Impact Factor : 0.548
- NLM ID: 101723284
- OCoLC: 999826537
- LCCN: 2017202541
Almassabi Rehab*, Alamrani Bashayer and Albalawi Johara
Received: April 10, 2023; Published: April 19, 2023
*Corresponding author: Almassabi Rehab, Department of Biochemistry, Faculty of Sciences; University of Tabuk, Tabuk, Saudi Arabia
DOI: 10.26717/BJSTR.2023.49.007867
Environmental changes led to increased exposure to fungus, infectious agents, cigarette smoke, pollen grains, and other early-life and life-long risk factors for developing and exacerbating asthma and allergy illnesses globally. Climate change affects the beginning, duration, and intensity of the pollen season as well as allergies to it. Worldwide, the prevalence of allergy disorders induced by pollens is rising. Everywhere, there have been seasonal fluctuations in pollens, and both children and adults are becoming more sensitive to pollens. Understanding airborne pollen allergen trends are essential for reducing the high prevalence and negative socioeconomic effects of respiratory disorders linked to pollen around the world. The production of pro-inflammatory and immunomodulatory mediators from pollen and mold allergens might hasten the onset of IgE- mediated sensitization and allergy. Diagnosis of the component that has been resolved is really important in figuring out the complicated issue. Skin prick tests (SPT), specific IgE detection, and a complete medical history are all necessary for the diagnosis of pollen-related respiratory illnesses. The only treatment that can alter a disease’s course naturally is Allergen-Specific Immunotherapy (AIT). The Saudi Kingdom’s Vision 2030 aspires to advance the health sector’s growth and raise its standards of quality, effectiveness, and risk-avoidance measures. There are still gaps in our understanding of the underlying mechanisms and how environmental allergen exposures interact with immunological pathways to affect disease development, particularly in the Middle East, which makes it difficult to prevent pollinosis caused by airborne grass pollen exposure. The goal of the current review is to identify pollinosis caused by exposure to airborne grass pollen in subtropical regions.
Keywords: Pollen Allergy; Pollinosis; Pollen Grain; Climate Change
Abbreviations: SPT: Skin Prick Tests; AIT: Allergen-Specific Immunotherapy; IGE: Immunoglobulin E; AR: Allergic Rhinitis; MHE: Major Histocompatibility Complex; GM-CSF: Granulocyte-Macrophage Colony- Stimulating Factor; PPT: Prick-To-Prick Testing; IDT: Intradermal Test
Allergy illnesses are becoming more common everywhere due to environmental changes. Studies revealed a link between the rise in allergic diseases and increasingly modern lifestyle changes, including changes in diet, time spent indoors, use of antibiotics, and environmental exposure to air pollutants. These changes are driven by global trends of increasing urbanization and rapid population growth (Murrison, et al. [1]). Increased exposure to fungus, pathogenic agents, cigarette smoke, pollen grains, and other early-life and life-long risk factors for developing and exacerbating asthma and allergy illnesses arose from these environmental changes (Haines Ebi, et al. [2]). Climate change is one of the environmental changes, which poses a serious threat to world health and may have an impact on numerous disease-related aspects in the twenty-first century. According to earlier studies, climate change affects the onset of asthma and allergy disorders and regulates pollen generation, which causes allergic symptoms. One of the most significant effects of climate change on human health may be its effects on pollen (Choi, et al. [3]). Immunoglobulin E (IgE)-mediated sensitization and allergy can be hastened by the production of pro-inflammatory and immunomodulatory mediators from pollen. Climate change initially affects the duration and severity of pollen season as well as allergy to pollen (D’Amato, et al. [4]).
