Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Soilihi Moustafa Abdou1, Ernestho-ghoud Indretsy Mahavivola2, Randriamampianina Tahianasoa3, Rajaonarison Ny Ony Narindra Lova Hasina4, Ahmad Ahmad4, Vololontiana Hanta Marie Danielle5 and Raveloson Nasolotsiry Enintsoa1
Received: April 04, 2023; Published: April 29, 2023
*Corresponding author: Ernestho-ghoud Indretsy Mahavivola, Internal Medicine Unit, Private Medical Clinic, Antananarivo, Madagascar
DOI: 10.26717/BJSTR.2023.50.007888
Introduction: Recurrent anemia, deep vein thrombosis and periodic paralysis hypokalemic have rarely been reported as a complication of Sheehan’s Syndrome. The following was an unusual case reports detailing a patient presenting with all three above presentations.
Case Presentation: The case consisted of a 51-year-old woman, admitted for deterioration of general condition, with vomiting and disorder consciousness. In her past medical history, she had experienced an abundant postpartum hemorrhage 21 years ago complicated by recurrent anemia treated with blood transfusion. She presented agalactorrhea and amenorrhea following the last delivery. Clinical examination showed Glasgow’s score 12/15, low blood pressure 80/50 mmHg, heart rate at 60 bpm, mucocutaneous pallor, painful edema of the right lower limb. The laboratory findings showed microcytic anemia 8.9 g/ dl, high level of ferritin at 1642 ng/ml (4.63-204) and transferring saturation coefficient 70% (normal 20 and 40%), hyponatremia 103 mmol/L (136-144) and hypokalemia 3 mmol/L (3.5-5), high level of serum creatine kinase 2545 (25-170IU/L). Hormonal test found anterior pituitary insufficiency with destruction of the thyrotropic, corticotropic, gonadotropic and lactotrophic axis functions. MR images of the pituitary gland showing an empty sella turcica with no visualization of the anterior pituitary, posterior pituitary and pituitary stalk. Diagnostic of Sheehan’s syndrome was finally established. In addition, she presented deep vein thrombosis of the posterior tibial vein of the right lower limb. Hydrocortisone® substitution was complicated by periodic paralysis hypokalemic (low level of kalemia 2, 4 mmol/L (3.5-5). Her weakness and hypokalemia responded well to potassium supplement.
Conclusion: From this case, panhypopituitarism should be counted among the possible causes of recurrent anemia. This anemia and secondary hemochromatosis could explain the deep vein thrombosis. Furthermore, clinicians should beware of this manifestation when administering steroids in the SS patients, especially to avoid periodic paralysis hypokalemic.
Keywords: Recurrent Anemia; Deep Vein Thrombosis; Periodic Paralysis Hypokalemic; Sheehan’s Syndrome
Sheehan’s syndrome (SS) or pituitary necrosis of the postpartum is a rare pathology and difficult to diagnose that can be life-threatening [1]. Microcytic anemia is frequently associated with iron deficiency, sideroblastic anemia, inflammatory anemia, thalassemia [2] but rarely associated with SS. Furthermore, deep vein thrombosis during SS was rarely reported. In addition, periodic paralysis hypokalemic triggered by hydrocortisone administration has never been described during SS. So, recurrent anemia, deep vein thrombosis and periodic paralysis hypokalemic have rarely been reported as a complication of SS. In this paper, we herein report an unusual case report of recurrent anemia, deep vein thrombosis and periodic paralysis hypokalemic as a complication of SS.
Figure 1 Sagittal T2 weighted (a) and T1 weighted (b), coronal T2 weighted (c) and T1 weighted (d) MR images of the pituitary gland showing an empty sella turcica (arrows) with no visualization of the anterior pituitary, posterior pituitary and pituitary stalk.
