Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Ahmer Irfan1#, Jeremie MP Lever1#, Connie Shao1, Mona N Fouad3, Margaret I Liang3,4, Daniel I Chu1, J Bart Rose1,3 and Sushanth Reddy1,3*
Received: April 11, 2023; Published: April 26, 2023
*Corresponding author: Sushanth Reddy, Department of Surgery, University of Alabama at Birmingham, BDB505,1720 2nd Avenue South, Birmingham, AL, USA
DOI: 10.26717/BJSTR.2023.50.007890
Background: Telehealth will improve access for underserved patients with cancer who must travel great distances to reach referral medical centers. Disparities exist in resources needed to utilize telehealth. It is not known to what extent technological knowledge may be associated with demographic factors.
Methods: We conducted a cross-sectional survey in surgical, gynecologic, breast, and medical oncology clinics at an NCCN-designated Comprehensive Cancer Center. The five-part survey focused on socioeconomic determinants of health (SEDOH) and technological knowledge. Technological knowledge was measured using a multiple-choice quiz modified from the Student Tool for Technological Literacy (ST2L).
Resulst: Three-hundred-forty-four participants responded (64.3%). The mean age of the respondents was 57.5 years, 70.0% women, 67.3% White, and 25.4% Black. Ninety-six patients (30.0%) did not have adequate internet access for telehealth use, and a 6.5% reported no internet access. Increasing patient age (p<0.001), Black race (p=0.002), East Asian descent (p=0.034), and lack of high-speed internet access (p=0.045), were all associated with worse technological quiz score. Patients with a greater health literacy (p<0.001) and higher education level (College graduate, p<0.02; Graduate school, p<0.001) were both associated with increased technological quiz score.
Conclusions: About one in three respondents did not have adequate internet access for video telehealth.There were significant disparities in knowledge of technology among patients with cancer and these disparities were associated with demographic characteristics. This study provides a foundation for identifying patients that may have barriers to successful utilization of telehealth.
Keywords: Telehealth; Telemedicine; Remote clinical service; Technology; Technological knowledge; Socioeconomic determinants of health
Remote clinical service, or telemedicine, has the potential to greatly expand cancer care. Telemedicine can improve access to specialty providers, create flexibility in scheduling, and decrease healthcare costs. Although telemedicine has been used since the 1960s, its expansion grew exponentially during to the COVID-19 pandemic [1]. This strategy was implemented in our healthcare system to mitigate unnecessary contact between high-risk people [2,3]. As the pandemic is starting to end, evaluation of telemedicine is now underway. Many patients and providers exhibit increased patient satisfaction with remote interactions in select circumstances [4]. It is clear that telemedicine will remain an integral part of cancer care [5]. As we are witnessing telemedicine’s growth, it is imperative that we recognize its limitations. We and others have shown disparities in telemedicine use during the pandemic with decreased telemedicine use by the elderly, Black patients, and economically disadvantaged peoples [6- 8]. Given the dependence on remote technology during the pandemic, there has been great interest in improving internet access as part of infrastructure improvements in the US [9]. However, internet access alone cannot explain telemedicine disparities. Employing social media use as a surrogate for technological access, younger age, Black race, or annual income less than $30,000 are factors associated with increased social media use compared with older. Age, White race, or annual income greater than $75,000, respectively [10].
Therefore, an effective telemedicine delivery model must include all levels of the socioeconomic determinants of health (SEDOH) in the constructs of patient and provider engagement [11]. Telemedicine utilization requires that the subjects demonstrate comfort, basic understanding of functionality, and the ability to use or troubleshoot telemedicine. Our group has previously shown that patient engagement and comfort using health technologies differ by sex, race, and insurance status [12,13]. We therefore sought here to study cancer patient technological knowledge in the context of SEDOH to identify those individuals who might struggle more with telemedicine usage in their care.
Setting
The University of Alabama at Birmingham (UAB) Medical Center is a tertiary referral hospital serving the population of Alabama. We conducted this study in the outpatient cancer clinic setting in the divisions of Surgical Oncology, Medical Oncology, Gynecologic Oncology, and Breast Oncology over the course of 2 months (October to November 2020). All patients attending these clinics were given an anonymous paper survey to prior to their provider in-person visit. Completion was voluntary and participants returned unidentified surveys in secure lockboxes to ensure anonymity. Surveys were collected weekly and transcribed into a secure online database. The UAB Institutional Review Board approved the conduct of this study (IRB-300005711).