Climate and atmospheric carbon dioxide concentration have an impact on plant function. Crops, soils, insects, and diseases are all impacted by climate change in the agricultural sector. Temperature, solar radiation, water, and atmospheric carbon dioxide (CO2) concentration are the primary crucial climatic factors for crops. The rise in CO2 concentration has an impact on plant growth, resulting in longer pollination times (D’Amato, et al. [4]). Allergen transporters like pollen can be altered in the atmosphere and release allergens, resulting in allergen-containing aerosols in the ambient air, as a consequence of the effects of environmental pollutants, which serve as irritants to the skin and mucous membranes. It has been shown that pollen is an allergen carrier and that it releases highly active lipid mediators, known as pollen-associated lipid mediators, that have pro-inflammatory and immunomodulating effects in allergy disorders (Holgate, et al. [5]). Climate change may have a variety of interconnected effects on plant phenology. As a result, the subsequent modification may have an impact on the occurrence of pollen allergy. Because of how climate change would affect allergenic plant species, respiratory allergy disorders, such as asthma, allergic rhinitis, allergic conjunctivitis, and perhaps atopic dermatitis, will become more common (Choi, et al. [3]). It is clear that both allergic asthma and pollinosis have a significant negative impact on the quality of life of people with pollen allergies. These conditions harm their mental health, jeopardize their educational and professional careers due to presenteeism and absenteeism, and subsequently reduce their productivity. Since pollen allergy incidence is influenced by environmental and bioclimatic conditions that define the distribution of allergenic plants, understanding airborne pollen allergen trends is essential for reducing the high prevalence and socioeconomic impact of pollen-related respiratory diseases globally. The Saudi Kingdom’s Vision 2030 aspires to advance the health sector’s growth and raise its standards of quality, effectiveness, and risk-avoidance measures. Given that there are more and more palm trees in Saudi Arabia, it is crucial to comprehend how pollinosis caused by exposure to airborne grass pollen is affected by climate change and how to prevent it. There are still gaps in our understanding of the underlying mechanisms and how environmental allergen exposures interact with immune pathways to affect disease development, particularly in the Middle East, which makes it difficult for us to prevent pollinosis caused by exposure to airborne grass pollen. The purpose of this review is to identify pollinosis caused by exposure to airborne grass pollen in subtropical regions.
Effect of Climatic Change on Increasing Pollen Grain
Climate change is associated with changes in pollen allergens because higher CO2 levels in the atmosphere can speed up and expand plant growth, which in turn can increase pollen allergen potency and length and frequency of blooming. Additionally, increased exposure and sensitivity to subtropical grasses are the results of climate change. The species that bloom in the early spring and those that respond more favorably to warmer temperatures exhibit an earlier onset of the pollen season and its peak (Haines Ebi, et al. [2]). As a result of early flower blooming brought on by warmer temperatures brought on by climate change, more carbon dioxide is released into the sky. The intensity of airborne allergens, the amount of pollen in the air, and allergy symptoms all rise as a result of these temperature fluctuations. People who do not already have allergies may develop them if they are exposed to greater amounts of pollen and mold (Change, et al. [6]). pollen has been shown to mediate an allergy by generating highly active lipid mediators (pollen-associated lipid mediators), which have pro- inflammatory and immunomodulating effects in allergy illnesses (Holgate, et al. [7]). Changes in wind patterns can increase the long-distance transport of pollutants and pollen grains, making this transport mechanism just as important as local changes in pollen patterns, which can result in allergies that make it difficult to work, require medical attention, and increase the need for medication, all of which have a significant impact on the cost of health care (Thien, et al. [8]).
Pollen Allergy and Pollinosis
The Poaceae family is the main source of grass pollen allergies due to their widespread distribution and substantial pollenproducing capacity. The Poaceae family comprises over 12.000 wind-pollinated species, which release tremendous amounts of pollen into the atmosphere (García‐Mozo, et al. [9]). Sensitization to pollen components causes pollinosis, also known as seasonal Allergic Rhinitis (AR), pollen allergy, or hay fever. pollen allergens induce clinical symptoms after coming into contact with already-sensitized people’s conjunctiva and airway mucosa (Taketomi, et al. [10]). When the anthers release pollen at dispersion in natural pollination, the mature pollen grains dehydrate. The pollen granules quickly alter metabolically after coming in contact with a wet surface, absorbing water. Consequently, the pollen allergens are swiftly released when pollen grains penetrate the conjunctiva, nasal, or oral mucosa, which causes symptoms of pollinosis in the ocular and respiratory mucous membranes of sensitized patients (Cherrez Ojeda, et al. [11]). Inhaled pollen hydrates due to humidity in the respiratory mucosa, where sensitization typically takes place. Pollen allergens that the immune system misinterprets as potential antigens are among the proteins released by hydrated pollen, which causes an IgE-mediated hypersensitivity reaction against them (Mothes, et al., [5,12-14]), the IgE-mediated hypersensitivity reaction causes inflammation of the upper airways, a sign of seasonal allergies.
