corresponding author: Suresh Kishanrao, Public Health Consultant, Bengaluru & Visiting Professor-MPH, KSRDPRU, Gadag, India
DOI: 10.26717/BJSTR.2023.50.007893
Headaches, medially known as cephalalgia, is one of the most common disorders of the nervous system. Approximately half of all adults have had a headache during the past year, and it is the sixth cause of disability in the world. It is the most disabling conditions and can have a substantial impact on quality of life of those affected. If it occurs repeatedly, it may be called as headache disorder. The latest International Classification of Headache Disorders has broadly classified headache disorders into primary and secondary based on their origin. Primary headache the subject of this paper is triggered by lifestyle factors, like alcohol, particularly red wine, processed meats that contain nitrates, changes in sleep or lack of sleep, poor posture, skipped meals & stress. Majority of those with headache have primary headache disorder especially migraine, tension-type headache, and medication-overuse headache. The tension-type headache (TTH), episodic TTH of less than 15 days/month, is reported by more than 70% in some populations. Stress is one of the main aggravating factors across geographies, more so in millennials and females. The Global Burden of Disease Study 2019 estimated that migraine caused 41.1 million YLDs 5.4% of Total YLDs, and tensiontype headache 5.5 million years of life lived with disability. Headache disorders are most troublesome in the productive years of life with lost working days and reduced productivity. Without proper treatment, can become chronic or recurring affecting the well-being of an individual and predispose them to other illnesses.
Self-care with simple analgesics in managing primary headache disorders can help reduce frequency of attack and severity with positive effect on physical symptoms and functional capacity. Paracetamol (acetaminophen) is a safe analgesic with good gastrointestinal tolerance and is first line option. Caffeine’s anti-nociception enhancing effect when given with acetaminophen significantly improves efficacy over use of paracetamol alone. Ninety percent of headaches seen in practice are due to a primary headache disorder where there are no confirmatory tests, and neuroimaging studies, if done, are normal. In this review use of a logarithm is suggested that makes first an emphasis on the recognition of red flags that help in the identification of secondary headaches, referral or management and expects establishing good referral mechanisms in the health system. This also emphasises most importantly a good history taking that allows the physician to recognize a pattern that in turn leads to the correct diagnosis for better management. A comprehensive history needs time, interest, focus and establishment of rapport with the patient. When to ask what question to elicit which information, is an art that is acquired by practice and improves with experience.
Methods & Materials: This review is based on eight case studies of various types of headaches, and literature review and a logarithm suggested by Physicians Association of India and Neurologists Association of India
Keywords: Headache; Cephalgia; Migraine; TTH; Cluster Headache; Nummular Headache; Burden; Health System and Public Health
Abbreviations: TTH: Tension-Type Headache; MRI: Magnetic Resonance Imaging; CGH: Cervicogenic Headaches; CT: Computed Tomography; EEG: Electroencephalogram
Headache is one of the most common, painful, and disabling conditions that affects people of all ages worldwide and can have a substantial impact on quality of life of those affected. Known as Cephalgia in medical terminology, if it occurs repeatedly, it may be called as headache or Cephalgia disorder [1]. The latest International Classification of Headache Disorders has broadly classified headache disorders into primary and secondary based on their origin. Primary headache disorders include migraine, trigeminal autonomic cephalgia, tension-type headache, and other primary headache disorders [2]. Primary headache the subject of this paper, is usually triggered by lifestyle factors, like alcohol, particularly red wine, processed meats that contain nitrates, changes in sleep or lack of sleep, poor posture. Skipped meals & Stress. The most common primary headache disorder is tension-type headache (TTH), episodic TTH, of less than 15 days per month, is reported by more than 70% of some populations. Stress is one of the main aggravating factors for headache across geographies, more so in millennials and females. Majority of those with headache have primary headache disorder especially migraine, tension-type headache, and medication-overuse headache [2]. Headache disorders were the cause of 46.6 million YLDs globally in 2019, 5.4% of total YLDs, with 88.2% of these attributable to migraine [1]. Headache disorders in 2019 ranked 14th among global causes of DALYs for all ages and both genders. In terms of lost healthy life, that equates to 46.6 million people dying one year early.
In the ranked causes of YLDs, headache disorders (602.5 per 100,000 person/years) were third, below low back pain (823.0) and, by a tiny margin, depressive orders (605.7). Among females, gynaecological diseases (second: 764.0) contributed more than headache (third: 751.0) and depressive disorders (fourth: 743.7) despite their clearly evident association with female gender. The association of headache disorders with young adulthood was disturbing. In all young adults, headache disorders (813.4) were top cause of YLDs, whereas among females aged 15–49 years, headache disorders (1016.1) were second only to gynaecological diseases (1230.5), with depressive disorders third (890.4) [1]. Headache disorders were fourth in South Asia and in sub-Saharan Africa, third cause of YLDs in East Asia & Pacific and in Middle East & North Africa, but second in Europe & Central Asia, fifth in Latin America & Caribbean and sixth in North America [1]. A recent meta-analysis of 357 publications, mostly from high-income countries, estimated global prevalence of active headache disorder as 52.0%, of which migraine was 14.0%, TTH 26.0% and of H15+ 4.6%. These estimates were comparable with those of migraine and TTH in GBD2019, the most recent iteration, but higher for headache overall. Each day, 15.8% of the world’s population had headache. Methodological factors like publication year, sample size, inclusion of probable diagnoses, sub-population sampling method, screening question and scope of enquiry (headache disorders only or multiple other conditions) contribute to variation [3]. With these considerations migraine prevalence estimates increased over the years, while estimates for all headache types varied between world regions [1-3].