Survey
The survey was a multiple-choice, five-part questionnaire. Sections focused on different SEDOH: self-reported demographics, cell phone access, internet access, health literacy, and technological knowledge. Health literacy was determined using the Brief Health Literacy Tool [14]. Technological knowledge was the primary outcome measured and assessed using novel modified questionnaire based on the validated Student Tool for Technology Literacy (ST2L) [15]. The ST2L is a 107-question validated tool is used to gauge technological literacy for middle school students and consists of knowledge assessment items as well as performance-based task items. From the 107-item tool, ten multiple choice questions focusing on general technological knowledge were selected for our modified, brief technological knowledge quiz. A companion study was conducted assessing digital comfort and health literacy as a function of SEDOH in the same survey [13].
Income
Median income was estimated using IRS data for individual zip codes. Alabama statewide median annual income for a four-person household was 48,486 USD. Income level was categorized as being less than or equal to 1x, between 1 and 2x, and greater than or equal to 2x the statewide median income.
Statistical Analysis
Covariates were compared using chi-squared analysis for categorical data and ANOVA for continuous data. Ordered logistic regression was performed to univariable and multivariable analyses to identify covariates statistically related to technological knowledge using STATA [16]. 1 (Stata Corp; College Station, TX) with p-values less than 0.05 accepted as statistically significant.
A total of 534 survey were distributed with 344 returned for analysis (64.4% response rate). The mean age of the respondents was 61 years. Most were female (70.2%) and White (64.1%). Similar to our region’s demographics [16]. 24.3% were Black. The highest education level among patients in the study demonstrated variation; the most common answers were high school with diploma (n = 112, 33.5%), college with degree (n = 93, 27.8%), and college without degree (n = 81, 24.3%). One participant did not attend high school and a number of patients were graduate degree holders (n = 39, 11.7%). The majority of patients had smart phones, with the most common devices being iPhones (n = 171, 51.2%) and Android devices (n = 123, 36.8%). Sixteen participants (4.8%) reported non-smart phone ownership and some patients did not know the type of cell phone they owned (n = 10, 3%). The most common means of internet access were cable-based (n = 174, 52.1%), Digital Subscriber Line (DSL) (n = 50, 15%), and cell phone (n = 35, 10.5%). Of note, 24 patients (7.2%) did not have any access to internet at home (Table 1). The outcome measured was total technological quiz score. 327 (95.1%) of respondents completed the quiz with a mean score of 5.7 questions correct (median 6, interquartile range 3-8) and evenly distributed. The most common score for the quiz was 9 (Figure 1). The question that was least frequently answered correctly (n = 32, 9.8%) was the identification of Trojan as malware (most common answer was virus).
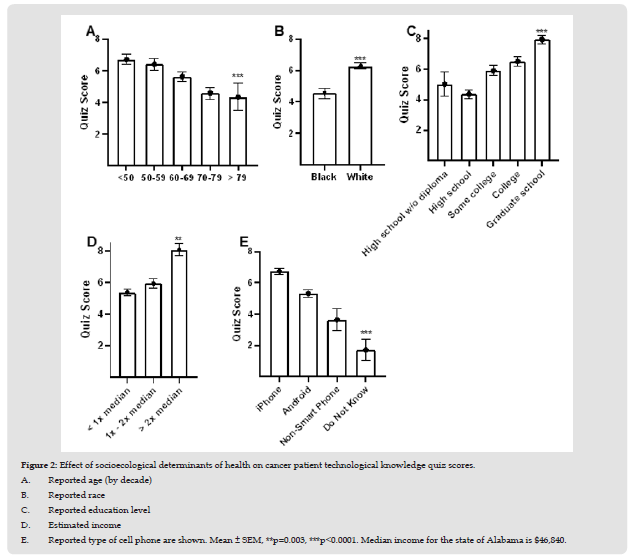
Quiz score was examined in unadjusted analysis with different covariates (Figure 2). A poorer technological knowledge score was associated with increasing age (p < 0.001) (Figure 2A) and black race (p < 0.001) (Figure 2B). Patients who reported a higher level of education (p < 0.001) (Figure 2C), and with an income greater than 2x the national. median (p = 0.003) (Figure 2D) were found to have statistically higher scores. As expected, patients with smartphones had higher technological scores but those patients who did not know the type of phone they used had lower scores (p < 0.001) (Figure 2E). Ordinal logistic regression was performed to determine variables that may be associated with technological knowledge. Mixed model ordinal logistic regression was used to control for multiple demographic variables with quiz score as the dependent outcome. After controlling for demographic variables in multivariable analysis, increasing patient age (p < 0.001), Black race (p = 0.002), East Asian descent (p = 0.034), and lack of high-speed internet access (p = 0.045), were all associated with worse technological quiz score. Patients with a greater health literacy (p < 0.001) and higher education level (College graduate, p < 0.02; Graduate school, p <0.001) were both associated with increased technological quiz score. (Table 2). One of the strongest negative associations of technological knowledge in our analysis was Black race. In comparison to White respondents, Black individuals had similar baseline demographic characteristics and self-reported internet accessibility.