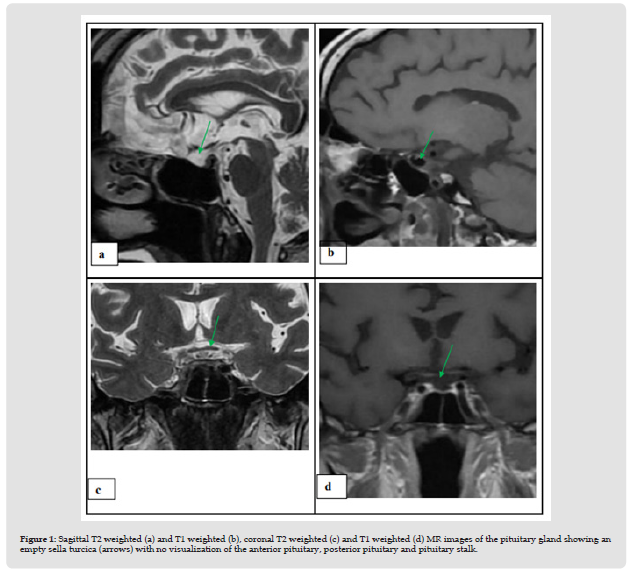
The case consisted of a 51-year-old woman, admitted for deterioration of general condition, with vomiting and disorder consciousness, without fever. In her past medical history, 21 years ago, she experienced abundant postpartum hemorrhage 3500 ml. She had unexplained anemia and recurrent blood transfusion. She had agalactorrhea and amenorrhea following her last childbirth. At admission, clinical examination showed Glasgow’s score 12/15. The exam found a status performance index 4, low blood pressure 80/50 mmHg, heart rate at 60 bpm, mucocutaneous pallor, painful edema of the right lower limb. The reminder of the clinical examination was unremarkable. The laboratory findings showed microcytic hypochromic anemia at 8.9 g/dl, mean corpuscular volume 81 (85- 95), normal white blood cells and platelets count, high level of ferritin at 1642 ng/ml (4.63-204) and transferring saturation coefficient 70% (normal 20 and 40%). Mutation of HFE gene of hemochromatosis was not performed. Another laboratory test revealed hyponatremia 103 mmol/L (136-144) and hypokalemia 3 mmol/L (3.5-5), high level of serum creatine kinase 2545 (25-170IU/L). Thyroid hormone status showed central hypothyroidism: low level of T3L 0.95 pg/ ml (1.88-3.18), low level of T4L 5.41 pmol/L (9-19.04) and normal TSH 1.37uIU/ml (0.35-4.94). The ultrasound and CT scan confirmed hypothyroidism: a pericardial effusion and thyroid hypotrophy. The other hormone tests showed adrenal insufficiency with low level of cortisol 2.5 ug/dl (3.7-19.4), a low level of estradiol 0.00 pg/ml (normal range < 10.28), a low level of prolactinemia 2.29 ng/ml (5.18-26.53), low level of FSH 2.01 mIU/ml (26.72-133.41), and LH 0.59 mIU/ml (5.16-61.99). These hormonal deficits were suggestive of anterior pituitary insufficiency. MR images of the pituitary gland (Figure 1) showing an empty sella turcica with no visualization of the anterior pituitary, posterior pituitary and pituitary stalk. This same MR images did not find hemochromatosic pituitary gland. After constellation of clinical and paraclinical signs, the diagnosis of SS complicated by panhypopituitarism (including destruction for 4 axes thyrotropic, corticotropic, gonadotropic and lactotropic), was finally established. In addition, doppler ultrasound of the lower limbs showed deep vein thrombosis of the posterior tibial vein of the right lower limb. The patient’s inflammatory and vasculitis work-up was unremarkable. Malignancy work-up was also negative. Parenteral hypertonic sodium serum® and hydrocortisone® substitution was managed. After one week, levothyrox® substitution was administered. Low molecular weight heparin was also managed, relayed by oral fluindione® . She developed flaccid paralysis and decreased tendon reflexes in both the upper and lower extremities. Her weakness of 2/5 motor power also in-volved in all four limbs, deficit of the extensor muscles of the neck with a drooping neck attitude when sitting. Sensory function and cranial nerves were spared. She was lucid with a Glasgow score of 15/15. Respiratory and ocular examination was unremarkable. The remainder of her physical examination was within normal limits. The laboratory results showed hypokalemia 2.4 mmol/L (3.5-5). Antiacetylcholine antibody and electroneuromyography were unavailable. The lumbar puncture was not done. The chest CT scan of the thymic area was normal. The dose of levothyroxine was increased to 100 ug and the dose of hydrocortisone was reduced to 25 mg. Her weakness and hypokalemia responded well to potassium supplement. The patient was followed for more than one year and there were no other new systematic symptoms.
Sheehan’s syndrome (SS) is frequently associated with panhypopituitarism complicated by rhabdomyolysis, hyponatremia [1] but rarely associated recurrent anemia and deep vein thrombosis. SS associated with panhypopituitarism is a rare but serious condition, which can be life-threatening. Our patient had severe anemia and hyponatremia, which was reversible after hormone substitution therapy with hydrocortisone® and levothyroxine® . The usual causes of microcytic anemia have been excluded. So, unexplained and recurrent microcytic anemia was unusual complication of SS. Furthermore, the infectious diseases, inflammatory and immunological causes of panhypopituitarism have been eliminated. Our study had financial limits. Genetic test for primary hemochromatosis was not unavailable. However, this patient did not present any criteria for primary hemochromatosis. Brain MRI did not detect hemochromatosic hypophisitis. So, recurrent microcytic anemia associated with SS was the main interest of this study. This seemed to indicate that recurrent anemia was the complication of SS, especially since the anemia disappeared after treatment of panhypopituitarism. Indeed, during the panhypopituitarism secondary to SS, corticosteroids should always be administered before starting other hormonal therapy. Treatment of hypothyroidism alone can trigger attack of adrenal insufficiency [3]. The causal link is defined as the very significant improvement in recurrent anemia and hyponatremia after SS treatment [1]. The SS and panhypopituitarism was difficult to diagnose, after 21 years of hemorrhage of deliverance.