Limited data available in India support such high burden despite a high diagnostic and treatment gaps for headache disorders in India and many developing countries. The Global Burden of Disease Study 2019 estimated the crude DALY rate of 606 (104-1331) per 100000 population country. The overall cumulative and by gender prevalence in 2019 is indicated in the following (Table 1) [1] Based on a recent epidemiological study to estimate headache burden in the national capital region of Delhi involving rural and urban areas, the 1-yr prevalence of migraine was estimated to be 27.2% (personal communication). Other small studies indicate that primary headaches are at least as prevalent in India as in the West, or maybe more, and better epidemiological data are needed for the correct estimation of the disease burden. Applying the current estimates to population of India, of around 1400 million, and an adult population (65%) of 850 million the absolute numbers of people with 1 year headache prevalence works out to 300 million of TTH, 212 million of Migraines and 25.5 million of daily chronic headaches, look formidable and staggering [4]. In a study from Bengaluru, out of 2050 subjects, 464 patients suffered from tension type headache. Overall prevalence of tension type headache was 22.6%. Prevalence was higher in females (57.9%) as compared to males (42.1%). The headache experienced by majority of the student population was unilateral (31.4%), pulsating type (51.6%) and of moderate intensity (77.1%). Common associated symptoms were nausea associated with other factors (40%) and photophobia and phonophobia (18.6%).
Stress (72.1%) and decreased sleep (49.4%) were the most common triggering factors [5]. The practice of self-medication was reported by 80.2% of subjects. This study noted a high frequency of trigger factors in medical professionals, the most common triggering factors being stress and disturbed sleep [6]. Another study from Urban Kolkata, 1-year prevalence of primary headaches and migraine were estimated to be 14.9 % and 14.1% respectively. Overall DALY was much higher in women as compared to men per 100000 (7209 versus 2140) and highest in women in the age group of 30-34 year. Another door-to-door survey, 2,329 biologically unrelated adults (aged 18–65 years) randomly sampled from urban (n = 1,226) and rural (n = 1,103) areas in and around Bangalore points to an observed 1-year prevalence of any headache as 63.9 %, with a female: Male 4:3. The age-standardised 1 year prevalence of migraine was 25.2 %; higher among females than males (OR: 2.1 [1.7-2.6]) and among rural Population than urban (OR = 1.5 [1.3-1.8]). The age-standardized 1 year prevalence of TTH was 35.1 %, higher among younger people. The estimated prevalence of all headaches on ≥15 days/month was 3.0 %; pMOH was 1.2 %, five-times greater among females than males and with a rural preponderance. About 25% participants with headache in last one year had a contact with a healthcare provider and of those, 30.3% with migraine had consulted, 84.0% of these in primary care. Primary care providers were the most important source of treatment for headaches except those with headache on ≥15 days/ month.
Among Headache >15 days almost half of them had gone to a specialist doctor [6]. This indicates that there is a large diagnostic and treatment gap for headaches which need to be corrected by re-organizing our health services, if we are to reduce the burden of headache on society [7]. Two more rural studies in West Bengal with a sample of 37286 and 20842 reported a mean migraine rate of 1.37% (with a prevalence ration 0.93 in men and 1.64% in women) in 1996 and 4.17% in 2003 [7]. From the point of view of managing headaches by individual doctors and in smaller settings lack of standard treatment protocols are the key challenges. It was only in 2016 that test protocols are proposed by some organization and are yet to be field tested and agree upon [8,9]. This article is based on personal and professional colleagues’ experiences of managing headaches at primary and secondary facilities and by individual practitioners including Indian Systems of Medicines (AYUSH). Review of literature on management practices, and the recently developed Algorithmic protocols. The article primarily approaches the issue from the point of management of headaches in smaller settings, therefore it discusses primary and secondary headaches among common categories of people approaching the health care providers like headaches in adults, children, elderly, pregnant women, cervicogenic and atypical headaches. It also documents epidemiological and economic burden due to headaches and suggests a public health approach to address headache disorders for India Major challenges in addressing headache disorders effectively in India are low perceived severity, absence of burden data, lack of standard treatment protocols for headache disorders and primary care models for neurological disorders in developing country context. There needs to be a better appreciation of the burden and a public health approach among all stakeholders, if burden of headache disorders is to be addressed effectively in India [10].
A Case of Migraine Accentuated by TTH
Bhargavi an young lady in her early thirties, with a daughter, happily married known to have migraine once in 2-3 months approaches on18 March 2023, a local physician with severe headache for over 15 days, following a minor scuffle in the family and frustration of not conceiving for the second time for last 3-4 months as couple desired. The physician after physical examination and battery of blood tests and Xray skull daises it as Sever migraine and prescribed Flumarin10 (Flunarizine Hydrochloride 10 mg, protects against ICH by reducing brain injury, cell apoptosis and the activation of P13K AKT pathway) once a day in the night and Migrest (a combination of Domperidone, that helps in relieving nausea and vomiting & Paracetamol an analgesic) twice a day both in the morning and night for one month. Both drugs are used for reducing the frequency and intensity of the pain on regular use [11]. They are not useful once there is headache in alleviating the ache. Though the intensity has decreased after a week’s use and the patient is under observation. In this case migraine was accentuated due the family tension the lady was undergoing (TTH)
Migraine & Yoga
A 38-year-old married Hindu female housewife suffered from Migraine since 8 to 9 years visited Yoga & Naturopathy OPD Headquarter, Janakpuri New Delhi with the complaints of headache, nausea and dizziness. She had recurrent attacks of headache each with duration of 4 -5 hours to 3 days. She was having low blood pressure and depression problem from last two years due to some family problem [12]. On examination her Blood Pressure was 90/70 mmHg and weight 62 Kg. She was on medication for Migraine and Low Blood Pressure. According to her pain was aggravating by routine physical activity and sometimes accompanied by nausea or vomiting. She was put on yoga therapy session of one hour for 6 days per week for twenty-One days including loosening exercises, Asanas, pranayama’s, meditation and Kriyas and with that he followed proper diet and naturopathy treatment as prescribed. {(pdf) case study on patient with migraine. There was a significant decrease in headache activity, medication score, symptoms, and stress perception. Deep breathing exercises relieved stress and anxiety by balancing stress hormones and eating whole grains and fresh fruits and vegetables helped in reducing frequency of migraine. {(Pdf) case study on patient with migraine. (Siddappa Naragatti [6]).