Mechanism of Sensitization
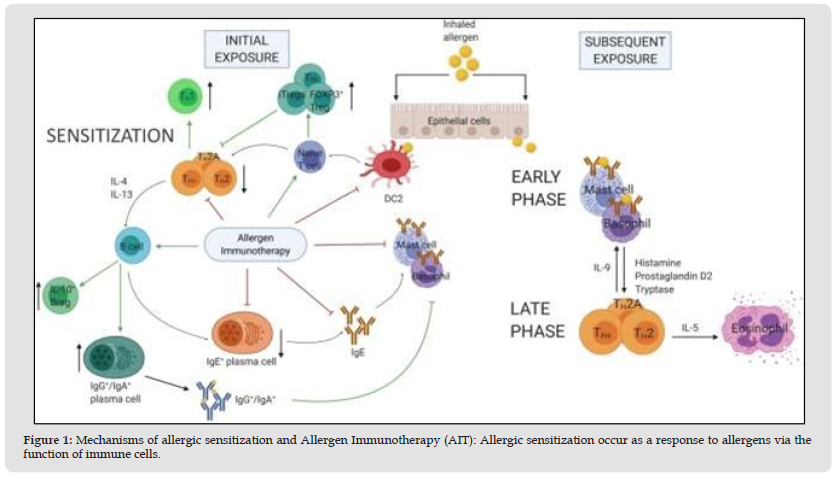
The first stage of the cascade of allergic inflammation is controlled by complicated connections between epithelial cells (ECs) and dendritic cells (DCs), which in turn triggers the early and late phase responses (Drazdauskait, et al. [15]). When an allergen enters the upper respiratory tract, antigen-presenting cells (such as dendritic cells and B cells) pick it up and convert it into a tiny peptide that binds to particular Major Histocompatibility Complex (MHC) class II molecules. Afterward, the MHC class II-peptide complex is expressed on the cell surface, where it is recognized by the Th0 receptor and other costimulatory molecules, leading to differentiation into Th2 CD41 lymphocytes that produce cytokines like IL-4, IL-5, and IL- 13, all of which are crucial for triggering various aspects of the IgE inflammatory immune response (Bernstein, et al. [16]). When IgE+ plasma cells produce IgE, which binds to high-affinity FcεRI receptors on the surface of mast cells and basophils, the phenomesnon of sensitization to the allergen takes place. Following a subsequent exposure, the allergen stimulates degranulation by forming crosslinks between nearby IgE molecules. This results in early-phase reactions (Drazdauskait, et al. [15]). Itching and sneezing are brought on by stimulation of the histamine receptors H1 and H2 on sensory neurons, but tight junctions are downregulated and vascular permeability is increased when these receptors are stimulated on ECs.
A mechanism of ongoing worsening of the allergic cascade locally produced histamine in nasal secretions of AR patients is sufficient to damage epithelial integrity in vitro. This encourages immune cell infiltration to the nasal mucosa along with cysteinyl leukotriene and prostaglandin D2-mediated chemoattraction (Drazdauskait, et al. [15]). The late-phase allergic reaction, which might appear 4 to 8 hours after the early or immediate phase reaction, is caused by these lipid mediators’ chemoattractant characteristics, which are vital for drawing inflammatory cells into the tissue (Bernstein, et al. [16]). A large influx of inflammatory cells, primarily T lymphocytes, basophils, and eosinophils, characterizes the late-phase response, which is mostly inflammatory in nature. Leukotrienes, kinins, and histamine are just a few of the mediators that these cells release, and as a result, the symptoms persist and the late phase of the disease develops (Pawankar, et al. [17]). The production and release of numerous cytokines and chemokines, including IL-4 and IL- 13 from mast cells, other cytokines like Granulocyte-Macrophage Colony-Stimulating Factor (GM-CSF), which is primarily released by epithelial cells, and IL-5 from mast cells and T lymphocytes, prolong the survival of the infiltrated eosinophils in the nasal mucosa, are crucial to the orchestration of the late phase response (Pawankar, et al. [17]) (Figure 1).
Figure 1 Mechanisms of allergic sensitization and Allergen Immunotherapy (AIT): Allergic sensitization occur as a response to allergens via the function of immune cells.
Symptoms of Pollen Allergy
Sneezing, an itchy nose, rhinorrhea, and nasal congestion are the most common symptoms induced by allergens (Averbeck, et al. [18]). The symptoms of bronchial allergic asthma that might worsen as a result of inhaled allergens include coughing, wheezing, shortness of breath, chest tightness, pain, or pressure (Damialis, et al. [19]). Acute rhinosinusitis (RS), an inflammation of the paranasal sinuses and nasal cavities, is one of the side effects of pollen allergies. The symptoms include frontal or maxillary headache, fever, and mucopurulent or bloody nasal discharge (Ebell, et al. [20]).
Diagnosis of Pollinosis
A number of skin tests are employed in the diagnosis of allergies, including
1) Skin Prick Test (SPT), which serves as the initial step in the identification of type I, immediate, IgE-mediated allergies. Prickto- Prick Testing (PPT) with native allergens is a unique variation of type I skin examinations; it is safe, has improved sensitivity, and is reasonably specific when carried out and carefully assessed.
2) Depending on the read-out time, the Intradermal Test (IDT) can assess both immediate IgE-mediated allergy and delayed-type hypersensitivity. It correlates with SPT and has high sensitivity and low specificity.
3) For cell-mediated, delayed-type hypersensitivity reactions, a patch test is used. It doesn’t matter for IgE-mediated allergies (Ansotegui, et al. [21]).