A Japanese study reported a case of SS in a 68-year-old woman, with severe normochromic normocytic anemia, low erythropoietin levels, empty sella turcica and panhypopituitarism, diagnosed 48 years after hemorrhage of delivery. Erythropoietin levels normalize after hormonal therapy with hydrocortisone and levothyroxine [4]. This study is confirmed by the Gokalp et al in 2009. Patients with SS have significantly higher rates of hypochromic-microcytic anemia and iron deficiency, leukopenia, and thrombocytopenia compared to controls [5]. The same study reports that patients with SS had normochromic normocytic anemia (55%) and hypochromic-microcytic anemia (45%). This study demonstrates that anemia responds well to appropriate replacement therapy [5]. Several case studies report a case of SS with normochromic normocytic anemia. A case report in 2013 consisted of 30-year-old woman presented with SS diagnosed 6 years after a hemorrhage of delivery [6]. A study published in 2014, describes a 62-year-old woman, who has panhypopituitarism, revealed by anemia and recurrent hyponatremia [7]. Recently in 2022, the authors report a case of a 40-year-old woman, with SS, with panhypopituitarism, who presents aplastic anemia complicated by pancytopenia, with reversible normochromic anemia after hormone replacement therapy with hydrocortisone® and levothyroxine® [8]. An Italian study also describes a case of a 35-year-old woman, who also presents SS, with hypopituitarism, severe normocytic anemia and hyponatremia, reversible after hormone substitution therapy [9]. Another study reports a 45-year-old woman, who suffers from anemia secondary to SS. Panhypopituitarism has been adequately treated with hydrocortisone, thyroxine and estrogen substitution.
The hemoglobin level became normal [10]. To sum up, the relationship between SS and anemia seemed to be definitively established. In the case in discussion, SS, recurrent anemia with iron overload and deep vein thrombosis were diagnosed simultaneously. This case suggested that anemia and thrombosis were the complications of SS, especially since anemia and thrombosis disappeared after treatment. Furthermore, unusual case of thrombosis was uncommon on the SS. Therefore, the direct causes of venous thrombosis have been excluded. So, general thrombophilia was the main interest of our second discussion. Indian study reported the first case of SS associated with deep vein thrombosis. This is a 30-year-old woman, who presents an SS diagnosed 6 years after a hemorrhage of delivery, complicated by a deep vein thrombosis of the left poplitea. The only biological abnormality highlighted was normochromic normocytic anemia [11]. In their prospective study of 121 patients, Stolz et al, confirm the significant association between severe anemia and cerebral venous thrombosis [12]. A recent study in 2023, Ernestho-ghoud et al, report that relationship between anemia and thrombosis was established [13]. Other hypotheses have described in the literature. Iron overload was evoked in the arterial thrombotic risk. In 2003, chronic iron overload may contribute to increased arterial thrombosis [14]. In 2019, a randomized study also demonstrated that iron overload triggered the risk of venous thrombosis through the mechanism of blood stasis [15]. Furthermore, our patient presented periodic paralysis hypokalemic induced by hydrocortison® substitution. Hypokalemic paralysis, genetic or secondary, is present identically by muscle weakness. In literature review, the hypokalemic patient presented with paraplegia or tetraplegia [16,17].
The diagnosis was established after excluding other causes of hypokalemia [16,17]. Hypokalemic paralysis might be secondary to primary hyperaldosteronism, hyperthyroidism and drug-induced hypokaliemia [16,17] such as hydrocortisone® in our case. To return in the case in discussion, and after Asian and Western reports, SS complicated by recurrent anemia and deep vein thrombosis can also affect black patients. In our observation, SS and hypochromicmicrocytic anemia were diagnosed simultaneously. SS should be counted as a possible cause of recurrent anemia. The causal relationship between SS and anemia seemed to be definitively established. So, we wonder why about the absence of systematic research for SS during hypochromic microcytic anemia in women, especially to prevent recurrent blood transfusion and deep vein thrombosis. Furthermore, hydrocortisone substitution was responsible for reversible periodic paralysis hypokalemic, which should encourage us to use hydrocortisone be careful during SS.
Recurrent anemia, deep vein thrombosis and SS coexist in our observation. From this case, SS had to be counted as a possible cause of microcytic hypochromic anemia. Hormonal test should be performed during recurrent anemia suggestive of SS. Therefore, early diagnosis of SS would prevent hemochromatosis secondary to blood transfusion. This recurrent anemia and secondary hemochromatosis could explain the deep vein thrombosis. Moreover, the clinician had to be careful about the use of hydrocortisone during SS to avoid paralysis periodic hypokalemic.
The authors declare that they have no competing interests.
All authors contributed to project conception and critical review of manuscript. The author (s) read and approved the final manuscript.