A Migraine with Aura
A young unmarried women of 22 years cam to me in early 2022 with complaints of headache since menarche at the age of 13 years. Headache appeared 1or 2 times a month lasting for about 6-9 hrs. Scintillating scotoma in her left eye preceding headache every time. The visual changes lasted for about 30-45 minutes followed by hemicranial throbbing headache. Making her to doubt that she may have some tumour in the brain. After an eye examination by an ophthalmologist, and ruling out eye problems causing visual symptoms, a Head CT scan and a Magnetic resonance imaging (MRI), she was put on Beta blockers PNOL 40 Tablets (Propranolol HCL 40 mg) and Chlorpromazine tablet 10 mg per day for 2 weeks and followup with Chlorpromazine around her periods relieved her of the episodes over 3 months’ time. She was trained about Biofeedback and other forms of relaxation training to deal with stressful situations, following a sleeping and eating routine (Don’t sleep too much or too little). And try to eat meals at the same time every day and drink plenty of fluids helped her to get complete relief after 6 months.
Chronic Migraine in a Young Boy
A 10 yr. old boy suffering from CHRONIC MIGRAINE reported along with his parents. He was suffering from headache at interval of three days for 2½ yrs. The nature of headache was gradual increase with severe intensity within an hour & gradual decline, Location of ache was around eye and forehead, Lt. side, throbbing in nature, squeezing pain, lightening pain. There was no Aura but drowsiness with dark circles around eyes 2 hours before pain. Other symptoms included hyperacidity- burning sensation in chest & abdomen, before and after sleep and spicy food consumption. His obesity was for 4 years. He also had pain in both at heels while resting that decreased on standing, Running, or pressing. There was pain in entire spine after a fall on lumbar region, that occasionally comes & goes. He also had Myopia, for 2 years, used spectacles. His allopathic treatment of painkillers and antiemetics during the episodes had not helped him much except temporary relief [13]. on examination the young boy, was very obese with a large belly and fair complexioned. His chubby cheeks covered most of the facial area hiding his eyes. He had a broad forehead and dense hair. Homeopathic treatment with SARSAPARILLA 30 for 5 months did not help. Hence re-evaluation was done talking to his mother. She revealed his state of mind during the attack of pain as he got very angry during the pain. He could not bear the slightest noise or anybody stepping inside his room. Normally, he was afraid of his father, but when in pain, he even screamed at him without any fear. His face turns red hot when angry. His headache was diagnosed due to violent anger, he was put on CHAMOMILLA 30 (chamomilla 30x tablets contain chamomilla for assisting with occasional sleeplessness and irritability). Next week his father rang up & informed that he was feeling better and requested the medicine by courier, and the same continued till May 2006. CHAMOMILLA 30 was continued, and he was to avoid Sun exposure during summer. They returned for consultation when he had a slight headache after 1½ yrs. He had no attack of headache during this whole period. His backache and hyperacidity were reduced considerably. This case demonstrates the need for taking history of symptoms like thermal, miasm during an attack, (Excess anger in this case) so that the correct Similimum becomes clear.
Autobiography of First Attack of Sinusitis Headache
Way back in 1963 when I was a first year MBBS student, once in the winter of Dharwad a known cooler place than I had grown up until then, I had headache following common cold, for over 8 days. It used to be heavy in the morning and as the day progressed reduce but not completely relieved. After a week I consulted the ENT professor who diagnosed it as acute sinusitis and did an antrum wash and put me on antibiotics for 5 days. I got complete relief, but I used to get such attacks almost every year for about 5 years I was there. After joining health services in a district with much warmer climate, I was completely relieved of sinusitis related headache.
Atypical Headaches
A 37-year-old male, who presented to me a family medicine practitioner in July 2019 with persistent headaches which subsided postprandial and was later hospitalized for stroke-like symptoms for 6 weeks. The LP suggested viral aetiology; however, CSF yielded no evidence of a specific virus. The patient’s computed tomography (CT) was non-diagnostic and magnetic resonance imaging (MRI) confirmed no acute intracranial abnormalities. Electroencephalogram (EEG) showed no definite epileptiform discharges, electrographic seizures, or evidence of non-convulsive status epilepticus. He was started empirically on intravenous (IV) acyclovir 800 mg Q6 for 10 days, followed by another 10 days of oral valacyclovir 500 mg twice a day (BID) antiviral leading to a complete resolution of his symptoms and confirming the diagnosis as viral encephalitis. This case is unique in its presentation due to the postprandial resolution of the patient’s headache with no evidence of a specific virus in the CSF. In primary care setting, insidious causes for a headache, such as viral infections, should be ruled out by an empirical treatment and don’t be in a hurry to refer to a neurologist for management.