Treatment of Pollen Allergy
There are three stages of seasonal allergic rhinitis severity: mild, moderate, and severe. Sneezing and rhinorrhea types, nasal blockage types, and mixed kinds with nasal blockage as general complaints are the categories for mild and severe cases, respectively. There are suggested medications and therapy modalities for each grade. Patients with mild or sporadic seasonal allergic rhinitis should get oral antihistamines as treatment. In cases of mild illness, cromolyn can be used instead of oral antihistamines (Chaaban Corey, et al. [22]). Effective treatment for seasonal allergic rhinitis with a moderate to long duration is intranasal corticosteroids. An oral antihistamine can be used in conjunction with an intranasal corticosteroid if the patient has severe seasonal allergic rhinitis. Considerations for treating severe seasonal allergic rhinitis include using analgesics, ipratropium bromide, or oral decongestants. Immunotherapy should only be used as a last option for patients for whom other treatments have failed. Avoidance is the main therapy for chronic allergic rhinitis. Antihistamines either orally or intravenously are beneficial for treating minor or sporadic symptoms that are resistant to the release. Intranasal corticosteroids should be used to address symptoms that are moderate or persistent. If corticosteroids alone are inadequate, adding an oral antihistamine may be necessary (Beard, et al. [23]). By fostering immunological tolerance, allergen-specific immunotherapy (AIT) is thought to alter the course of allergic illness. Traditional AITs, like subcutaneous and sublingual immunotherapy, require extended treatment times and frequently result in local or systemic hypersensitivity reactions. As a result, AIT is only used as a secondline therapy for only 5% of allergy patients. In order to get over these limitations, new administration methods such as synthetic recombinant allergen preparations and intralymphatic, intradermal, and epicutaneous immunotherapies have been investigated (Hylander, et al. [24]).
Prevention from Pollen Allergy
Prophylaxis in pollen allergies is challenging due to the fact that people work in the same area and it can be difficult to completely avoid exposure to airborne pollen. The public may be advised to remain inside, keep windows and doors closed, and avoid gardening and grass-cutting during peak pollen seasons when the quantity and propagation of airborne pollen are significant in order to reduce exposure. However, some fundamental preventive measures can be taken to reduce exposure (Ravindra, et al. [25]). According to (Li, et al. [26]) study, indoor air filtration can effectively treat allergic rhinitis brought on by pollen. In order to effectively manage the disease process, it can be quite helpful to identify the environmental allergens or irritants that cause rhinitis symptoms. Most mild illnesses can be controlled with simple preventative actions. Eliminating allergens can also lessen the severity of allergic rhinitis and the requirement for medicine. Pollen, dust mites, animals, insect proteins, and fungi are the main allergens. Complete avoidance of the allergen is typically not feasible or practical, and environmental control may take weeks to months to have full positive effects (Beard, et al. [23]). The following steps can be taken to reduce exposure to dust mite allergens: get rid of carpets and soft toys; use covers for pillows and mattresses that are impermeable to allergens; vacuum beds once a week, and wash linen at 60°C. Due to a dearth of high-quality evidence, the implementation of avoidance measures is mostly reliant on consensus panel recommendations. Subpopulations of patients may react differentially to the same treatment program, as with any avoidance tactic. Age, symptom severity, seasonality, preferred medicine administration method (e.g., nasal vs. oral), adverse effects of medications, cost, the time it takes for the medication to take effect, and benefit to coexisting diseases all necessitate individualization in a patient’s treatment plan (Post, et al. [27]).
The present review discussed pollinosis caused by exposure to airborne grass pollen in subtropical climates and summarized recent studies on thes effect of environmental changes on pollen allergy. Environmental pollution, the cause of hypersensitivity and pollen allergies, and other associated issues are significantly impacted by climate change. Pollen output rises as a result and the traits that make them more allergic change as well. The production of proinflammatory and immunomodulatory mediators from pollen and mold allergens might hasten the onset of IgE- mediated sensitization and allergy. The most common symptoms induced by allergens include sneezing, an itchy nose, rhinorrhea, and nasal congestion The symptoms might worsen as a result of inhaled allergens including coughing, wheezing, shortness of breath, chest tightness, pain, or pressure, or even develop to acute rhinosinusitis. There are suggested medications and therapy modalities for each stage of seasonal allergic rhinitis. Patients with mild or sporadic seasonal allergic rhinitis should get oral antihistamines as treatment. In cases of mild illness, cromolyn can be used instead of oral antihistamines. The prevalence of allergy disorders caused by pollens is rising worldwide. There have been seasonal fluctuations in pollens everywhere, and both children and adults are becoming more sensitive to them. It is important to identify the environmental allergens or irritants that cause rhinitis symptoms in order to manage the disease process. Most mild illnesses can be controlled with simple preventative actions.