Figure 2 Effect of socioecological determinants of health on cancer patient technological knowledge quiz scores. A. Reported age (by decade) B. Reported race C. Reported education level D. Estimated income E. Reported type of cell phone are shown. Mean ± SEM, **p=0.003, ***p<0.0001. Median income for the state of Alabama is $46,840.
However, White individuals had higher estimated incomes by over $14,000 and 1.7x health literacy scores. (Table 3). The strongest positive association for technological knowledge was increased health literacy. As health literacy improved, respondents were younger (p < 0.001) and more likely to be female (p = 0.014), have a college degree (p < 0.001) and use a smartphone (p = 0.04). (Table 4).
With telemedicine expansion, it is critical to understand which patients may experience difficulty using telemedicine in its current format. The ability to utilize this technological format requires a multidimensional analysis of patients’ telemedicine usage. This is, to our knowledge, the first study evaluating technological knowledge in any patient population. Age, race, education, internet accessibility, and health literacy all were statistically related to technological knowledge. Race is known to be a social construct and there are likely additional factors contributing to the association with this selfreported variable. Our findings clearly demonstrate disparities that will be important in the adoption of widespread telemedicine use. Interestingly, estimated income was not associated with technological knowledge. Our study is buoyed by our strong response rate and is reflective of the demographics of the surrounding area [17]. Our findings echo concerns raised by the digital divide as it pertains to medical care. Originally described in the 1990s, the digital divide originally described the gap between those with Internet access and those without [18]. It has become clear that Internet access or connectivity is not the only player in determining the digital divide: digital literacy and skills are critical to bridging the gap [19]. Low health literacy, race, and internet accessibility have each been shown to predict patient ability to use electronic health records in their care [20-22].
Digital health literacy assessment is a nascent field [16]. Several studies demonstrated similar findings to our own and linked age, education level, and health literacy to digital health literacy [23-25]. In contrast to many of these studies, our work shows that income was not associated with digital health literacy. Although this would seem counterintuitive, income was not associated with seeking telehealth among US cancer survivors in a prior study [26]. In addition, our data comes from an older and racially or ethnically diverse population, while the prior work evaluated data obtained from younger and more homogenous groups. Finally, all previous study data were based on the random sampling of the general population and not on patients in a healthcare setting. Our study must be considered in the context of its limitations. Due to the anonymity of our study, we cannot assess whether the patients accurately responded to technological knowledge questions without the assistance of family members present during the evaluation. Additionally, our entire study cohort were patients who presented in-person to our cancer center. During the study time period, approximately 12% of our institution’s cancer volume were being seen remotely.6 Patients using remote visits may have better telemedicine literacy, thus our sample could have been skewed towards those with limited telehealth literacy. In addition, we did not use the complete ST2L questionnaire due to its length.
Therefore, we are unable to explicitly draw conclusions regarding patients’ digital literacy as it is defined in the ST2L tool. However, the knowledge gathered here will help identify those who have difficulty using and troubleshooting devices and tools required for current telemedicine applications.
SEDOH are associated with technological knowledge among a diverse group of patients with cancer. Race, education level, home internet access, and health literacy were all related to technological knowledge in our population. These results help us identify those patients who are at risk of not being adequately prepared to utilize telemedicine to receive the care they need. Reaching patients who are from disadvantaged background for remote healthcare is an ethical and moral imperative. Interventions must be developed to mitigate disparities in telemedicine use due to lack of technological knowledge and other features of digital health literacy.
We would like to acknowledge the O’Neal Comprehensive Cancer Center at the University of Alabama at Birmingham Heersink School of Medicine, the clinical site where the study was performed.
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Conceived and designed study, recruited patients: MNF, MIL, DIC, JBR, TNW, SR
Collected/analyzed data, generated figures/tables: JMPL, CS, AI, SR
Drafted manuscript: JMPL, CS, AI, SR
Edited and approved of final version of manuscript: JMPL, AI, CS, MNF, MIL, DIC, JBR, TNW, SR