Tension-Type Headache (TTH)
1. This is a report of a 50-year-old female patient complaining
of a constant dull headache, all day for nearly a year. A detailed
history and her occupational details indicated that she was promoted
a year ago as an office superintendent involving oversight of pool of
a dozen typists and timely put-up responses to assembly questions
of the Department of Health and Family Welfare. Her seat did not
ergonomically suit her short nature, being tall she had to bend her
back and neck for about 6-8 hours a day. A physiotherapist evaluated
the patient and found active trigger points in her cervical muscles.
Then, she received Positional Release Therapy for her trigger points.
After 3 treatment sessions, the patient’s headache stopped completely.
During the 8 months following the treatment she was without pain
and did not use any medication. Positional Release Therapy could be
an alternative treatment to medication in patients with T.T.H.
2. A 33-year-old rural male presented to my clinic complaining
of headaches. The patient described the headaches as dull, achy, and
occasionally throbbing’ in quality. The intensity of pain was 4.5/10
on a visual analogue scale (VAS). There were no sensory or motor
phenomena, and no visual or hearing disturbances. The headaches
were intermittent, and detailed questioning failed to identify any
daily pattern. Typically, a headache would last for between one and
two hours, with a frequency of two to three episodes per week. Loud noise, and work stresses were aggravating factors, while rest and
self-prescribed paracetamol (2 tabs 500mg) generally relieved the
episode.
Headache in Covid 19 Patients
Headache, has been a commonly reported symptoms of coronavirus disease-2019 (COVID-19) illness since late 2019 across the world. In our apartment complex out of 34 cases over a period of 1 year (June2020-May 2021) 18 (62%) men, with an average of 57 reported headache. We found that younger people and those with fewer comorbidities did not develop a headache. 50% of headache cases were associated with low levels of C-reactive protein. Pharyngitis, loss of taste, joint pain, and nausea were common in patients with headaches. We experienced migraines and tension-type headaches were the most prevalent.
Based on me and my friends experience in approaching headache a primary care doctor in general must follow 3 Key steps [9,10]:
Evaluate & Diagnose Headache by History & Physical Examination
History Must Include:
1. When did the headaches start?
2. How long have the headaches been happening?
3. How often do they happen?
4. What triggers the headaches? certain foods, situations,
physical activity, or medications cause?
5. Who else in the family has headaches?
6. Any notable symptoms between headaches? - weakness,
changes in vision or loss of consciousness?
7. Are the headaches keeping a person from missing work? Are
they bothering while on work?
8. How are the headaches affecting quality of life? - spend a lot
of time in bed? miss out on meeting friends?
9. Where is the pain located? What does the pain feel like? How
long does the pain last? What makes the pain feel better?
10. What time of day/he gets a headache? Do the headaches
happen suddenly?
11. Is there an aura before the headache? experience changes
in visions or blind spots? Do they see bright lights or experience
numbness/ tingling?
12. Any decreased appetite and changes in attitude or behaviour
and
13. What treatments have you tried at home? Medication? Ice
packs? Turn the lights off in the house, etc.?
Physical Examination: Check for Fever, tenderness over sinuses,
High blood pressure, Muscle weakness, Balancing problems, Vision
problems, Rhinitis, or common cold and ear infections and postural
problems due cochlear damages/implantation
Look for Red Flag Signs for Urgent Need for Referral- Identify Referral Pathways
It is important to identify the care pathways for referral to higher centres in case a headache sufferer has ominous symptoms and signs or becomes refractory to the treatments offered at the primary level. Red flag signs for immediate referral include Thunderclap onset, Signs of Meningism, Papilledema with focal signs, acute Glaucoma. Similarly, Elderly with cognitive changes, Papilledema with no focal signs, or any relevant systemic infections - sinusitis, Urethritis etc. Indian Health system needs strengthening Referral system at all levels with trained human resources and appropriate diagnostic and treatment technologies and medicines.
Check if it is Secondary Headache and Treat the Cause
e.g., Sinusitis, Refractory errors, other infections etc.
Classify & Treat Primary Causes by Age & Gender- Identify Treatment Pathways
Management of Migraine: NSAIDS (Ibuprofen, Paracetamol), Ergots (Migranal, Trudhesa Triptans (El triptan 40- mg dose).
Management of TTH: NSAIDs, Ana Tensol, Chlorpromazine,
Counselling.
Management of Cluster Headache: Intranasal or Subcutaneous
Triptans.
Management of Trigeminal Neuralgia: Intranasal or
Subcutaneous Triptans.
Management of overuse/abuse of Medications: Gradual
withdrawal, Analgesics, Barbiturates.
Choose Management (Referral/ Treatment) Pathways (Annexures 1 & 2)
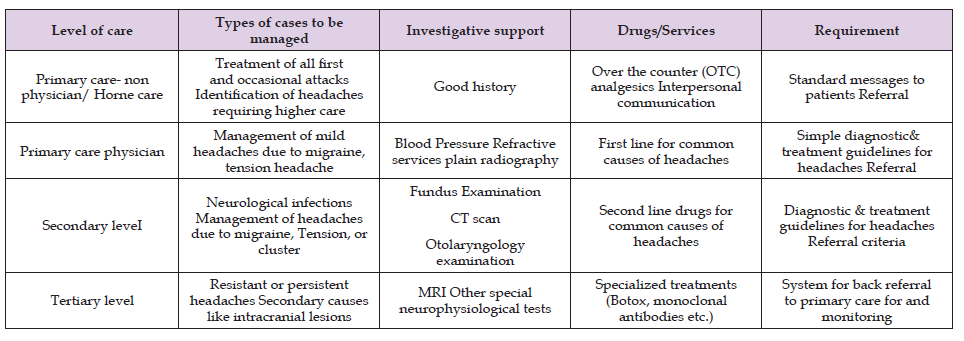
Both Logarithms help approaching headaches in primary and secondary set up. The first step involved is identifying if it is secondary to known causes listed in the recent international classicisation of headaches (Table 1) and either treat or refer depending upon the status. For example, a Sinusitis case may respond to antibiotics in the initial stages but the same may need antrum wash by an ENT specialist. Refractory errors following testing using Snellen’s chart may need to be referred straight away (Table 2) [9,10]. Second step involves identifying the type of Primary headaches. The table below with characteristics etc would help in differentiating the common primary headaches [3]. In differential diagnosis between headaches of Overvoltage, Migraine, Arterial Hypertension, Ischemic stroke, and Low blood pressure (Table 3) [9].
Table 2. List of Headache Disorders - The International Classification of Headache Disorders, 3rd Edition Issued by International Headache Society [3].
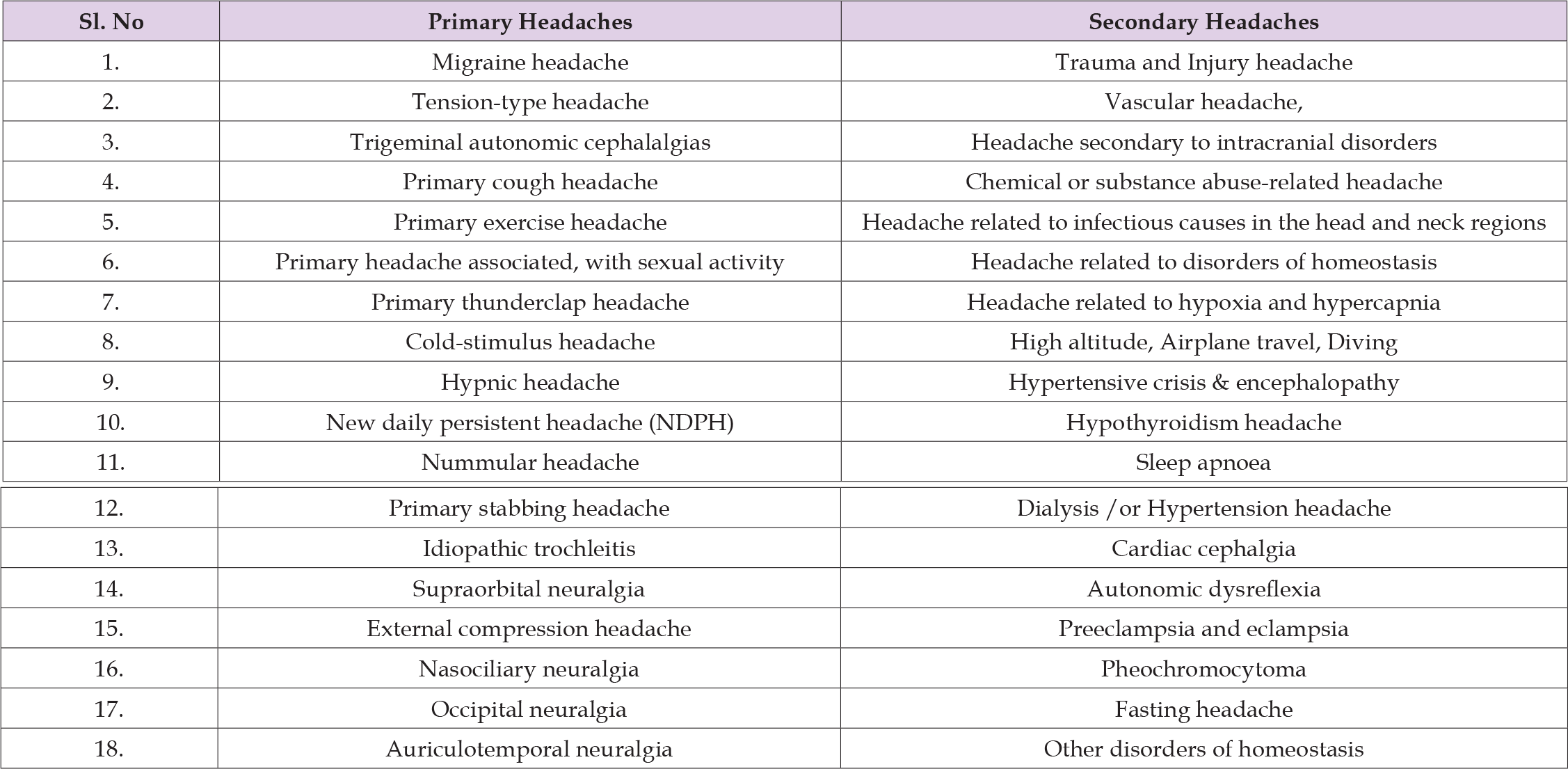
Table 4. The Following Table Depicts the Level at Which and by What Means Headaches Can be Managed [9,10].
Headaches in Adult Population
The most common primary headache disorder in India is tensiontype headache (TTH). Episodic TTH, <15 days per month, is reported by more than 70% of some populations. Stress is a common trigger. Migraines is the second common cause of headache, it first occurs during adolescence, tend to peak by 30s, and gradually become less severe and less frequent in the following decades. The Women suffer more than Men, the ratio being 3:1. Both types are a common symptom of different types of anxiety, inability to control anxiety and constantly worrying nature (Table 4). They are triggered by lifestyle factors like- Changes in sleep or lack of sleep, Poor posture, skipped meals and Stress and Alcohol, particularly red wine, processed meats that contain nitrates [6,10]. From one of the recent studies in Delhi, nearly 300 million tension type headaches,215 million Migraines and another 25 million chronic daily type headaches are projected each year. Bengaluru study reported a practice of self-medication by 80.2% of subjects and less than 20% sought care, of them 80% went primary care doctors and rest went to a neurologist (Figure 1).
Cervicogenic Headaches (CGH)
Cervicogenic headaches (CGH) are defined by the International Headache Society as “pain, referred from a source in the neck and perceived in one or more regions in the head and or face.” About 15 to 25% of all headaches are secondary headaches with causations in the cervical spine. In India the prevalence of CGH is 4%, the exact causative mechanism for CGH remains unclear. The positional default position of the atlas is a contributing factor to CGH. The upright position in humans results in a vertical gravitational compressive force in the cervical spine due to the head’s weight. Over time these forces result in progressive degenerative changes, cause motion restriction and pain [14]. Degenerative changes will result in abnormal muscle tone, that affect the positional relationship between cervical vertebrae, & lead to abnormal cervical motion patterns. It has been demonstrated that there is a direct connection between the trigeminal nerve (cranial nerve V) to the face and head & the spinal nerves of the first three vertebrae through the trigeminocervical nucleus. A current study is underway to determine if muscle strength and tone of suboccipital muscles controlling the position and movement of the atlas can be retrained /normalised, it will significantly change the management of those suffering from cervicogenic headaches [15].
Geriatric Headaches
Older people have fewer headaches than younger ones, and women have more headaches than men through their lives. After age 75, the prevalence drops to 55% women and 21% in men, respectively [16].
Cerebrovascular Disease: Headaches commonly accompany stroke. A study of 163 patients who’d had a stroke, 60% reported a headache with the stroke, especially women and those with a history of headaches. Up to 46% reported having an incapacitating headache; most said the headache was mild to moderately painful. The headaches are equally likely to come on quickly or slowly.
Head Trauma: Falling due to inability of balancing is a particular problem, about 30% of people ages 65 and older fall at least once a year. If the person has dementia, they might not remember having fallen. Headaches are present in up to 90% of patients with head trauma, including subdural hematomas. The headaches can range from mild to severe, can be intermittent or constant, and can happen on one or both sides of the head. Coughing, straining, or exercise can make them worse, and sometimes there’s vomiting and nausea.
Temporal Arteritis: Headaches are the most common symptom of temporal (giant cell) arteritis (TA).
Trigeminal Neuralgia: The condition is more common in people older than age 50 and is seen more in women than men. When there is pressure on the trigeminal nerve, which controls facial feeling, it can cause excruciating pain in the lower part of the face, around the nose, and above the eye. It is triggered by brushing your teeth, chewing, or blowing nose. Anticonvulsants -carbamazepine are the drugs of choice. About 30% of people don’t respond to medication but may respond to surgery.
Postherpetic Neuralgia: Postherpetic neuralgia is nerve pain that lingers after shingles, a rash also known as herpes zoster Shingles has the same origin as chickenpox, caused as it is by the varicella virus. It is characterized by sores that form and crust over 3 to 4 weeks. It can cause nerve damage that leads to burning, shooting, and tingling pain for 3 months or longer. The persistence of pain from shingles is more common among people older than age 80. Shingles involving the face nearly doubles the risk of developing facial postherpetic neuralgia. Treatment includes anticonvulsants, antidepressants, aspirin, NSAIDs, and creams.
A rare disorder that occurs in 40 to 79 age cohorts. Diagnosed after ruling out drug withdrawal, temporal arteritis, sleep apnoea, brain trauma, migraines, and other causes. The headache (on one or both sides) occurs only during sleep and awakens a person at a consistent time. It can throb or not, be from mild to severe. They typically last for 2-3 hours nightly for years. Treatment includes caffeine pills before bed or a one or two cups of coffee, lithium carbonate, indomethacin, atenolol, melatonin, cyclobenzaprine, or prednisone.
Headaches During Pregnancy
a woman prone to get headaches, pregnancy can make the problem
worse. Headaches in pregnancy are probably caused by hormones,
and changes in the way your blood circulates. Common causes include:
1. Giving up caffeine,
2. Fatigue
3. Sinus Congestion
4. High Blood (Pregnancy induced hypertension)-PIH-initial
stage
5. Stress and Hunger
6. Too Much Exposure to The Sun And
7. Dehydration
8. On rare occasions, headaches could mean pre-eclampsia.
However, of women who usually suffer from migraines, some
either have less trouble with and others find these painful
episodes becoming more frequent and intense when pregnant.
Management: Simple analgesic and work out on triggers. Paracetamol, is considered safe for occasion but aspirin and ibuprofen, are not recommended. PIH need to manage with drugs.
Compresses: A warm compress around your eyes and nose for sinus / a cool compress at the base of your neck for TTH. Steam Inhalation is beneficial for a cold and stuffy nose (2 drops of peppermint or eucalyptus oil/Vicks added).
Avoiding Sun: When t in the sun, it is advised use an umbrella or dupatta to cover your head and dark glasses to protect your eyes from the glare. Keeping hydrated well-Drink lots of water to keep yourself hydrated as well.
Massage: Massage works especially well on tension headaches, which build in the neck, shoulder, and back muscles. Eat little and often: Low blood sugar is a common cause of headaches. Try eating smaller, more frequent meals.
Stay Active: Regular exercise can reduce the frequency and severity of migraines. A walk / a dip in the swimming pool once a day. Get eyes tested for refractive errors: Sometimes pregnancy may affect your vision, causing headaches.
Taking a Cold Shower/ Splash Cool Water on Face: It works by constricting the dilated blood vessels in the head to bring fast, relief other alternative Indian system treatments- green colour therapy, Yoga, Pranayama & Taking a break (small nap) to address fatigue and exhaustion [17].
Headaches in Children
Most parents seek care only when a headache wakes their child
from sleep or is more frequent or changes behaviour or personality.
Headaches happen to 25% of younger children & 75% of adolescents.
Among children between 5 and 17 years of age, 20% report headaches
TTH - (15%) and migraines (5%). Children’s headaches often don’t
last as long (2-72 hours), Children feel the pain all over their head,
instead of just one side or section & Children C/O abdominal pain,
vomiting and nausea. Simple illnesses like the flu, an infection or a
fever, Sinus infection, Sore throat, Ear infections, Head trauma, Stress,
Anxiety, Depression, Tension, Exercising too much, Meningitis, Viral
encephalitis, Haemorrhage, and a Tumour. The red flags of Headaches
that change over time, increase in frequency, weakness and/or loss
of sensation; headache on awakening with or without vomiting;
confusion or difficulty thinking. Headaches that lead to symptoms
like visual changes or loss of vision; slurred speech, problems
moving your arms or legs, loss of balance, confusion, or memory
loss & headache getting worse over 24 hours Most headaches in
children aren’t serious. Two common kinds of headaches that kids
get are tension headaches and migraines. Keeping the child in a cool
place, wet cloth on child’s forehead and rest in a dark, quiet room
will resolve. Paracetamol tablets is enough. A headache in a child
is related to stress (of scholastic performance, going to school or a
particular subject or a teacher), Refractory errors, Sinus infections,
hunger, genetics, hormones, diet, medications, and dehydration
[18]. Recurrent headaches of any type can cause school problems,
behavioural problems, and/or depression. Or Vice versa Sinus
examination & tenderness, MRI (magnetic resonance imaging)
and CT scan (computed tomography) help in diagnosis. Common
management and treatment of headache in children include:
1. Medications: Ibuprofen (Tab. Brufen- 200 mg), (Advilchildren),
Crocin, (Aleve®) and acetaminophen (Tylenol®).
Abortive therapy- at the first sign of a migraine.
2. Headache Education: Headache triggers. Common triggers
education- Lack of sleep, Specific foods, Caffeinated drinks,
Chocolate. Nitrates (meats, ham, bacon, sausage, hot dogs), some
cheeses (tyramine-containing foods, like pizza). MSG-containing
foods.
3. Lifestyle Changes: 8 hours of sleep every night, 6x 250ml of
water every day, Three healthy meals, Cardio exercise (45 min x
3-5 times a week). Relaxation.
4. Stress Management: Deep breathing exercises, Mindfulness
or meditation, Mental imagery relaxation, Music therapy &
Counselling.
5. Recommend - Specialists Consultation: Ophthalmologist
(vision issues), ENT (ear, nose, and throat specialist for balance
problems), Gastroenterologist (for stomach problems),
Psychologist or psychiatrist (for stress and emotions) and
Headache specialist.
Covid 19 Headache
Headache in COVID-19 illness is usually secondary headache due to the infection. A small proportion (20%) of Covid 19 patients may have new onset with no history of headache or may report a significant change in previous headache episodes. Mostly COVID-19 illness precipitated headache episodes like past headache. Headache as the presenting symptom among less than 5% in patients with COVID-19 was detected in the regular screening protocol [6]. The presence of headache as a COVID-19 onset symptom at hospitalization was higher in subjects with the Delta variant than in those infected with the Wuhan or Alpha variants. The prevalence of long COVID-19 headache 6 months after hospital discharge was higher in individuals infected with the Delta variant than in those infected with the Wuhan or Alpha variants, to infer that Headache was a common symptom in both the acute- and post-COVID-19 phase in subjects infected with the Wuhan, Alpha, and Delta variants but mostly in those infected with the Delta variant [9]. Out of 120 COVID-positive cases, 26 (21.66%) reported headache during COVID illness. Out of these, 12 cases reported newonset headache without any history of headache. Fourteen cases had a history of headache Among these 14, 6 cases reported a change in their character of headache from their regular headaches. So overall, secondary headache due to COVID-19 illness was reported in 18 (15%) cases and in other 8 cases, COVID illness precipitated the headache episode of past headache type [19-21]
Nummular Headache
Nummular headache is a chronic primary headache disorder
recognized by the international headache society. Although it is a
benign disorder, in some instances it can be very resistant to treatment
and can cause significant morbidity. Nummular headache is a primary
headache disorder without an identifiable underlying aetiology.
It is not associated with any psychiatric disorders, anxiety, and
depression unlike Migraine or TTH. Migraine and tension headaches
may be concurrently present with a nummular headache but are
not related. Nummular headaches are classified as epicrania, that
include headaches that arise from epicranial tissue such as internal
and external layers of the skull, all the layers of the scalp including
epicranial nerves and arteries. It is characterised by.
1. Mild to moderate head pain
2. Pain is felt only in a rounded and elliptical area of 1-6 cm in
diameter.
3. Pain is chronic and either continuous or interrupted by
spontaneous remissions lasting weeks and months and
4. Not attributable to another disorder.
Treatment includes NSAIDs and analgesics. In resistant cases,
preventative therapy with chemical neuromodulators such as
gabapentin, pregabalin and tricyclic antidepressants TCAs have been
successfully used (Table 5).
Note: Source {3}: Nummular Headache - Muhammad Salman Janjua,
Migraine
Migraine is an episodic disabling headache requiring long-term management. Migraine is very common, affecting one in five women, one in 16 men, and even one in 11 children. Migraine attacks are three times more prevalent in women, likely because of hormonal differences. Certainly, genetic and environmental factors play a role in the development of migraine disease. Migraine management through Yoga therapy & naturopathy would reduce the medication cost with positive health benefits. A case study to evaluate the efficacy of Yoga & naturopathy as an adjuvant therapy in migraine patients by assessing clinical outcome and autonomic functions tests indicated that. is one of the most common and misunderstood diseases encountered in general medical practice. Migraine extracts a significant personal, psychological, social, and economical toll from migraineurs and their families. Recent advances in understanding pathophysiology and acute therapy provide the potential to markedly reduce the impact of migraine.
Tension Type Headaches (TTH)
Tension type headache is one of the most prevalent, primary headaches and a benign neurological disorder. It is also known as’ muscle contraction headache’, ‘stress headache’, or ‘psychomyogenic headache’. TTH has a lifetime prevalence in the general population ranging between 30% and 78% in different studies. They affect approximately 1.4 billion people or 20.8% of the population. International headache Society classification (ICHD II), tension type headaches have been divided into two forms, episodic (ETTH) and chronic (CTTH). ETTH is further divided into wo groups namely infrequent and frequent (second digit classification). All the three types of tension type headaches share similar clinical features except for frequency. Individuals with less than five episodes per month are classified as infrequent episodic TTH which is the most common type of TTH. Only about 3% of individuals would have more than 10 headache days in a month. Nearly 2/3 of the persons have a gradual onset of a headache (64.9%) episode and in terms of timings around 1/3 would have a headache in the afternoon, that can be linked with exposure to sun and skipping of meals. Another quarter may have evening onset headaches due a tiring or unpleasant day at work or schools and colleges. The intensity of headache using the VAS for pain, 3/4 of the individuals would be suffering from moderate pain during the attacks. The common triggering factors include decreased sleep, hunger, irregularity in food intake, excessive work, emotional factors, noise, and reading (Figures 2 & 3).
Environmental and hormonal triggers like, head bath, hot water bath, watching TV/laptop for long hours, flickering lights weather changes, travel and offensive odour also contribute to TTH. The diagnosis of tension type headache is essentially clinical and relies only on symptoms. Thus, a detailed history of taking and through examination is important. Core clinical features required are 2 out of the four, namely-
1. Bilateral in location,
2. Pressing or tightening (non- pulsating, in quality,
3. Mild to moderate intensity and
4. Not aggravated by routine physical activity. Both categories
are unaccompanied by nausea or vomiting and no more than one
episode of photo or phono-phobia after excluding any primary
cause.
TTH Among Professionals (A Case Study Among Medical Students): In a study from Bengaluru, out of 2050 subjects, 464 patients suffered from tension type headache. Overall prevalence of tension type headache was 22.6%. Prevalence was higher in females (57.9%) as compared to males (42.1%). Headache experienced by majority of the student population was unilateral (31.4%), pulsating type (51.6%) and of moderate intensity (77.1%). Common associated symptoms were nausea associated with other factors (40%) and photophobia and phonophobia (18.6%). Stress (72.1%) and decreased sleep (49.4%) were the most common triggering factors. Practice of self-medication was reported by 80.2% of subjects. This study noted a high frequency of trigger factors in medical professionals, the most common triggering factors being stress and disturbed sleep [10]. Gender-wise triggers indicated that while among male top five triggers were stress, excessive work, hunger, decreased sleep and reading. Whereas in women Top 5 triggers were Stress, decreased sleep, emotional factors, excess work and watching TV or mobile phones (Tables 6-8) (Graph 1).
Cluster Headaches
Cluster headaches occur in cyclical patterns or cluster periods. A cluster headache commonly awakens you in the middle of the night with intense pain in or around one eye on one side of your head. They are one of the most painful types of headaches. Other symptoms include one-sided pain, restlessness, excessive tearing, redness of your eye on the affected side, stuffy or runny nose on the affected side, forehead or facial sweating on the affected side, skin pallor or flushing on face, swelling around eye on the affected side, drooping eyelid on the affected side. Bouts of frequent attacks can last from weeks to months, usually followed by remission periods of months and sometimes even years. It is rare and not life-threatening. There’s no cure for cluster headaches. Treatments can make cluster headache attacks shorter and less severe. Injectable Triptans, dihydroergometrine and local anesthetics reduce the number of cluster headaches.
Limited data available in India support high burden despite a high diagnostic and treatment gaps for headache disorders in India. There is a large diagnostic and treatment gap for headaches which need to be corrected by re-organizing our health services, if we are to reduce the burden of headaches on the society. Major challenges in addressing headache disorders effectively in India are low perceived severity, absence of burden data, lack of standard treatment protocols for headache disorders and primary care models for neurological disorders in developing country context. There needs to be a better appreciation of the burden and a public health approach among all stakeholders, if burden of headache disorders is to be addressed effectively in India.


